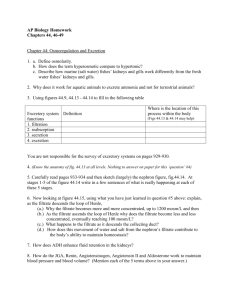
The Urinary System
advertisement

The Urinary System Chapter 15 The Anatomy of the Urinary System The urinary system is composed of – – – – Kidneys Ureters Urinary bladder Urethra. Functions of the Urinary System The urinary system functions to regulate – – – – blood ionic composition blood volume blood pressure pH. Red blood cell production Vitamin D synthesis Excretion of wastes. The Physiology of the Kidneys The story of the urinary system begins with the blood, for it is the blood which is regulated by the action of the kidneys. Our blood contains waste products which we need to eliminate from the body. – The most important of these wastes is a nitrogen-containing compound called urea. Whenever we convert the amino acids of proteins into the energy molecule of glucose we have a problem. What do we do with the nitrogen found in amino acids since glucose does not have nitrogen present? In the conversion process, which occurs in the liver, amino acids are converted into glucose with a resulting byproduct of urea. This compound must then be lost from the body before it accumulates to the level that would be toxic to the body’s tissue. The Physiology of the Kidneys: Glomerular Filtration Blood is sent to the kidney where it passes to the functional units of the kidney called nephrons. The afferent arteriole which carries blood to the nephron has a larger diameter than the efferent arterole which carries blood away from the nephron. This difference in vessel diameter increases the local blood pressure of the nephron. It is this pressure which will help to push substances through the membranous filter (glomerulus) of the nephron. This high pressure pushes substances through the capillary walls of the glomerulus much as a leaky garden hose looses more water when the water pressure is increased. This process is referred to as glomerular filtration. The Physiology of the Kidneys: Glomerular Filtration The filtration slits of the glomerulus are too small to allow the formed elements (cells and cellular components) and proteins of the blood to pass through thus the filtrate is only composed of water, glucose, electrolytes and, of course, urea. This is the reason that presence of cells and protein in the urine may be a cause of concern as it could indicate a kidney disfunction. The Physiology of Kidneys: Tubular reabsorption The filtrate which had been strained through the glomerular membrane will now pass into the proximal convoluted tubule, so called because it is closest tubule to the glomerulus (proximal) and that it is coiled (convoluted). Glucose readily passes through the filtration slits of the glomerulus and so is present within the filtrate which will ultimately be the urine lost from the body. Why then do we consider presence of glucose in urine to be an indication of non-normal functioning of the body (diabetes)? After all, shouldn’t glucose normally be found in the urine if it is found in the filtrate of the kidney tubules? The Physiology of Kidneys: Tubular reabsorption Since we go through so much trouble to obtain glucose (we obtain food, we cook food,we eat food, we digest food, we absorb food) it would be a very inefficient process for our body to simply then loose it to the outside. So our kidney nephrons retrieve glucose from the filtrate as it passes along the proximal convoluted tubule. Along with active transport of glucose across the proximal convoluted tubule lining other important substances such as sodium ions and chloride ions are also transported across to be returned to the blood. This process is referred to as tubular reabsorption. The Physiology of Kidneys: Concentration of the Filtrate When the filtrate reaches the loop of Henle it has now lost many of its solutes and has become more dilute. As the filtrate passes down the descending limb of the loop of Henle it passes through increasingly greater salt content in the surrounding tissue. This tends to pull water out of the renal tubule due to osmosis. Thus the filtrate becomes more and more concentrated due to the loss of water to the surrounding tissues. The Physiology of Kidneys: Concentration of the Filtrate As the filtrate passes up the ascending limb of the Loop of Henle the walls of the ascending limb is impermeable to water thus water is unable to pass back into the tubule even though on the return trip to the cortex of the kidney it is passing through tissue with less and less saltiness. This process represents urine concentration. The Physiology of Kidneys: Tubular Secretion Fluid leaving the ascending limb of the loop of Henle now passes through the distal convoluted tubule where substances are directly transferred from the surrounding capillaries into the renal tubule. This process is referred to as tubular secretion. Further concentration of filtrate The end of the kidney nephron brings us to the collecting ducts which collect the filtrate from hundreds of nephrons. Here we have a second chance to concentrate our urine. If antidiuretic hormone (ADH) is produced due to us not drinking enough water, its presence will open channels which allow water to go out into the surrounding kidney tissue as the collecting duct passes into the saltier medulla of the kidney. Micturition From the collecting duct the filtrate which now can be considered urine, passes into the minor calyx, the major calyx, the renal pelvis, and the ureter, in order to pass and be stored in the urinary bladder. It will remain here until we feel we need to er...ah...ahem...powder our noses. (I really mean the process of urination or micturition.) Fluids and Electrolytes Our body has a very delicate balance of its components. Fluid from our extracellular compartment are able to enter our intercellular compartment and vise versa. This movement of water from outside the cell to inside the cell is controlled by relative concentrations of electrolytes in the various fluid compartments. The relative concentration of the electrolytes in our various fluid compartments is illustrated in a diagram in your textbook. Their functions within the body are described in your text narration. Acidosis and Alkalosis For normal functioning of our cellular enzymes we need to have normal pH (acidity) in our fluids. We have a variety of buffer systems which tend to keep our acids and bases in balance (homeostasis). If our blood becomes too acidic the condition is called acidosis. If our blood becomes too basic the condition is called alkalosis. We can go into respiratory acidosis if we hypoventilate (lack of breathing will allow for the accumulation of carbon dioxide in our blood which reacts with water to form carbonic acid). Respiratory alkalosis is caused by hyperventilation (breathing too rapidly leads to a loss of too much carbon dioxide which leads to our pH going to high). Acidosis and Alkalosis Medications can lead to these pH problems as well. A person who seeks to commit suicide by ingesting a bottle of aspirin (salicylic acid) is creating acidosis and will die due to enzyme malfunction unless appropriate medical attention is delivered. A nursing school instructor once explained it to me this way. “If you don’t give the appropriate medication to a patient it is like being on the loosing team of a baseball game. When you hit the ball and begin to run around the baseball diamond, those bases are going to kick your ass...ids.”