What do these people have in common?
advertisement

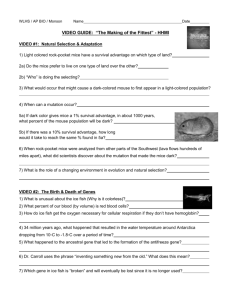
Sickle Cell Anemia From DNA to Disorder A production • /1pt Gene(s) Involved & DNA Code (length, arm, +/- strand and loci on chromosome, name of gene, discovery info, actual base sequence, introns/exons, cDNA, mRNA) • /1pt Protein Affected (How are primary through quaternary structure affected? How is enzyme activity affected? normal vs abnormal expression) • /1pt Cellular, Tissue & Organ effects (What signal transduction pathways are interrupted? What morphological changes in cells, tissues and organs result?) • /1pt Organ system effects (What body system(s) is(are) affected? How is it affected? How is disordered function different than normal function?) • /1pt Organism effects (What symptoms exist? How is it diagnosed?) • /1pt Treatment/Prevention (What preventative measure can be taken? What treatments are available? What treatments are presently being researched or are in clinical trials?) • /1pt Genetics (What is the mode of inheritance? Possibly include a Punnett Square and pedigree) • /1pt Ecological/Evolutionary effects/significance (In what geographic/ethnic population(s) is this disorder prevalent? Why those?) • /1pt Your Choice/Miscellaneous (choose an area not mentioned above to delve further into) • /1pt References (complete APA format bibliography with at least 3 references) Introduction Sickle Cell Anemia is a blood disorder caused due to mutation in the beta chain of the protein Hemoglobin. Hemoglobin primarily binds with oxygen allowing its transport throughout the blood for cellular processes. Gene(s) Involved & DNA Code There are various globin genes Chromosome 16 • Alpha (3-9mos) • Zeta (<8wks) Chromosome 11 • Beta (after birth) • Epsilon (<8wks) • Gamma (3-9mos) • Delta (after birth) Gene(s) Involved & DNA Code Official Gene Symbol: HBB Name of Gene Product: hemoglobin, beta Alternate Name of Gene Product: beta globin Gene(s) Involved & DNA Code Locus: 11p15.5 - The HBB gene is found in region 15.5 on the short (p) arm of human chromosome 11 Gene Structure: The normal allelic variant for this gene is 1600 base pairs (bp) long and contains three exons mRNA: The intron-free mRNA transcript for the HBB gene is 626 base pairs long. Coding Sequence (CDS): 444 base pairs within the mRNA code for the amino acid sequence of the gene's protein product Protein Size: The HBB protein is 146 amino acids long and has a molecular weight of 15,867 Da. Gene(s) Involved & DNA Code Sickle Cell is due to a point mutation. A substitution of the 2nd base in the 6th amino acid of the protein. Gene(s) Involved & DNA Code Gene Structure: The normal allelic variant for this gene is 1600 base pairs (bp) long and contains three exons mRNA: The intron-free mRNA transcript for the HBB gene is 626 base pairs long. Coding Sequence (CDS): 444 base pairs within the mRNA code for the amino acid sequence of the gene's protein product Gene(s) Involved & DNA Code A variety (376) of hemoglobin mutations exist including missense and nonsense substitutions, deletions, insertions, duplications and rearrangements (including inversions) Protein Affected Although several hundred HBB gene variants are known, sickle cell anemia is most commonly caused by the hemoglobin variant Hb S. In this variant, the hydrophobic amino acid valine takes the place of hydrophilic glutamic acid at the sixth amino acid position of the HBB polypeptide chain. Protein Affected Hemoglobin is a protein with 4 subunits Alpha chains consist of 141 amino acids Beta chains consist of 146 amino acids There are few alphaalpha or beta-beta interactions, but many alpha-beta hydrophobic interactions Protein Affected The SCA substitution creates a hydrophobic spot on the outside of the protein structure that sticks to the hydrophobic region of an adjacent hemoglobin molecule's beta chain. This clumping together (polymerization) of Hb S molecules into rigid fibers causes the "sickling" of red blood cells. Protein Affected Polymerization occurs only after red blood cells have released the oxygen molecules that they carry to various tissues throughout the body. Once red blood cells return to the lungs where hemoglobin can bind oxygen, the long fibers of Hb S molecules depolymerize or break apart into single molecules. Protein Affected Polymerized sickle hemoglobin does not form single strands. Instead, the molecules group in long bundles of 14 strands each that twist in a regular fashion, much like a braid These bundles self-associate into even larger structures that stretch and distort the cell. An analogy would be a water balloon which was stretched and deformed by icicles. Polymers of deoxygenated sickle hemoglobin molecules. Each hemoglobin molecule is represented as a sphere. The spheres twist in an alpha helical bundle made of 14 sickle hemoglobin chains. Cellular, Tissue & Organ effects A sickled red blood cell filled with sickle hemoglobin fibers. Several fibers (see arrows) are outside the cell. Cellular, Tissue & Organ effects Cycling between polymerization and depolymerization causes red blood cell membranes to become rigid Cellular, Tissue & Organ effects Another problem with sickle cells is that they do not last as long as normal red blood cells. Normal round red cells live about 120 days. Sickled red cells are more fragile than normal red cells and live for less than 60 days. The body cannot make red cells as fast as the sickle cells are being broken down. As a result the body has fewer red cells and less hemoglobin than normal, and this we call anemia. To determine the hematocrit, whole blood in a tube is centrifuged to pellet the red cells (packed red cells). Plasma remains on top of the packed red cells. The fraction of the blood that is packed red cells is the hematocrit. In this example, the hematocrit is about 