Respiratory Disorders
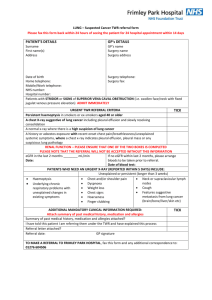
advertisement

Respiratory Stressors I Pulmonary Embolism Lung Cancer Thoracic Surgery Chest Tubes Pleural Effusions J Borrero 2/09 NUR240 Pulmonary Embolism Pulmonary Embolism -emboli that reach the lungs and obstruct pulmonary circulation -blood, air, fat, tumor cells, amniotic fluid, foreign objects -many die within 1 hr of onset of symptoms or before dx. Risk Factors for PE Virchow’s Triad of causes DVT and PE 1. Stasis of blood flow 2. Endothelial injury 3. Hypercoagulability What else???? Symptoms of a PE Chest pain with respirations S3 or S4 heart sounds EKG-non specific- T or ST abnormalities SOB-crackles, friction rub, breath sounds Dyspnea, hemoptysis, CP in<20% pts. Mild temp with sweating Shock: Tachycardia, hypotension, skin cold/clammy N&V Feeling of anxiety, impending doom, restlessness Assessment Laboratory: Elevated WBCs ABGs-Resp alkalosis Resp.acidosis. O2 Sats low CXR EKG Ventilation/Perfusion Scan CT Scan or CTA “Gold Standard” Pulmonary angiography- invasive Thoracentesis Management- Non surgical Nursing Dx: ABG analysis Prevention of DVT, prophylactic use of heparin Thrombolytic agents for massive clots O2, VS, lung/heart sounds, Mechanical ventilation Assess bleeding risk Nursing Diagnosis 1.Decreased Cardiac Output R/T … IVF Positive inotropic agents Vasodilators Outcome:Adequate tissue perfusion in all major organs Predictors: Adequate circulation Predictors: Nursing Diagnoses 2. Risk for injury (bleeding) R/T… Maintain H&H WNL Monitoring and pt. teaching 3. Anxiety R/T… Verbalization of fears Teach coping mechanisms Management Stable pts- Heparin for 5-10 days, then Coumadin started on the third day (from 3-6 weeks or indefinitely) Health Teaching Management- Surgical Embolectomy-removal of clot IVC fillter Heparin Protocol Dosage Calculations based on actual body weight. (round to nearest weight in dosing table i.e. if halfway or more to next weight round up, if less than halfway round down) 1. Heparin 25,000 units in 250 mL (100 units/mL) of ½ NS 2. Initial IV LOADING DOSE 3. Initial IV INFUSION RATE 4. WARFARIN will be started: No Yes at ________ mg P.O. daily, to start on second day of heparin. 5. LABS: CBC with platelets now & every 3 days beginning in a.m. PTT now and treat according to scale below. Pro time daily only if Warfarin started. 6. ADJUST heparin infusion based on sliding scale below: Target PTT = 71 – 123 seconds 7. MANAGEMENT *a. When two consecutive PTT's are within a 71123 range, order PTT every twenty-four hours (at least 4 hours after last PTT drawn). b. No adjustments are to be made for PTT's drawn less than 4 hours after the last heparin dose adjustment. c. Document all rate changes on MAR. Make changes as promptly as possible. 8. MONITORING a. Assess patient for bleeding every shift. b. Notify physician on rounds (STAT if unstable) if: any unscheduled interruptions in heparin infusion platelets less than 100,000/mm3 or decrease of 50,000/mm3 hemoglobin less than 10 gm/dL or decrease of 2 gm/dL significant bleeding patient suffers trauma or fall Lung Cancer Leading cancer killer for men and women Number of men has stayed stable but number of women continues to rise Lung cancer has surpassed breast cancer as the major killer of women and remains at the top of the list 70% have mets at time of dx. Long term survival is low. Most die within 1yr of dx 5 year survival rate is <15% Leading cause of cancerrelated deaths worldwide Kills more women than breast, ovarian and uterine combined Rate of lung Ca among women has not been declining as in men…but women are more likely to survive the disease No rationale offered for the difference The rate of lung Ca among non-smokers is increasing, esp. young women, reason is unclear New studies have identified some causes of increased incidence Risk Factors for Lung Cancer 85% are caused by inhalation of carcinogenic chemicals Cigarette smoke has 43 known chemical carcinogens Directly related to pack-years Second hand smoke is also a risk factor Exposure to ionizing radiation Air pollution (2-3x risk in urban areas) Chronic exposure to asbestos, coal distillates and radiation Genetic predisposition Underlying respiratory disease- COPD or TB Pathophysiology of Lung Ca Epithelial cell is attacked by carcinogen and binds to the cell’s DNA and damages it The cells mutate, have abnormal cell growth and develop into malignant cells The cells replicate and continue to change, causing the