Elbow examination
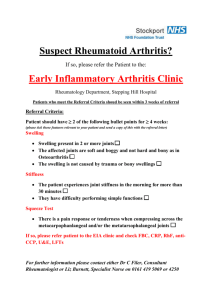
advertisement

WEEK 18: Locomotor system – History
Screening Questions:
1. Do you have any pain or stiffness in your muscles, joints or back?
2. Can you dress yourself completely without difficulty?
3. Can you walk up and down stairs without any difficulty?
If no to all three questions then it is unlikely the pt suffers a musculoskeletal problem. If yes to one question, take a
more detailed history.
Main aim = differentiate between inflammatory and degenerative/mechanical problems, and to assess impact on pt.
Does the problem arise in a joint?
Evolution of the problem – acute or chronic?
Current symptoms – inflammatory or non-inflammatory?
Pattern of affected joints
Involvement of other systems – inflammatory arthropathies often affect other systems – skin, eyes, lungs,
kidneys, as well as systemic symptoms eg malaise, weight loss, fever, night sweats, fatigue, depression
whereas OA is limited to the musculoskeletal system
Impact of condition on pt’s life
Presenting Complaint
Rationale
Pain – SOCRATES +
mechanism of injury
Site: How many joints? Which was the first joint or joints affected? Which were
subsequently affected? Is it bi-lateral, symmetrical or asymmetrical (most affected joint or
joints)? Pain may be localised to a joint or a number of joints; it can be localised to a
tendon, like in tendosynovitis (localised inflammation of a tendon sheath) or it can be diffuse
and spread over a wide area.
Does the pain
originate from a joint
(arthralgia), muscle
(myalgia) or other
soft tissue?
Pain is often at the site of inflammation or may be referred to sites well away from site of
pathology (somatic referral).Eg pain in left shoulder: ? pain from diaphragm or ischaemic
cardiac pain
Onset:Was onset triggered by an event – trauma or infection?
RA/Gout/trauma: acute/immediate, Joint sepsis: sub-acute (over 1-2days), OA: chronic = >3
months
Character:
Pain due to mechanical nerve compression = ‘shooting’; eg sciatica = buttockpain
that shoots down the leg, caused by IV disc protrusion/prolapse
Bone pain is deep or boring (and worse at night).
Fracture pain is sharp and stabbing; aggrevated by use and relieved by rest
Partial muscle tears may be painful; total tears may be pain-free
Pain due to OA = aching with sharp stabs associated with certain movements or in certain
positions; pts have ‘good’ and ‘bad’ days. Local pain = tumour, infection (osteomyelitis),
avascular necrosis, osteoid osteoma (benign bone tumour). Diffuse pain = osteomalacia
Associated symptoms: Fatigue (+++ in inflammatory), malaise, depression.
Stiffness and/or swelling of joints, erythema around joint (did this happen immediately?),
crepitus.
Rashes/psoriasis(autoimuune condition; may lead to psoriatic arthritis and inflamm
joints), fever, abdominal symptoms, weight loss (malignancy can confuse diagnosis).
Dry mouth & gritty eyes (sero –vearthropathies).
Vascular and/or neurological complications.
Does it affect sleeping pattern? Suggests chronic pain
Time: frequency, regularity & duration of episodes
Pain in the inflammatory arthropathies is often present all the time, both at rest and with
movement and is often worst in the mornings. OA pain is often worse on movement of the
involved joint and may be felt at rest when the limb is placed in certain positions.
Exacerbating and relieving factors:
Inflammatory: RA: pain at rest; worse in morning; stiffness eased with movement; helped a
lot by NSAIDs; tends to be more unpredictable pain with flare ups
Non-inflammatory(mechanical): OA: painful on activity/with movement; ease with rest
Severe bone pain is unremitting and persists through the night disturbing sleep.
Dorsal root compression caused by narrowing of the spinal canal which may cause pain in
the buttocks and legs on walking, is exacerbated by extension of the spine as when walking
downhill – extension of the spine narrows the canal further. Bending forward relieves the
pain because the spinal canal is opened up.
Generalized causes of arthralgia (joint pain)
Infective
o Viral, e.g. rubella, mumps, hepatitis B
o Bacterial, e.g. staphylococci, tuberculosis, Borrelia
o Fungal
Post-infective
o Rheumatic fever, reactive arthritis
Inflammatory: pain at rest and movement, worse in am, stiffness eases with movement/hot water
o May have infective or non-infective cause
o RA, systemic lupus erythematosus (SLE), ankylosing spondylitis, systemic sclerosis
Degenerative/non-inflamm: painful with activity, in pm, less painful with rest
o Osteoarthritis
Tumour – may have an inflammatory-like presentation if fast growing
o Primary, e.g. osteosarcoma, chondrosarcoma
o Metastatic, e.g. from lung, breast, prostate
o Systemic tumour effects, e.g. hypertrophic pulmonary osteoarthropathy
Crystal formation
Note that ‘reactive arthritis’ = Reiter’s syndrome;
o Gout, pseudogout
arthritis of small joints of hand and…skin and nail
Trauma, e.g. road traffic accidents
changes similar to that of psoriasis, and conjunctivitis,
Others
iritis, circinate balanitis (painless superficial ulcers on the
o Fibromyalgia syndrome
prepuce and glans), cervicitis, urethritis and superficial
o Sjögren's syndrome
mouth ulcers, synovitis in knees and hips, dactylitis (of
o Hypermobility syndromes
feet), plantar fasciitis
Localized
Trauma, e.g. sports injuries
Tendonitis, e.g. shoulder rotator cuff lesions, Achilles tendonitis
Enthesopathies, e.g. tennis elbow, golfer's elbow
Bursitis, e.g. trochanteric bursitis
Nerve entrapment, e.g. carpal tunnel syndrome
Referred pain:
Cervical:
o C1/2: occiput; C3, 4: interscapula region; C5: tip of shoulder, upper outer aspect of arm; C6, 7: interscapular
region or the radial fingers and thumb; C8: ulnar side of forearm, ring and little finger
Thoracic spine pain perceived at the chest
Lumbar spine perceived at the buttocks, knees and legs
Pain from acromiclavicular joint localises to the shoulder
Pain from glenohumeral joint or rotator cuff muscles localises to lateral aspect of upper arm
Elbow pain perceived at the forearm
Hip pain perceived at the anterior thigh or knee
Pain from the knee may be felt in the knee, hip or ankle.
Pain due to irritation of a nerve will be felt in the distribution of that nerve.
Stiffness
Muscle pain is
usually described as
stiffness
Clarify what the pt means – ‘how long does it take to get going?’:
difficulty initiating movement,
difficulty carrying out certain movements but with normal range
discomfort associated with movement of a particular joint or group of joints
restricted range of movement
Inflammatory presentation:Severe morning stiffness which goes on for some hours is
typical of rheumatoid arthritis. Patients may have great difficulty getting out of bed and
generally getting going in the mornings with RA.RA may also be diurnal and be painful at
night too.
Non-inflammatory, mechanical presentation:OA may cause stiffness for <30mins, if rest
and try moving again stiffness only lasts a few mins, pain on movement too.
If stiffness predominates over pain, suspect soft tissue contracture or spasticity (increasing
muscle contraction in response to stretch) or tetany (involuntary sustained contraction) and
check for increased tone associated with an UMN lesion.
Stiffness related to soft tissues rather than joint itself:
Polymyalgia rheumatic: affects shoulder and pelvic areas mainly
Inflammation of tendon insertion sites (enthesopathies): golfer’s and tennis elbow
Calcific tendonitis: supraspinatus tendonitis
Bursitis: trochanteric bursitis
Swelling
May be diffuse
oedema or localised
as a discrete
collection in a joint,
bursa or tendon
sheath
Erythema and
warmth
Weakness
Locking
Triggering
Deformity
Joints affected over
course of disease
Recurrent inflammatory episodes may lead to joint subluxation or dislocation or fixity of
the joint in a so called ‘fixed deformity’ leading to total loss of function and to resulting
disability. For example: arthritis of the proximal interphalangeal joint of the index finger
may result in reduction of movement in that joint or some fixity of the joint. The patient
may find it difficult to do up the shirt buttons or he/she may no longer be able to play a
musical instrument.