40%. Organ system effects The rigidity of these red blood cells and their distorted shape when they are not carrying oxygen can result in blockage of small blood vessels. This blockage can cause episodes of pain and can damage organs. Organism effects Anemia results in less oxygen being carried to various organs and tissues, including the heart, brain, lungs, and muscles. Without enough oxygen, these organs do not function effectively. Weariness and general fatigue may be signs of Anemia. Organism effects Due to poor circulation of blood (oxygen and nutrients) SCA sufferers are subject to several complications in addition to anemia: Sickle Dactylitis, bone pain, priapism, leg ulcers, strokes, bone pain, splenic sequestion, kidney damage, chest syndrome, pain episodes Organism effects Organism effects Genetics Sickle cell anemia is an autosomal recessive genetic disorder. For the disease to be expressed, a person must inherit either two copies of Hb S variant or one copy of Hb S and one copy of another variant. Genetics Individuals who have one copy of the normal HBB gene (Hb A) and one copy of Hb S, are described as having sickle cell trait and do not express disease symptoms. Ecological/Evolutionary effects/significance Malaria Sickle Cell Sickle cell anemia is particularly common among people whose ancestors come from sub-Saharan Africa; Spanish speaking regions (South America, Cuba, Central America); Saudi Arabia; India; and Mediterranean countries, such as Turkey, Greece, and Italy. Ecological/Evolutionary effects/significance In areas where the sickle cell gene is common, the immunity conferred has become a selective advantage. Individuals heterozygous for SCA have a higher resistance to infection from malaria Treatment/Prevention Many treatments are being used and researched to prolong the lives and quality of life in SCA sufferers. These include: Hydroxyurea, bone marrow transplant, gene therapy, stroke prevention (STOP) study and adhesion blockers. Treatment/Prevention Hydroxyurea All people have fetal hemoglobin in their circulation before birth. Fetal hemoglobin protects the unborn child and newborns from the effects of sickle cell hemoglobin. Unfortunately, this hemoglobin disappears within the first year after birth. One approach to treating sickle cell disease is to rekindle production of fetal hemoglobin. The drug, hydroxyurea induces fetal hemoglobin production in some patients with sickle cell disease and improves the clinical condition of some people. Hydroxyurea also helps to fight against HIV. Treatment/Prevention Gene therapy This is a technique whereby the absent or faulty gene is replaced by a working gene, so that the body can make the correct enzyme or protein and consequently eliminate the root cause of the disease. Leboulch's team removed the bone marrow from mice with a sickle cell disease, isolated the stem cells—which give rise to red blood cells—and inserted the new anti-sickling gene. When the genetically modified stem cells were transplanted back into the mice, they produced healthy round red blood cells. http://news.nationalgeographic.com/news/2001/12/1213_TVsickle.html Your Choice/Miscellaneous The precise mechanism by which sickle cell trait imparts resistance to malaria is unknown. A number of factors likely are involved and contribute in varying degrees to the defense against malaria. People with normal hemoglobin (left of the diagram) are susceptible to death from malaria. People with sickle cell disease (right of the diagram) are susceptible to death from the complications of sickle cell disease. People with sickle cell trait, who have one gene for hemoglobin A and one gene for hemoglobin S, have a greater chance of surviving malaria and do not suffer adverse consequences from the hemoglobin S gene. Your Choice/Miscellaneous Homologues for the HBB gene have been found in a variety of organisms such as the: rat, mouse (Hbb-b2), African clawed frog (LOC397871), C. elegans nematode (C24A3.4), rainbow trout and tropical clawed frog (Str.8573) Resources this is not appropriate APA format • • • • • • • • • • DOE Genomes: http://www.ornl.gov/sci/techresources/Human_Genome/posters/chromosome/hbb.shtml Carnegie Institution Tutorial: http://carnegieinstitution.org/first_light_case/horn/lessons/sickle.html Gene Card: http://bioinfo.weizmann.ac.il/cards-bin/carddisp?HBB&search=HBB&suff=txt Hemoglobin Architecture (CHIME): http://info.bio.cmu.edu/Courses/BiochemMols/BuildBlocks/Hb.html SSA & Genetics, Background Info: http://chroma.gs.washington.edu/outreach/genetics/sickle/sickle-back.html Your Genes, Your Health, SSA: http://www.ygyh.org/sickle/whatisit.htm SSA & the use of Bioinformatics: http://peptide.ncsa.uiuc.edu/tutorials_current/Sickle_Cell_Anemia/SC2001/ Gene Atlas: http://www.dsi.univ-paris5.fr/genatlas/ SSA Virtual Lab: http://k12education.uams.edu/scvlab/montage.htm Sickle Cell Disease PPT: http://www.scinfo.org/tutorial/Sickle%20Cell/sld001.htm Questions I WILL ask you… • What is the name of the gene that causes this disorder? • What protein does this gene code for? • On what chromosomes (and where) is it found? • How is the mutated protein function different than the original/normal/intended protein function? • How does the difference in protein cause a difference in the cell? • How are cells with mutated proteins different (in structure, in function etc.) that normal cells? • How does the mutated tissue behave differently than normal tissue? • How does the organ system function differently than normal? • What are the symptoms of this disorder? • How can this disorder be prevented? • How can this disorder be treated? • How is this disorder inherited/continued in future generations? • What is the occurrence of this disorder (quantitatively) in the general population? In special (gender, ethnic, geographic) populations? Why?