pulmonary epithelium to become an invasive carcinoma Metastasize by direst extension through blood and by invading lymph gland and vessels Lung Ca Classification 1.Small cell lung cancer (SCLC) or oat cell -2% of all lung Ca -99% associated with cigarette smoking -fast growing 2. Non small cell lung cancer (NSCLC) - has the best survival rate if tx early - includes squamous cell, adenocarcinoma and large cell cancer Assessment History Risk Factors Respiratory Assessment Presence of Abnormal findings: Inspection Palpation Percussion Auscultation Psychosocial Assessments Warning Signs Persistant cough or change in cough Change in resp pattern Hemoptysis Wheezing/dyspnea Blood streaked sputum Chest pain- dull or pleuritic Hoarseness or dysphagia Recurrent episodes of PN, Pleural effusion Compression of SVC Weight loss Clubbing of the fingers Clinical Manifestations Paraneoplastic- additional manifestation caused by hormones secreted by tumor cells 1.Endocrine Hypercalcemia Cushing’s Syndrome SIADH- Syndrome of Inappropriate Antidiuretic Hormone Ectopic Insulin- Hypoglycemia Clinical Manifestations 2. Neuromusular Peripheral neuropathy, cerebellur degeneration, seizures Myasthenia-like muscle weakness 3. Cardiovascular Thrombophlebitis Endocarditis Dysrhythmias Clinical Manifestations 4. Hematologic Anemia DIC 5. Musculoskeletal Bone pain from mets and pathological fractures Late Manifestations Fatigue Weight loss Anorexia Dysphagia N&V When to seek immediate attention: Superior Vena Cava Syndrome Spinal Cord Compression Loss of bladder/bowel tone Staging & Metastasis Staging- done at time of dx to assess size and extent of disease Staging by tumor size, location, degree of invasion of primary Tumor, Nodes and Metastasis From Stage 0 to Stage IV TNM Mets usually to long bones vertebral column liver adrenal glands brain (personality changes, in 50% of cases) Diagnostic Evaluation CXR Chest CT Scan- fine needle aspiration MRI Bronchoscopy/Thoracoscopy Sputum cytology Thoracentesis- with pleural effusion Percutaneous needle bx, lymph node bx, and bx of metastatic sites. Diagnostic Evaluation Mediastinoscopy- under general anesthesia, a scope is passed through a supra sternal incision along the trachea, visualize the mediastinum and bx lymph nodes or tumor Video Thoracosopy- endoscopic procedure for bx and to dx masses PET Scans to detect mets Management Depends on the cell type Stage of the disease Physiologic status of patient Nursing Interventions Maintain airway Administer O2 as ordered calorie/protein diet Smoking cessation Chemotherapy Used to slow tumor growth Treat patients with distant mets or small cell cancer of the lung Supplement sx or radiation therapy Not a cure and does not prolong life to a measurable degree Many side effects Choice of drug depends on the growth of the cell and the specific phase of the cell cycle that the medication affects and overall health of the patient Drugs are generally used in combination Chemotherapy Drugs * platinum analogues cisplatin (Platinol-AQ), carboplatin (Paraplatin) *taxanes- paclitaxel (Taxol), docetaxel (Taxotere) alkylating agents ifosfamide (Ifex) mitomycin (Mitomycin C) inca akloids- vinblastine sulfate doxorubicin (Adriamycin) vinorelbine (Navelbine) cyclophosphamide (Cytoxan), Methotrexate * generally first line drugs Chemotherapy Side Effects Alopecia N&V Mucositis Anemia Immunosuppression Thrombocytopenia Other Management Bronchodilators Antibiotics Pain Management Radiation therapy Radiation Therapy Curative if only local disease, palliative for mets Can be used in combo with sx and chemo to improve outcome Shrink tumor size preop Relieve superior vena cava syndrome Pt monitoring and teaching: Maintain dye marks, no lotion, no soap, no sun exposure Observe for complications- skin irritation, peeling, fatigue, nausea, taste changes, esophagitis Maintain adequate fluids Surgical Management Depends on stage of Cancer Localized (Stage I or II)-NSCLC - lobectomy - wedge resection - segmental resection - pneumonectomy - thoracotomy PNEUMONECTOMY Entire lung is removed Bronchus is severed and sutured No chest tube, fluid is allowed to collect Diaphragm is paralyzed in elevated position to prevent shift Positioning depends on physician Removal of RL is more dangerous because of larger vascular bed Surgical Management Lobectomy Segmental Wedge Thoracic Surgery Management Pre Op Baseline studies Explanation of the surgery/incision/dsg Use of chest tubes ICU/ Ventilator/O2 Teaching re: C&DB, splinting,pursed lip breathing Pain management-PCA Relieve anxiety Thoracic Surgery Management Post Op Care Impaired Gas Exchange R/T… 1. Airway Management Semi-fowler’s Suction prn C&DB Humidified O2 Use of IS Regulate fluid intake 2.Respiratory assessment Mechanical ventilation Post Op Care Ineffective Breathing Patterns Assess for respiratory complications Tension Pneumothorax Subq emphysema Pulmonary embolism Pulmonary edema Assess for CV complications Decreased Cardiac Output Cardiac dysrhythmias Hemorrhage and hemothorax Post Op Care Activity Intolerance R/T restricted arm and shoulder movement Monitor for fatigue Monitor nutrition Encourage rest alternating with activity Dangle at bedside Monitor VS Acute Pain R/T surgical incision, CT Pain management RTC IV preferable, PCA Comfort Measures- dsg, irritants, tubing, positioning Anticipatory Grieving Refer to ACS for support after dicharge Chest Drainage Opening of the chest causes some degree of pneumothorax Air and fluid that collects prevents lung expansion and gas exchange Catheters or chest tubes are inserted and attached to drainage systems Purpose:Reinflate lungs and remove collections of fluid or air from the pleural space due to a pneumothorax, hemothorax or pleural effusion Chest Drainage System is usually 3 bottle/chamber system New systems allow for dry suction (water seal). Preset at -20cm H20 Heimlich valve- is a one way flutter valve made of rubber tubing in a plastic chamber. Chest Drainage Water in the second chamber acts as a seal and allows air and fluid to drain from the chest into the first chamber but cannot reenter the chest tube Think of a cup of water and a straw. If you blow bubbles into a submerged straw, air would bubble out through the water. Now if you wanted to draw back air through the straw, you would only draw water Drainage accumulates in the first chamber and air exits through the second chamber. The first chamber remains empty in case of pneumothorax Chest Drainage The water level fluctuates as the pt breathes (tidaling) Up on inhalation Down on exhalation Outside suction may be added to promote drainage of fluid and removal of air Addition of suction creates constant bubbling in 3rd chamber If bubbling occurs in the absence of suction there may be a leak in the system Nursing Care Assess patency of CT/ Pleurovac Keep 2 padded clamps and bottle of sterile H2O at bedside Vaseline and sterile gauze Assess amt/type of chest drainage q1h 1st 24hrs. Notify MD >100/hr Assess respiratory status Assessment of Water Seal Function Fluctuation of fluid in water seal compartment during respiration is normal If tidaling does not occur- observe for bubbling, possible leak Rapid bubbling in absence of leakEMERGENCY-notify MD May have loss of air from incision or tear in pleura Care of the Chest Tube and Drainage System System kept below the insertion site If postitioning pt on affected side, check for kinks & occluded tubing Tape all connections securely with adhesive tape Coil tube at pts side Monitor tension on tubing when pt sits up or turns over If unit accidentally tips over, stand it up right away If drainage has moved from the collection chamber, replace unit Change dsg prn, monitor insertion site Documentation Duration and Removal of CT Duration of CT is dependent upon CXR Normal Resp Status Drainage <100ml/24 hr Place occlusive dsg over insertion site Monitor pt CXR Change dsg prn Chest Tube Complications Dislodged Tube from Chest Wall 1.Apply pressure over insertion site 2.Notify MD 3.Have pt cough forcefully and cover wound with vaseline gauze and DSD 4.Tape on 3 sides only 5.Stay with pt and assess for resp distress 6.Prepare for CT reinsertion 7.If S&S of tension pneumo/mediastinal shift are present, release dsg to let air escape Interventions for Emergency Situations Disconnected Chest Tubes- check agency policy Clean both ends with alcohol and allow to dry Reconnect and tape Assess continuously for resp distress Anticipate a STAT portable CXR Interventions for Emergency Situations Tension Pneumothorax Assess for resp distress, tracheal shift, diminished to absent breath sounds, assymetrical breathing, hypotension, pain Assure system is patent, not clamped or obstructed Notify MD STAT and increase O2 Prepare for needle thoracostomy (14G ) Stay with pt and assess continuously Place in hi fowler’s if not contraindicated Prepare for ABG and/or CXR Interventions for Emergency Situations Disconnection from drainage system Submerge open end of