Identify site, localisation, extent and time course
Swelling in the absence of trauma is suggestive but not pathognomonic of
inflammation/inflammatory disease process. It is important to be aware that pain or
sensory disturbance may give rise to the sensation of swelling without actual swelling
being present.
Check if swelling is red and warm(co-existing infection)
Nodal OA causes bony, hard and non-tender swellings in the PIPS and DIPS.
Ankle swelling is more often due to oedema than to swelling of the joint.
When vascular structure (bone, ligaments) damaged: rapid swelling within mins due to
bleeding into the joint.
If avascular structures (menisci-torn, articular cartilage-abraded): a reactive effusion
hours-days cause joint swelling.
Acute inflammation = infection; common in infective, traumatic and crystal-induced
conditions, not so in RA or SLE.
Problem may be secondary to pain
Proximal weakness: primary muscle disease eg immune-mediated inflammatory disease
(dermatomyositis) or non-inflammatory myopathy (2nd to chronic alcohol use, steroid
therapy or thyrotoxicosis)
Distal weakness: commonly neurological eg peripheral neuropathy of thiamine or B12
deficiency, connective tissue disorders or hereditary sensory motor neuropathy
(Charcot-Marie-Tooth disease)
Intermittent weakness: if worsens during activity => myasthenia gravis; if slowly
progressive = motor neurone disease
Sudden onset: eg wrist or foot drop indicate a mononeuritis multiplex associated with
RA, vasculitis or connective tissue disease, DM or HIV infection.
Incomplete range of movement at a joint due to an anatomical block(loose body, torn
meniscus). True locking is due to mechanical obstruction. Pseudo-locking is loss of ROM
due to pain (egpts with patellofemoral pain will not flex leg)
Finger movement of flexion to extension – blocked in extension which then ‘gives’ suddenly.
Results from nodular thickening or fibrous thickening of the flexor fibrous sheath. Adults:
ring, middle fingers. Congenital: thumb
Acute deformity may be due to fracture, dislocation or swelling (haemarthrosis or
intramuscular haematoma). Malopposition of the joint surfaces may be partial (subluxation)
or complete (dislocation). Establish if joint deformity is fixed or mobile, and if mobile,
whether it is passively correctable.
Mono articular = only 1 joint – usually but not exclusively a feature of degenerative
disease, usually DIP or PIP and/or first CMC joint
Nodules or lumps
Red/ dry eyes
Fever, Rash, ulcers
Loss of function
Oligo articular2-4 joints– Is usually a feature of reactive arthritis, Reiters syndrome usually
asymmetrical large joints or dactylitis (sausage digit).
Poly articular = >4 joints – Usually but again not exclusively a feature of inflammatory
disease, usually MCP, PIP and MTP joints
Axial – affects the spine
Also consider: large or small joints involved?; is the pattern symmetrical or not?
RA = polyarthritis, symmetrical; note that early RA may affect any pattern of joints.
Seronegativearthrotides (-ve for rheumatoid factor) eg psoriatic arthritis = more likely to be
asymmetrical
OA = weight-bearing joints and parts of the spine that move the most (lumbar and cervical)
Predominant involvement of the small joints of the hands, feet or wrists suggests an
inflammatory arthritis, e.g. RA or SLE. Medium or large joint swelling is more likely to be
degenerative or a seronegative arthritis, e.g. OA, psoriatic arthritis or ankylosing spondylitis.
Nodal osteoarthritis has a predilection for the distal interphalangeal joints and
carpometacarpal joint of the thumb.
‘Outer herbedes’ Heberdens nodes – Small bony nodules typically found at dorsum of DIP
joint and associated with OA
Bouchards nodes – Small bony nodules typically found at dorsum of PIP joint and
associated with OA
Rheumatoid nodules – Fleshy, firm and non-tender typically found at extensor surface of the
knuckles; may also occur at sites of pressure or friction (sacrum)
Gouty tophi = white, firm, irregular subcutaneous collections of monosodium urate crystals
in people with longstanding high levels of uric acid in the blood; sites = helix of ear, extensor
aspect of fingers, hands and toes. Overlying skin may ulcerate, discharging crystals and
become infected.
Commonly conjunctivitis and anterior uveitis (=iritis) are found Reiters syndrome and
ankylosing spondylitis. Episcleritis is found in SLE and RA. Scleritis is found in RA.
Reduced tear production (dry eyes; keratoonjunctivitis sicca) found in Sjogren’s syndrome,
RA and SLE.
SLE and septic arthritis
Gives an indication as the progression of disease.
Past Medical History
Complaint
Infection
Trauma
Diagnosed muscular
skeletal disorders
Auto immune disease
Previous operations
Rationale
Particularly relevant in Septic arthritis and may give rise to a relapse in SLE
OA often develops at the site of trauma around joints; previous dislocations?
SLE is prone to relapse and remission. Don’t miss the obvious- a diagnosis of some type of
arthritis may have already have been made.
RA and SLE are auto immune diseases
Generic information needed for all PMH; presence of liver disease will mean many diseasemodifying drugs of arthritis can not be used.
Similar symptoms, long term conditions that you see the GP for, hospital stays, surgery, previous diagnoses?
DM, steroids, IHD, stroke and obesity = co-morbid factors
Felty's syndrome
Rheumatoid arthritis with splenomegaly, lymphadenopathy and neutropenia
Sjögren's syndrome
Arthritis with 'dry eyes' (keratoconjunctivitissicca), xerostomia (reduced or absent saliva production), salivary gland
enlargement and Raynaud's phenomenon
Enteropathic arthritis
Associated with inflammatory bowel disease - ulcerative colitis and Crohn's disease
Psoriatic arthritis
With skin and nail features of psoriasis
Haemophilia
Associated with (especially knee) arthropathy because of recurrent haemarthroses
Sickle cell disease
Associated with osteonecrosis of the hip due to bone infarction
Still's disease
Juvenile idiopathic arthritis
Reactive arthritis
Urethritis, conjunctivitis and inflammatory oligoarthropathy about 1-3 weeks after sexually transmitted chlamydial
infection or infective gastroenteritis
Drug History
Allergies – a poly arthritis could be the result of an allergic reaction
Current and previous medications: did it work, any side effects and why was it stopped or changed?
Drugs for any other conditions; OTC medications
Drug
Diuretics
Steroids
Statins
ACE-I
Antiepilepics
Immunosuppressants
Quinolones
Possible adverse effect
Gouty arthritis
Osteoporosis, myopathy, avascular necrosis, infections (think! Cushing syndrome)
Myalgia, myositis, myopathy
Myalgia, arthralgia,
Osteomalacia, arthralgia
Infections
Tendonopathy, tendon rupture
Social History
History
Smoking
Alcohol
Diet
Domestic circumstance
What can and can’t do
Functional independence
Effect on life/ mental state
Rationale
Lung cancer with bony mets; hypertrophic pulmonary osteoarthropathy
Trauma, myopathy, rhabdomyolysis, nerve palsies
Vit D = osteomalacia/rickets; vit C = scurvy; anorexia nervosa = osteoporosis
Lives alone/ with family
Does pain/ loss of movement effect them in their activities of daily living(ADL); hold pens,
dress themselves, use cutlery; washing, dressing, toileting, stairs, cooking, shopping
Incorporates body image- may be altered. Does immobility impede ability to interact
socially
Occupation
Ask for current and previous. Does occupation effect disease e.g. repetitive strain on
individual joints may be a catalyst for O.A. Disease/ illness may also affect the patient’s
ability to work. Time off? RSI, hand vibration syndrome and fatigue fractures – litigation?
Army recruits, dancers and athletes = fatigue fractures
Age
Age related factors may be applied to all the above e.g. inability to work may be more of
an issue in a younger patient and altered body image may be again more of an issue.
Use this as a rough guide and try not to make sweeping assumptions
FIFE, work, home, stairs, wheelchair, living conditions, sports and aspirations?
Functional loss => limitation in an activity => restriction on participation in life’s activities
Family History
RA; OA; Gout; Back disease; Psoriasis; Ulcerative Colitis or Crohn’s Disease.
Muscular dystrophies: Duchenne, Becker, dystrophiamyotonica, limb girdle
Erlos-Danlos syndrome, Dupytrene’s contracture
Osteomalacia = more common in Asians (due to less sunlight exposure and vit D); sickle cell disease may present as
joint pain in Africans; bone and joint TB may present in Africans and Asians.
Sexual History
May be relevant in reactive arthritis, gonococcal arthritis and hepatitis B.
Give 3 examples of drugs used in locomotor disorders:
analgesics
anti-inflammatory agents
disease-modifying drugs for rheumatoid arthritis
List 4 risk factors for locomotor disorders (if necessary indicating for which condition risk applies):
1
2
3
4
WEEK 19: Locomotor system – Examination
GALS Screen: ask questions, if yes to them then proceed with GALS assessment
Should ask the patient 3 questions before commencing the assessment –
1) Do you have any pain or stiffness in your muscles, joints or back?
2) Can you dress yourself completely without any difficulty?
3) Can you walk up and down the stairs without any difficulty? Mobility aids?
(Obesity(raised BMI)?)
Assess active movements before passive movements
GALS = a brief screening examination which should take 1-2 mins; do tasks when pt standing up first, then ask
them to move to the couch.
Ask pt to undress to their underwear and stand in front of you
Gait: causes: limping, stiffness of movement, asymmetry, walking aids, difficulty with standing up from sitting
grey = spine assessment but easier to do when pt standing already
Observe Gait
Ask the patient to walk a few steps away from you, turn and walk back. Observe for:
Symmetry
Smoothness
Ability to turn quickly(unsteady?)
Observe patient in the
anatomical position,
observe from behind,
from the side and from
the front for:
Bulk (swelling, deformity) and symmetry of the shoulder, gluteal, quads and calf muscles
Inspect spine from
behind(undressed)
Inspect thoracic
spine from
side(undressed)
Assess lumbar spine
movement
Scoliosis, muscle bulk, symmetry of legs and trunk. Asymmetry of sacroiliac joints/ iliac
crests (diff leg length), swelling of gluteal, hamstrings, calves
Normal cervical lordosis, thoracic kyphosis, lumbar lordosis and evidence of knee flexion or
hyperextension.
Lateral lumbar flexion
Ability to fully extend elbows and knees
Popliteal swellings
Foot abnormality
Ask the patient to bend down to touch their toes – good for functional assessment i.e. can
they dress themselves.
As this can be achieved by good hip flexion, it is important to palpate for normal
movement of the vertebrae too. Place 2 fingers on the lumbar vertebrae – the fingers
should move apart as the patient flexes forwards and come back together as they
straighten up.
Ask pt to slide hand down leg
Arms stand in front of the pt
Gently press
supraspinatus
Hands behind head
Hands behind the back
Shoulders, elbows,
wrists
Observe back of hands
and wrists
Observe Palms
Detect hyperalgesia
Tests abduction and external rotation of GHJ, and elbow flexion (often first movements
affected by shoulder problems)
Tests adduction and internal rotation of the shoulder
Flexion and extension (do wrists by prayer sign, and reverse prayer sign!)
Ask patient to bring their elbows into their side with palms facing downwards (pronation).
Observe backs of hands for joint swelling, deformity and scars.
Ask pt to turn hands over (supination) observe for muscle bulk or abnormality
Assess power grip and
strength
Assess fine precision
pinch
Squeeze MCPs
Ask the pt to make a fist, and open hands (tests ROM of fingers first). Then assess grip by
asking the patient to grip your fingers.
Ask them to pinch each finger in turn with their thumb – assesses joint movement, co –
ordination
Squeeze across the MCP joint and assess for tenderness suggesting inflammatory joint
disease (RA) – watch patients face for signs of pain
Legs ask pt to lie on the couch supine
Assess full flexion and
extension
With patient on couch ask the patient to extend and flex both knees feeling for crepitus
Assess internal rotation
of the hips
Abduction/adduction
Feet movements
Temperature
With hip and knee flexed at 90º, holding knee and ankle to guide the movement, rotate
assess internal rotation of each hip in flexion
Ask pt to abduct/adduct leg
Ask pt to dorsiflex and plantar flex foot and move toes.
Of knee = ?inflammation
Perform Patella tap
Perform patella tap - looking for knee effusion; slide hand down thigh to compress the
suprapateller pouch, forcing any effusion posterior to patellar. +ve = pattelar bounces
From end of couch assess the feet for swelling, deformity or callosities on the soles of the
feet (suggest abnormal loading)
Squeeze the MTP joints for inflammatory joint disease – watch the face for signs of pain
Inspect feet
Squeeze MTPs
Straight leg raise
Only if pt complains of symptoms indicative of sciatica; pt is supine - take the leg by the
heel and raise it (leg has to remain straight with the knee fully extended). In the normal
person you should be able to raise the leg to a right angle position. In a patient with nerve
root compression symptoms, straight leg raising will be very restricted – (record the angle).
Spine ask pt to sit on couch with legs hanging off
Palpate down the spine, looking for any signs of tenderness.
Assess lateral flexion of
the cervical spine
Assess rotation of the
cervical spine
Assess temporal
mandibular joints.
Assess thoracic spine
movement
Ask the patient to tilt their head to touch their ears to their shoulders
Ask the patient to touch the tip of the shoulder with the chin
Ask patient to open mouth wide and then move lower jaw from side to side.
Arms crossed, pelvis fixed, ask pt to turn left and right (thoracolumbar rotation)
Recording GAIT:
If –vefinding, put a cross and describe finding below.
Regional Examination of the Musculoskeletal System (REMS)
Basic Principles:
1. Introduce yourself
2. Look: - Pain, asymmetry, deformity, stiffness (Active Range of Movement).
3. Feel: - Heat, swelling, crepitus, asymmetry, deformity.
4. Move: - Passive Range of Movement, (ROM) may be measured with a goniometer.
5. Assess function of the joint
Hand examination
Have the patient sitting with their hands palm down on a pillow.
LookLooks at BOTH hands with palms
facing down
Nails.
Fingers.
Wrist.
Palm
Skin
Swelling
Muscle Bulk
Turn hands over – palms up
Muscle wasting on thenar/hypothenar
eminences?
Feel
With hands palm up
Peripheral pulses
Bulk of the thenear and hypothenar
eminences for tendon thickening
Assess median and ulnar nerve sensation
With hands palm down
Assess radial nerve
Temperature
Tenderness
Is there swelling? If so; is it bony or soft
tissue?
Compare both sides for symmetry, deformity, muscle wasting and
scars; do the changes mainly involve the small joints – DIPS, PIPS and
MCPS, or the wrists?
Vasculitic changes(urticaria, purpura, nodules), nailfoldvasculitis,
splinter haemorrhages(Endocarditis), thimble pitting(psoriasis),
onycholysis(psoriasis), clubbing(Hypertrophic pulmonary
osteoarthropathy)
Inflammation, Scars: - Joint replacements (most commonly the MCP’s).
Nodular deformities(inflam) of the PIP’s – Bouchard’s Nodes (OA).
Nodular deformities(inflam) of the DIP’s- Heberden’s Nodes (OA).
Swan necking (RA) Boutonniere’s = (PIPflexion with
DIPhyperextension) (RA) Z deformity of the thumb (RA).
Squaring of the hand due to swelling of CMC joints(metacarpal comes
out) (OA).
Gouty tophi
Scars: dorsal scars of arthrodesis for pain (this results in loss of function
so don’t flex the wrist during the exam).