the chest tube in sterile water Prepare new equipment and attach, use adhesive tape Wipe ends with alcohol and allow to dry Chest tube becomes obstructed by clot Observe tubing for signs of clot, decreased flow of fluid through tube Gentle milking of tube, do not strip Pleuritis Inflammation of the pleura generally 2nd to viral respiratory illness, pneumonia or rib injury. Self limiting and short duration Pain unilateral and localized, sharp or stabbing, may refer to neck or shoulder Dx: based on presenting symptoms. CXR and EKG to r/o other problems Tx: Analgesics and NSAIDS. Codeine for pain and to suppress cough Report increased fever, productive cough, dyspnea or SOB Pleural Effusions Excess fluid in pleural space Systemic Causes: CHF, liver or renal disease, connective tissue disorders RA and SLE Local Causes: PN, atelectasis, TB, lung CA and trauma Pleural Effusions The accumulated fluid can be transudate or exudate: Transudate: protein free fluid forced from lung by increased (overload) pressures in the lung “weeps out” Heart failure, ascites from liver failure, renal disease, PN Exudate: contains cells > 3% proteins Inflammation, infection, malignancy in pleural space, TB, pancreatitis, subphrenic abscess, empyema Pleural Effusions Symptoms- dyspnea, pleuritic CP Diagnosis- diminished BS, dullness over effusion CXR/CT/Ultrasound- to differentiate, localize pleural effusions Thoracentesis- analysis of pleural fluid Fluid removal is limited to 1200-1500cc to prevent cardiovascular collapse, relieve symptoms -may be diagnostic, cells are sent for cultures -done under radiology or ultrasound Pleural Effusions Chemical Pleurodesis- tx to prevent recurrence of pleural effusions A sclerosing agent is instilled. Creates an inflammation that causes adhesions between the pleura layers so no fluid can accumulate there. Pleural Effusions Treat the underlying cause- antibiotics, thoracotomy Pt teaching re the recurrence of symptoms and control of systemic causes NCLEX TIME While assisting a client in changing positions, the chest tube is pulled from the client's chest. What should the nurse do first? A.Check breath sounds. B.Place the end of the chest tube in a cup of water. C.Place the client in a reverse Trendelenburg position. D.Cover the opening in the chest with a dressing. NCLEX TIME Which of the following findings in the client after lung reduction surgery would require an immediate intervention? A.Pain on inspiration B.Decreased cough C.Absence of breath sounds D.Drainage from operative site NCLEX TIME The nurse teaches the client being discharged after pneumonectomy to: A.Always sleep with the operative side down. B.Take temperature daily to monitor for signs of infection. C.Avoid using arm on affected side. D.Perform deep breathing exercises with the operative side up NCLEX TIME The nurse assesses the client receiving chronic oral steroids for which of the following complications? A.Weight loss B.Renal calculi C.Hyperglycemia D.Tachycardia NCLEX TIME In teaching the client about radiation therapy for lung cancer, the nurse explains that side effects may include: A.Weight gain B.Dyspnea C.Oral bleeding D.Taste changes NCLEX TIME The registered nurse is caring for a client with lung cancer who has just been admitted to the ICU after having a pneumonectomy. The client is intubated and being ventilated with a positive pressure ventilator. All of the following orders are received. Which one will the nurse implement first? A.Morphine sulfate 6 to 10 mg IV for pain B.Continuous pulse oximetry to keep O2 saturation at 92% to 100% C.Ceftriaxone (Rocephin) 500 mg IV every 6 hours D.Infusion of one unit packed red blood cells over 2 hours NCLEX TIME The RN and nursing assistant are working together to provide care for a group of clients. Which of these nursing activities could the RN delegate to the nursing assistant? A.Monitor the effectiveness of oxygen therapy for a client admitted with chronic bronchitis. B.Reinforce the use of slow expiration through pursed lips to maximize gas exchange for a client with sarcoidosis. C.Auscultate for improvement in breath sounds in a client who has had a right upper lobectomy. D.Document discharge instructions for a client being discharged with new medication prescriptions. NCLEX TIME The nurse identifies which of the following as risk factors for development of pulmonary emboli? (Choose all that apply.) A.Delayed wound healing B.Immobility C.Renal stones D.Thrombocytopenia E.Obesity F.Lung cancer