Rashes (often aggrevated by exposure to light; common in vasculitis eg
SLE) and erythema, Skin tightening of scleroderma (thickening of skin),
muscle wasting, Ulnar deviation.
Rashes(psoriasis); erythema(RA), wasting, scars (Carpal Tunnel
release; mid-line and hard to see), Dupytren’s contracture (general);
muscle wasting(RA)
Thinning, Bruising(long-term steroid use), Rashes(purpura), erythema
Looks for generalised and focal swelling of DIP, PIP, MCP, CMC joints;
Decreased dorsal muscle bulk in RA common
Can the pt do this or is the a problem with the radioulnar joint?
If only thenar, then pt may have carpal tunnel syndrome; look for a
carpal tunnel release/decompression scar too.
(Ask if there is any pain, tenderness or parasthesia!)
Gently touch over both thenar and hypothenar eminences, and index
and little fingers. Is sensation symmetrical?
Gently touch over the thumb and index finger web space
Assess temp over forearm, wrist and MCP joints. Any differences?
Inflammation of joints is often associated with warmth of the overlying
skin. (Run the back of the hand over the joint and compare the skin
temperature with the opposite joint and / or with the surrounding skin).
Gently squeeze across MCPJ; watch the pt’s face for discomfort.
Most tender spot?
Is tenderness within or outside the joints?
Is it focal or generalised?
Bimanually palpate any MCPJ, DIPS or PIPS that appear swollen or
painful. Is there evidence of active synovitis? Synovitis = warmth,
swelling and tenderness triad over joints
Previous synovitis evidence = thickened, rubbery but non-tender joints.
Is it hard or bony(OA)/soft(combination of synovial hypertrophy and
synovial effusion)/spongy/fluctuant?
Assess for fluctuance and mobility: OA = hard and bony; RA = soft and
rubbery
For discreet swellings note – site, size, shape, contour, consistency,
colour, tenderness, attachment to surrounding structures.
Check for squaring of the carpometacarpal joint of the thumb.
Check for Heberden’s (DIPS) and Bouchard’s (PIPS) nodes.
In possible tumours look also for evidence of raised lymph nodes
Compare with opposite limb to decide if joints are normal.
DIPs, PIPs, MCPs and wrists using the two
thumbs. There should be crevices on both
sides.
Bimanually palpate the pt’s wrists.
Run your hand up the pt’s arm along the
ulnar border to the elbow
Move (active and passive [crepitus?]).
Ask pt to straighten fingers fully against
gravity
Can they make a fist?
Wrists
If history/examination suggest carpal
tunnel syndrome…
Assess median and ulnar nerves for power
Feels for crepitus during passive
movements
Limitation with pain
Instability
Function: Ask pt to grip two of your fingers
Ask pt to pinch your finger
Ask pt to pick up a small object like a coin
out of your hand.
These are lost in early inflammation.
Feel and look for rheumatoid nodules or psoriatic plaques on the
extensor surfaces
Active = pt moves it; passive = I move it; if loss of active movement but
passive intact, suggests problem with the muscles, tendons or nerves
rather than in the joints
If unable to do so it may indicate joint disease, extensor rupture or
neurological damage – assess this by moving fingers passively.
If they can then they can move all their joints.
If they can’t this indicates early sign of tendon or small joint
involvement. Move the fingers passively to decide if the problem is with
the tendons or nerves, or in the joint.
Tests wrist flexion and extension both actively (prayer sign) and
passively
Perform Phalen’s test – forced flexion of the wrists for 60s – a +ve test
reproduces the pt’s symptoms
Done by thumb abduction and finger spread respectively.
Crepitus can only be felt by palpating the joint while it is moved. Coarse,
rough, palpable crepitus is a feature of osteoarthritis.
Note if pain occurs during movement
Pain throughout the range of movement is characteristic of inflammatory
disorders.
Pain at the end of a restricted range of movement occurs in
osteoarthritis.
Pain on certain movements only, suggests a periarticular disorder.
Can the joint move into abnormal positions?
If extension is present but not normal (e.g. in the knee) record as
hyperextension
Assess power and grip strength
Assesses pincer movement (Thumb to little finger).
Assesses pincer grip and function. Also, can they do buttons, keys,
write name, use a knife and fork? Test as well as ask.
Elbow examination
Look
Pt standing; expose upper limbs; look from front, side and behind
Environment
Mobility aids
Carrying angle
A valgus angle of 11-13° when elbow is extended; bigger in females due
to wide hips
Cubitus varus deformity: caused by supracondylar fracture
Cubitus valgus deformity: caused by non-union of a lateral condylar
fracture
Swelling, bruising, scars, skin change
Skin change = ?psoriatic plaques
Evidence of synovitis between lateral epicondyle and olecranon
For olecranon bursitis, trophi or nodules, muscle wasting
For rheumatoid nodules
Found on proximal extensor surface of forearm
Feel
Temperature
Use back of hand; across the joint and the forearm
Bony contours/ joint margin of elbow and
Holding forearm in one hand, and with elbow flexed at 90°, feel for
focal tenderness
lateral and medial epicondyles and olecranon (tennis and golfer’s
elbow), defining an equilateral triangle. Any focal tenderness?
Palpate any swelling:
Soft: olecranon bursitis; hard: bony deformity; boggy: synovial thickening
secondary to RA
sponginess (elbow extended) for synovitis
Bursae
Rheumatoid (subcutaneous) nodules
Move
Elbow flexion (touch your shoulder)
Elbow extension (straighten your arm)
Assess supination (arms at side of body
and flex elbow)
Pronation (turn hands to floor)
Special test: tennis elbow
Special test: golfer’s elbow
Either side of the olecranon. Any tenderness too? Synovitis is usually
felt as a sponginess/boggy between the olecranon and lateral
epicondyle.
Fluid-filled sacs near olecranon, usually soft but may be firm if acutely
inflamed/infected. Attempt to displace the fluid!
On proximal extensor surface of the forearm
Assess actively and passively, feeling for crepitus and hyperextension.
Compare both sides; check for pain first
Normal ROM is 0-145°; <30-110° = functional problems
Normal ROM is 0-90° (0° is thumb up)
Normal ROM is 0-85° (0° is thumb up)
Lateral epicondylitis: flex elbow at 90°, pronate and flex wrist fully;
support pt’s elbow and ask them to extend wrist against resistance. Pain
is produced, and may be referred down extensor aspect of arm
Medial epicondylitis: flex elbow at 90°, supinate and extend wrist fully;
support pt’s elbow and ask them to flex wrist against resistance. Pain is
produced, and may be referred down flexor aspect of arm
Function
Can the pt put the hand to their mouth? Behind their head? Jacket on?
Medial epicondyle = flexor muscle attachment = golfer’s elbow
Lateral epidcondyle = extensor muscle attachment = tennis elbow
A subcutaneous bursa overlies the olecranon: inflammation or infection = bursitis
Rheumatoid arthritis can also cause elbow pain
Shoulder examination
Look at whole shoulder girdle, inc axilla; expose upper limbs, chest and neck
From front, side and behind, topless
Symmetry, posture, scars, bruising
Environment
Aids or adaptations
Deformity
Anterior GHJ and complete ACJ dislocations are obvious; shoulder
contour in posterior GHJ dislocation may only appear abnormal when
standing above pt and looking down on the shoulder; prominence of
ACJ?
Swelling and dislocations (compare both
In dislocations, prox humeral fractures, haemarthrosis, inflam conditions,
shoulders from front)
rheumatoid effusions, pseudogout, sepsis
Muscle wasting
Of deltoid, supraspinatus and infraspinatus (latter two = chronic tear of
their tendons). These overlie upper and lower parts of scapula
Size and position of the scapula
Elevated, depressed, winged (SALT injury; brachial plexus injury; viral
infection of C5-7 nerve roots; muscular dystrophy); small and elevated
scapula occurs in rare conditions Sprengel’s shoulder and Klippel-Feil
syndrome
Feel: stand in front of pt
Check for pain first!
Temperature
Over the front of the shoulder
Palpate any bony landmarks
Sternoclavicular joint-clavicle-acromiclavicular joint-acromion process
(2cm inferomedial to lateral end of clavicle)-head of humerus-coracoid
process-scapula spine-greater tuberosity of humerus and biceps tendon
in bicipital groove. Any tenderness? Clavicular fractures and ACJ
injuries = local tenderness and deformity
Supraspinatus tendon
Extend the shoulder (brings supraspinatus anterior to the acromion
process); tenderness is present with ligamentous tears and calcific
tendonitis
Palpate the muscle bulk
Of the supraspinatus-infraspinatus-deltoid muscles
Supraclavicular area
Lymphadenopathy
Move: stand behind pt
First two = screening tests: fully examine shoulder if in pain
Both hands behind head
Assess external rotation in abduction; compare both sides
Arms down, both hands behind their back
Assess internal rotation in adduction; compare both sides. If there’s a
to touch their ‘shoulder blades’
restriction, describe what the pt can achieve – can they reach the
lumbar, lower thoracic or mid-thoracic level?
Determine active and passive ROM at each stage; to test true GHJ movement, anchor the scapular by
pressing down on the shoulder. After ~70° of abduction, the scapula rotates – scapulothoracic movement
Ask pt to raise the hands behind them and
Assess flexion and extension
to the front above their head
With elbow flexed at 90° and tucked into
Assess external rotation; difficulty may indicate frozen shoulder
pt’s side (thumb up)
As above but in across body
Assess internal rotation; loss = capsulitis
Ask pt to move arms inwards across their
Tests adduction
trunk
Ask pt to abduct the arm/ move arm out
Assess for a painful arc (between 60° and 120°):
from body so fingertips are pointing to the
Active: pt abducts arm– pain?
ceiling
- If pt can’t initiate abduction, passively abduct pt’s arm (which is
internally rotated) to 30-45° while placing your hand over their
If any limitation, lack of initiation or pain
scapula to confirm there is no scapula movement. Ask pt to
(painful arc), then test rotator cuff.
continue abduction. Pain on active movement, esp against
resistance, suggests impingement
- If pt can actively abduct arm: then passively abduct arm fully
and ask pt to lower/adduct it slowly
Ask pt to abduct arm against resistance: tests deltoid to abduct against
resistance; compare both sides side.
Ligamentous tears and injuries
Pain in early abduction = rotator cuff lesion, usually occurs between 40120°; due to damaged/inflamed supraspinatus being compressed
against the acromial arch (impingement)
Pain in late abduction (>90°) which prevents pt from raising arm straight
above head, even passively, is suggestive of acromioclavicular arthritis
Tests component muscles of rotator cuff (have to neutralise the effect of
other muscles crossing the shoulder). Discrepancy between active and
passive ROM = ?tendinous tear
Subscapularis and pec major = powerful internal rotators. To isolate the
subscapularis, test internal rotation with the pt’s hand behind their back.
Loss of power = tear; pain on forced internal rotation = tendonitis
Supraspinatus: with arm by their side, test abduction. Loss of power =
tear; pain on forced abduction = tendonitis
Bicipital tendonitis
Function
Can the pt put their hands behind their
head/back?
Can they put a coat on?
Infraspinatus and teres minor: test external rotation with arm in the
neutral position (but with 30° flexion to minimise deltoid involvement).
Loss of power = tear; pain on external rotation = tendonitis
Palpate the bicipital tendon in its groove – any tenderness?
Ask pt to supinate the forearm, and then flex arm against resistance.
Pain = bicipital tendonitis
Involved in washing, grooming and getting dressed
Conditions affecting the shoulder
Non-trauma
Trauma
Rotator cuff syndromes, e.g. supraspinatus,
infraspinatus tendonitis
Impingement syndromes (involving the rotator
cuff and subacromialbursa)
Adhesive capsulitis ('frozen shoulder')
Calcific tendonitis, often after injury/stroke
Bicipital tendonitis
Rheumatoid arthritis
Rotator cuff tear
Glenohumeral dislocation
Acromioclavicular dislocation
Fracture of the clavicle
Fracture of the head or neck of the humerus
Causes of shoulder girdle pain
Rotator cuff Degeneration, tendon rupture, calcific
tendonitis
Subacromial Calcific bursitis, polyarthritis
bursa
Capsule
Adhesive capsulitis
Head of
Tumour, osteonecrosis, fracture/dislocation
humerus
Joints
Glenohumeral, sternoclavicular - synovitis,
osteoarthritis, dislocation, Acromioclavicular –
osteoarthritis
Referred
Cervical spine, radicular pain by central nerve
root compression, diaphragm (by phrenic
nerve). Commonest cause is cervical spondylosis
(disc narrowing and osteophytes = nerve root
impingement
Hip examination
Look expose whole of lower limb
Environment
With pt standing, inspect from front,
side and back
Special attention
With pt lying flat and face up
Leg length
Scars
Feel
Palpate over the greater trochanter and
ASIS
Palpate soft tissue contours
Move
With pt supine
Flexion
Abduction
Adduction
With pt prone
Extension
Internal rotation
External rotation
Active internal and external rotation:
pt supine
Thomas’ test;
Assesses for a fixed flexion deformity of
the hip (often seen in OA) which are
hidden when the pt lies supine by arching
their back and tilting their pelvis.
Trendelenberg test;
Exposes dislocation and subluxations,
weakness of the abductors, shortening of
the femoral neck
Function
Ask the pt to walk
Orthopaedic shoes (1 boot with a big heel), walking aids
Muscle wasting, esp gluteal muscle bulk, scars, sinuses, asymmetry of
skin creases, swelling, deformities
Position of limbs (eg external rotation, pelvis tilting, standing with one
knee bent, foot held plantarflexed or in equinus)
Compare each leg: is there an obvious flexion deformity of the hip?
If possible disparity, then measure with a tape measure (from anterior
superior iliac crest to medial malleolus of the ankle). A fractured neck of
femur = leg is shorter and externally rotated
Previous ops?
Tenderness? In the expected position?
Tenderness in and around the joint
Ask pt if they’re in any pain
Fix pelvis by using left hand to stabalise the contralateral ASIS since
any limitation of hip movement may be masked by movement of the
pelvis
Ask pt to flex hip until knee meets abdomen; normal ROM = 120°
With pt’s leg straight, ask them to move it out from the midline; normal
ROM = 30-40°
With pt’s leg straight, ask them to move it across the midline; normal
ROM = 30°
Ask pt to raise each leg off the bed; normal ROM = a few°
Ask pt to keep knees together but spread ankles as far as possible
Ask pt to cross the legs over
Hip and knee flexed at 90°, one hand supports the knee, the other
moves the ankle medially and laterally; often limited in hip disease
Keep one hand under pt’s back to ensure that normal lumbar lordosis is
removed (palm up). Fully flex one hip and observe the opposite leg – if it
lifts of the couch then there is a fixed flexion deformity in that hip (as
pelvis is forced to tilt a normal hip would extend allowing the leg to
remain on the couch). Test both hips.
Ask pt to stand upright with no support.
Ask them to raise their left leg by bending the knee. Watch the pelvis,
which should normally rise on the side of the lifted leg.
Repeat the test but with pt standing on left leg/raising right leg.
+ve test = pelvis falls on the side of the lifted leg = hip instability on the
stance side (ie the pelvis will dip on the contralateral side to muscle
weakness eg stand on right leg, pelvis on left will dip if gluteal muscles
on right are weak)
Antalgic gait = painful => presents as a limp
Trendelenberg gait = weak proximal muscles => ‘waddle’
Hip problems: osteoarthritis, trochanteric bursitis, tendonitis (of ileotibial head), osteonecrosis, fractured hip (elderly
and athletes)
Knee examination
Look: with pt lying flat on couch
Inspect environment
Walking aids?
Deformity? Genu valgum/varum Valgus deformity (knock-kneed), where leg below the knee is deviated laterally or
varus deformity (bow-legged), where the leg below the knee is deviated medially
Check for knee flexion deformity If pt lies with one knee flexed, this may be due to a knee or hip problem: distinguish
by examining the hip movements as above
Muscle wasting
Quadriceps wasting almost invariable with inflammation or chronic pain and
develops within days. ?measure girth in both legs 20cm above tibial tiberosity
Leg length discrepancy
Neck of femur fracture
Scars
Suggest previous operation or infection
Erythema
Inflammation
Swelling
Anteriorly and posteriorly: an enlarged pre-patellar bursa (housemaid’s knee) and
any effusion around the joint. A large effusion forms a horseshoe-shaped swelling
above the knee. Swelling beyond the joint margins = infection, trauma, tumour
Rash
Psoriasis
Loss of medial and lateral
Possible effusion? Found in septic arthritis, haemarthrosis and trauma
dimples around patellar
Feel:
Check for pain first
Temperature
Using back of hand; mid-thigh to knee; compare both knees. Warm in septic
arthritis, haemarthrosis and inflammatory arthritis
Palpate along the borders of the Tenderness?
patella and joint line of the knee, Palpate for tenderness and swelling along the joint line from the femoral condyles
and do so whilst pt bends knee
to the inferior pole of the patella, then down the inferior patellar tendon to the tibial
slightly
tuberosity. Localised pain over tibial tiberosity = Osgood-Schlatter disease
Collateral ligaments
Either side of joint
Synovitis
Pt’s knee extended and quads relaxed, ?sponginess on both sides of quads tendon
Baker’s/popliteal cyst
Behind the knee in popliteal foassa
Large effusion; knee extended
Perform a patellar tap; apply firm pressure over suprapatellar pouch with flat of
hand working from quads to patellar. Tap on patellar (against femur)
Small effusion ‘ripple test’
If no obvious tap then assess for a fluid bulge by cross fluctuation.
Drain suprapatellar pouch. Empty medial joint recess using a wiping motion with
index finger: stroke the medial side of the knee upwards towards the suprapatellar
pouch to empty the medial compartment of fluid.
Then apply a similar wiping motion to lateral recess and watch the medial side. if it
re-fills = effusion
Move
Assess full flexion and
Assess active movement and passive movement (place one hand on the knee to
extension
feel for crepitus when assessing passively). Note the ROM. Knee to chest (0-140°).
Crepitus: chondromalacia in young females or OA. Restriction to full extension
occurs in meniscal tears, OA and inflamm arthritis; hyperextension up to 10° is
normal (genu recurvatum)
Quadriceps weakness
Ask pt to lift leg with knee kept straight; if the knee can’t be fully extended, an
extensor lag is present
With knee flexed at 90°, check
Initially, look from the side of the knee for posterior sag or step-back of the tibia =
stability of knee ligaments
posterior cruciate damage
Medial collateral ligament;
Flex knee to about 15°; hold ankle between elbow and side. Place hand on lateral
Valgus stress test
joint line whilst holding foot and ankle and lower tibia with other arm. Push
Lateral collateral ligament;
medially. Place hand on medial joint line; pull laterally. Normally, joint should move
Varus stress test;
no more than a few degrees; excessive movement = torn or stretched lig
Anterior/posterior drawer test;
Flex knee at 90°. Both hands on leg so thumbs are on tibial tuberosity and index
Posterior sag will result in false
fingers under hamstrings. Sit on foot. Gently pull tibia towards you. Normally, there
+ve anterior drawer test; ACL
is no/small movement. Significant movement (>1.5cm)anteriorly (and soft ending) =
tear ass with medial collat. tear
anterior cruciate ligament laxity; excessive movement posteriorly = PCL tear/laxity
Patellar apprehension test
Knee extended; push patellar laterally whilst flexing the knee. If pt resists flexion,
suggests previous patellar dislocation or instability
McMurray’s test for cartilage
Meniscal tears? With pt lying supine, bend hip and knee to 90°. Grip heel with right
hand and press on medial and lateral cartilage with left hand.
Internally rotate tibia on femur and slowly extend knee
Repeat but externally rotate tibia on femur whilst slowly extending knee; if torn, a
tag of cartilage may become trapped between the articular surfaces and cause
pain/audible click; may also feel crepitus.
Apley’s test for cartilage
With pt prone, flex knee to 90° and stabalise thigh with left hand. Grip foot with right
hand. Rotate or twist the foot downwards (grind!). torn meniscus produces
Provocation tests: menisci
Function
Ask pt to walk a few steps again
Squat test
symptoms.
Medial meniscus: passively flex knee to full extent; externally rotate foot and
abduct the thigh at the hip; extend knee smoothly; click or clunk felt/heard = tear
Lateral meniscus: internally rotate foot and adduct leg at hip
Varus or valgus deformity?
Keeping the feet and heels flat on the ground; if he can’t do this it indicates
incomplete knee flexion on the affected side = ?tear of the posterior horn of the
menisci
Knee problems: Osteoarthritis, cartilage problems, patellofemoral syndrome, cruciate ligament injury, Osgood
Schlatters syndrome
Foot and ankle examination
Look: expose lower limbs
With pt weight-bearing
Midfoot
Foot arch position; a dropped arch in a normal subject should resolve
when they stand on tip-toes
Calcaneal tendon thickening or swelling
Disease of the ankle or talar joint = varus or valgus deformity
From behind
Normal alignment of the hindfoot (look
from behind)
With pt sitting on couch and their feet overhanging the end of it
Environment
Walking aids? Orthopaedic shoes?
Pt’s footwear
Abnormal or symmetrical wearing of the sole? Evidence of a poor fit?
Presence of insoles?
Soles of feet
Calluses? Swellings, ulcers, scars?
Feet
Deformities: pes planus (flat footed), pes cavus (high-arched foot)
Symmetry or rashes (psoriasis)
Nails
Fungal infections? In-growing toe nails?
In between toes as well!
Hallux valgus of the big toe = bunion deformity = deviates laterally
Alignment of the toes
and ‘bump’ develops on medial side of 1st MTPJ (the bunion)
Clawing of the toes: MTPJ hyperextended, PIP and DIP flexedwith
?fixed contracture of each joint. Unopposed EHL and EHB cause
hyperextension. Result = inability to apply pulp of big to to floor when
standing.
Hammer toes: deformity of PIP of 2nd, 3rd and 4th toe causing it to be
permanently bent; may also have corns on top of joint and callus where
MTPJ contacts floor.
If there I clawing of toes, or calluses above and below the MTPJ, pain
and restriction of movement there may be subluxation (partial
dislocation) of the MTPJ.
Talipes equinovarus (clubbing of feet)
Calf and lower leg
Muscle wasting; if suspect then measure 10cm below the tibial
tuberosities
Feel
Always check for pain first!
Temperature
Over forefoot and ankle
Areas of tenderness? Palpate midfoot,
Over bony prominences: lateral and medial malleoli, MTPJ, IPJ, heel,
ankle joint line and subtalar joints
metatarsal heads
Peripheral pulse
Squeeze across MTPJ
Tenderness, watch pt’s face, assess for movement too
Palpate any swelling, oedema or lumps
Move
Assess active and passive movement; passive first
Ankle dorsiflexion
Ask pt to point toes towards their head
Ankle plantarflexion
Ask pt to push their toes towards the floor like pushing on a pedal
Inversion: subtalar joint between talus and
Passive: ask pt to turn foot inwards.
calcaneum
Active: grasp ankle with one hand, grasp the heel with the other (fixes
the calcanuem), turn sole inwards towards midline
Eversion
As inversion but turn sole outwards
Midtarsal joints
Active: grasp the heel with one hand and with the other attempt to move
the tarsus up and down and side-to-side
Toe flexion
Ask pt to curl their toes
Toe extension
Ask pt to straighten their toes
Toe abduction
Ask pt to fan out their toes as far as possible
Toe adduction
Ask pt to hold a piece of paper between their toes
Movement of mid-tarsal joints
Fix the heel with one hand and with the other, passively invert and evert
the forefoot.
Ottawa ankle test
Simmond’s test: assess for a ruptured
Ask the pt to kneel on a chair with their feet overhanging the edge.
Achilles tendon
Squeeze both claves; normally the foot will plantarflex but it won’t if torn
Function
Gait with and without shoes
Is there normal cycle of heel strike, stance and toe-off?
Ankle joint and foot problems: sprain, dropped arches, bunions, plantar fasciitis, calcaneal spur, achiles tendon
rupture
Spine examination
Look with pt standing, stripped down to underwear
Environment
Wheelchair? Walking aids?
From front, behind
Muscle wasting, asymmetry, scoliosis, scars, pigmentation, abnormal
hair growth (congenital abnormality e.g. spina bifida.)
From the side
Normal cervical lordosis(concave), thoracic kyphosis(convex), lumbar
lordosis(concave)
A ‘question mark’ spine (exaggerated thoracic kyphosis and a loss of
lumbar lordosis) is classic ankylosing spondylitis
Watch how pt moves onto bed
Feel
Down the spinal processes (T1 is most
Notice any prominence or step in spinal processes
prominent) and over sacroiliac joints
Palpate paraspinal muscles
Tenderness
Supraclavicular fossae
For cervical ribs or enlarged cervical lymph nodes
Anterior neck structures
Thyroid
Palpate sacroiliac joints
Move: start at neck and move down!
Assess active and passive movements;
Cervical spine movements (demonstrate
Assess active movements first.
the movements to the pt)
Flexion: bring their chin onto their chest (0-80°)
Extension: tilt their head backwards; look up (0-50°)
Lateral flexion: tilt their head to the side: touch ear on to shoulder (0-45°)
Rotation: turn head to look over each shoulder (0-80°)
Sudden/gradual resistance? Pain/paraesthesia in arm?
Thoracic and lumbar spine
Flexion: touch your toes
Extension: lean backwards
Lateral flexion: bend sideways, sliding hand down their leg
Rotation: anchor pelvis (put my hands either side, or ask them to sit
down), and then twist at the waist either way
Schober’s test – measure lumbar flexion
Standing erect, identify posterior superior iliac spines (located at L5 at
the ‘dimples of Venus’), mark with a pen 5cm below and 10cm above
the midline point between the PSIS, ask pt to lean forward; distance
between the two pen marks should be >20cm. If not, then there is
limitation of lumbar flexion (ie ankylosing spondylitis).
Alternatively, place two fingers over lumbar spine. Ask pt to touch their
toes. Your fingers should move apart during flexion and together in
extension.
Straight leg raise/ sciatic nerve stretch test Raise the leg to 90° (age-dependednt as elderly won’t be able to do this)
Pt lies supine
with the knee extended. Then dorsiflex the foot (Bragard test). If +ve =
exacerbate pain felt in back of thigh, which is relieved by knee flexion
Tension of the nerve roots supplying sciatic nerve (L5-S2); by nerve root
entrapment or irritation caused by a prolapsed disc (L4/5 or L5/S1)
Femoral nerve (L2-4) stretch test
Abduct and extend the hip, flex the knee and plantarflex the foot; +ve if
Pt lies prone
pain is felt in the thigh/inguinal region
Tibial nerve stretch
Flex the hip to 90° and extend the knee (causes the tibial nerve to
Pt lies supine
'bowstrings' across the popliteal fossa).
Press over either of the hamstring tendons, and then over the nerve in
the middle of the fossa. +test = if pain occurs when the nerve is pressed,
but not the hamstring tendons
Flip test (functional) overlay
Pt sits on end of couch with hips and knees flexed to 90°. Examine knee
reflexes. Extend the knee as if to examine ankle reflexes. The pt will
lie/flip back if they have a prolapsed disc.
If either of above two tests are +ve, suggest examining neurological and functional consequences
Causes of abnormal neck posture
Loss of lordosis or
Acute lesions, rheumatoid arthritis
flexion deformity
Increased lordosis
Ankylosing spondylitis
Torticollis (wry neck) Sternocleidomastoid contracture
Lateral flexion (cock Erosion of lateral mass of atlas in
robin position)
rheumatoid arthritis
Causes of pain in the thoracic spine
Adolescents and young adults
Scheuermann's disease
Ankylosing spondylitis
Disc protrusion (rare)
Middle-aged and elderly
Degenerative change
Osteoporotic fracture
Any age: tumour; infection
Red flag for back pain
History
Age < 20 years or > 55 years
Recent significant trauma (fracture)
Pain:
o thoracic (dissecting aneurysm)
o non-mechanical (infection/tumour/pathological fracture)
Fever (infection)
Difficulty in micturition
Faecal incontinence
Motor weakness
Sensory changes in the perineum (saddle anaesthesia)
Sexual dysfunction (e.g. erectile/ejaculatory failure)
Gait change (cauda equina syndrome)
Bilateral 'sciatica'
Past medical history
Cancer (metastases)
Previous steroid use (osteoporotic collapse)
System review
Weight loss/malaise without obvious cause (e.g. cancer)
Common spinal problems
Stretch tests: sciatic nerve. (A) Straight leg
raising limited by tension of root over
prolapsed disc. (B) Tension increased by
dorsiflexion of foot (Bragard's test). (C) Root
tension relieved by flexion at the knee. (D)
Pressure over centre of popliteal fossa bears on
posterior tibial nerve which is 'bowstringing'
across the fossa, causing pain locally and
radiation into the back.
Mechanical back pain
Prolapsed intervertebral disc
Spinal stenosis
Ankylosing spondylitis
Compensatory scoliosis resulting from leglength discrepancy
Cervical myelopathy
Pathological pain/deformity (e.g.
osteomyelitis, tumour, myeloma)
Osteoporotic vertebral fracture resulting in
kyphosis (or rarelylordosis), especially in
the thoracic spine with loss of height
Cervical rib
Scoliosis
Spinal instability (e.g. spondylolisthesis)
Stretch test: femoral nerve. (A) Pain may be
triggered by knee flexion alone. (B) Pain may be
triggered by knee flexion in combination with
hip extension.
To conclude:
A brief neurovascular examination including assessment of upper and lower limb reflexes, dorsiflexion of the big toe
and assessment of peripheral pulses. If any indication from the history, a full neurological and vascular assessment –
tone, power, sensation – should be carried out.
Investigations:
1. Imaging of bones and joints:
Plain X-ray – RA, OA, gout
MRI
CT
Isotope bone scans
DEXA scans – osteoporosis
Ankylosing spondylitis
2. Blood tests:
Indicate degree of inflammation and in monitoring response to therapy.
Erythrocyte sedimentation rate (ESR) is used and responds over days-longer but is non-specific and altered by many
things eg anaemia. C-reactive protein (CRP) responds more rapidly.
Serum uric acid – gout; may be unreliable during an acute episode
Autoantibodies: inflammatory arthropathyeg RA, though significance not always clear (Rheumatoid factor indicates RA
but is not pathogonomic)
Inflammatory arthropathy: could be caused by an infection, esp if only a single joint is affected. Send blood cultures
even if no fever present.
3. Synovial fluid analysis:
To exclude infection in the joint.
Synovial fluid should be sent for culture and gram staining.
If gout suspected, fluid should be assessed for cyrstals under a polarising light microscope.
Reference points
In general terms all the joints of the body are said to be at 0 neutral position when the body is in the anatomical
position. This would mean that the elbows are at full extension and can only flex, whilst the hip, shoulders, ankle and
wrist can both flex and extend.
Normal ranges – use a goniometer to measure the angle!
Differ and change as people age – children are much more supple than adults, and the joints continue to lose flexibility
throughout life. The measurements listed below are only a rough guide for an average adult.
Joint
Knees
Elbows
Hips
Shoulders
Spine
Movement
Flexion
Flexion
Pronation
Supination
Flexion
Extension
Abduction
Adduction
Internal Rotation
External Rotation
Flexion
Extension
Abduction
Adduction
External Rotation
Internal Rotation
Add in here!!!
Degree of Movement
0 - 140 (flexion only although hyperextension possible)
0 - 150 (as per knee)
0 - 90
0 - 80
0 - 120
0 - 40
0 - 40
0 - 30
0 - 30 (Test with knee flexed to 90)
0 - 30
0 - 180
0 - 50
0 - 180
0 - 40
0 - 45 (Test with elbow flexed to 90)
0 - 110 Often expressed as functional ability – maximum is to reach upper back
Introduction
The term “arthritis” means “inflammation of the joint(s)”, but is often used to include all joint disorders. “Rheumatism” is
an imprecise term often used by non-medical people to describe pain in muscles, bones or joints. The World Health
Organisation (WHO) has classified “arthritis and rheumatism” into four main categories:
1.
2.
3.
4.
Regional periarticular or ‘soft tissue’ diseases.
Back pain.
Osteoarthritis and related disorders.
Inflammatory arthropathies.
1. The regional, periarticular, soft – tissue disorders
This term covers an extremely common set of relatively minor conditions affecting the tissues surrounding a joint.
Most are caused by unaccustomed or repetitive usage, or by trauma: 'tennis elbow', 'housemaid's knee’ or
'policeman's heel'. A modern, computer age addition to this group of disorders is ‘repetitive strain injury’ (RSI).
Inflammation of a bursa, ligament, ligament insertion, tendon, tendon insertion, or tendon sheath causes regional pain
exacerbated by certain activities with localized tenderness.
2. Back pain
Nearly everyone suffers backache from time to time. Episodes of severe, incapacitating back pain are common in
young adults, and a major cause of work loss. Most resolve spontaneously after a few weeks, but there is also a high
incidence of recurrence, and of severe chronic back pain.
A precise diagnosis of the cause is often impossible. However, a minority of cases have a weIl-characteristed disorder
such as:
o a prolapsed intervertebral disc
o an inflammatory arthritis of the spine (such as ankylosing spondylitis), or
o a bony condition like osteoporosis.
There are numerous other uncommon but serious causes of back pain, including some neoplastic and infective
conditions e.g. myeloma, prostatic cancer deposits, other secondary deposits, T.B. of the spine
3. Osteoarthritis
Osteoarthritis (OA) is the commonest form of joint disease. It is an age-related condition in which there is focal
damage to the articular cartilage surfaces of the joint and a reaction in the underlying bone. In most cases it is
idiopathic but may develop secondary to any joint disorder.
It causes pain on movement, often worst at the end of the day, pain at rest, stiffness and joint instability.
It mostly affects weight bearing joints like hips and knees but also often affects the hands, cervical and lumbar spine.
Common manifestations are: joint tenderness , bony swellings ( e.g. Heberden’s nodes ), limitation of joint movement
and effusions.
4. The inflammatory arthropathies
This group of conditions includes systemic diseases which target joints ( e.g. rheumatoid arthritis), as well as purely
local inflammatory disorders ( e.g. septic arthritis). It includes some of the most severe, painful and disabling chronic
diseases, many of which have their onset in children or young adults.
Rheumatoid Arthritis (RA)
Psoriatic arthropathy
Juvenile chronic arthritis
Ankylosing Spondylitis
Reactive arthropathy
Crystal arthritis
Connective tissue disease e.g.: systemic lupus erythematosus
Septic arthritis
Inflammatory arthropathies are characterized by synovitis which causes painful swelling of joints, with warmth and
sometimes redness of the overlying skin. Usually many joints are affected.
The pattern of distribution of joint involvement is characteristic for the various disorders.
e.g.:
in RA in the hand the most commonly involved joints are the:
1. Metacarpo - phalangeal joints (MCP joints) and
2. The proximal inter phalangeal joints (PIP joints).
3. Often there is subluxation of the MC joints resulting in the characteristic ulnar deviation of the fingers.
In Psoriatic arthropathy the distal inter phalangeal joints (DIP joints) are typically involved and this is associated with
pitting and dystrophy of the nails.
Septic arthritis and acute gout often present with involvement of a single joint, i.e. a mono – arthritis.
Symptoms in Musculo – Skeletal Disease
The inflammatory arthropathies are systemic diseases and patients may experience symptoms and disturbances
outside the musculo-skeletal system per se (extra – articular manifestations).
Chronology :
a. Onset - time and circumstances of disease onset : ?acute or gradual and insidious
b. Progression
? rapidly progressing to maximum intensity of symptoms
?running an up and down course with exacerbations and remissions
For example,
i. Gout often starts in the middle of the night (often after surgery, trauma, or an illness like heart failure requiring the
prescription of large doses of diuretics) and becomes excruciatingly painful within a few hours.
ii. Reactive arthritis often starts with redness of the eyes followed by urethritis and an asymmetrical arthritis moving
from joint to joint, often two to three weeks after a gut or urogenital infection.
iii. Inflammatory polyarthropathies often start insidiously with joint pain and stiffness associated with general malaise
and tiredness and may run a variable course with exacerbations and remissions.
iv. The sudden, acute onset of severe pain in the lower back, often starting after getting up in the morning with severe
stiffness of the back and severe restriction of movement, often associated with shooting pains down the thigh and
leg suggests a prolapse of an intervertebral disc.
Symmetrical polyarthropathy involving small peripheral joints.
Both wrists are swollen and deformed.
There is swelling of almost all MCP joints( metacarpo-phalangeal joints).
There is some involvement and swelling of the PIP joints (proximal
interphalangeal joints).
There is some tendency to the formation of the ‘swan neck deformity’ in the
fourth and fifth fingers of both hands ->extension or hyperextension at the PIP
joint with flexion of the DIP joint ( distal interphalangeal joint ) giving the finger a
bit of an ‘S’ shape.
Additional observations : a. paper thin, wasted, atrophic skin; b. wasting of small
muscles of the hand – here you can see the wasted dorsal interossei c. nicotine staining of the nail of the right
index finger.
Diagnosis : most likely Rheumatoid Arthritis
Large, typical rheumatoid nodules on the extensor surface of the forearm.
They vary in size a lot and can be found in relation to tendons and joints. The extensor surface of the forearm is a
very characteristic site and should always be examined in a patient suspected of having rheumatoid arthritis.
Polyarthropathy involving small peripheral joints affecting predominantly the
DIP joints (distal interphalangeal joints) which are swollen.
The nail of the index finger shows typical psoriatic pitting. Other nails are
dystrophic.
This distribution of joint involvement together with the nail disease suggests
Psoriatic Arthritis
Shiny, yellowish deposits in nodules related to the DIP joint of the index finger. Very suggestive of urate
deposition.
Haphazard involvement of various joints of the hand. Some of the nodules look very
much like urate deposits. The picture is very suggestive of Gout.
Resolving acute mono - arthritis in DIP joint of the middle finger due to gout in a chronic
alcohol abuser.
General features:
Face
Hands
Body appearance/deformity
Specific examination features for you to practise:
inspection& palpation of joints
joint movement
inspection& palpation of spine
spinal movement
examination of limbs
gait
I have seen and read about the following conditions and can identify the common symptoms and signs
seen
read
about
give one common symptom and sign
Osteoarthritis
Rheumatoid arthritis
Spinal scoliosis
Hip fracture
Complicated long
bone fracture
Gout
Septic arthritis
I have seen or heard described the (1)following signs or symptoms and can distinguish the most common
causes
seen
read
about
give one common cause
joint effusion
muscle wasting
abnormality of gait
1.
Li S, Harrison D, Carbonetto S, Fassler R, Smyth N, Edgar D, and Yurchenco PD. Matrix assembly,
regulation, and survival functions of laminin and its receptors in embryonic stem cell differentiation. The Journal of cell
biology 157: 1279-1290, 2002.