File
advertisement

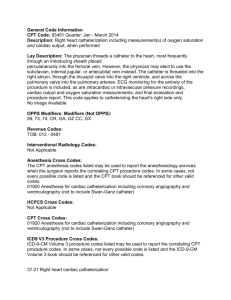
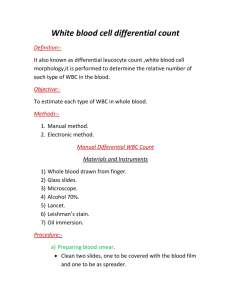
Cardiovascular: Decreased cardiac output r/t congestive heart failure and myocardial infarction Pt. has a history of CHF and an AV sequential pacer that, when investigated, was found to only be pacing the right ventricle. When pt. presented to ED his BP was 130/80 and he had <30 mL or urine output/hour for the first few hours that he was at EAMC. The pt. was also confused, disoriented, and his extremities were edematous. Interventions: Assess for signs and symptoms of decreased CO. Implement measures to improve CO such as: place pt. in Semi-Fowler’s position; administer diuretics, beta-blockers, and positive inotropes per MD order Goals: Pt. will have improved cardiac output AEB: BP within normal range for pt., usual mental status, urine output of at least 30mL/hour, and a decrease in edema. Goals partially met Neurological: Altered mental status Pt. is confused upon awakening but slowly becomes more oriented. Pt. is oriented to person and place but cannot recall numbers such as his phone number or address. Pt.’s daughter states that this is unusual for pt. Interventions: Assess for and monitor acute changes in cognition, treat underlying cause of altered mental status (decreased cardiac output and impaired gas exchange), use orientation techniques such as placing a clock and calendar in pt.’s room, explain hospital routines and procedures slowly and in simple terms Goals: Pt. will be orientated to person, place, and time. Pt. will demonstrate return of mental status to baseline. Goals not yet met Medical Diagnosis: Myocardial Infarction, Altered Mental Status Primary Nursing Diagnosis: Decreased cardiac output Respiratory: Impaired gas exchange r/t decreased pulmonary tissue perfusion associated with decreased cardiac output Pt.’s RR was 40 when he was admitted to the ED but they are now in the high 20’s to low 30’s. The pt. was extremely SOB upon arrival. He also has diminished breath sounds with coarse crackles over the lower lung fields. Pt.’s pulse oximetry is around 96% on 4L O2 via NC. His O2 sat’s drop significantly when the NC is removed. The pt. still has some confusion and disorientation. Interventions: Assess for signs and symptoms of impaired gas exchange and implement measures to improve gas exchange such as: perform actions to improve cardiac output, place client in a SemiFowler’s position, instruct client to use incentive spirometer Q2H, and maintain O2 therapy as ordered. Goals: Pt. will experience improved gas exchange AEB: normal rate, rhythm, and depth of respirations; pt. states a decrease in dyspnea; improved breath sounds; usual mental status; and pulse oximetry results within normal range. Goals partially met Past Medical History: Pt. has a history of CHF, type II diabetes, has an AV sequential pacemaker (after investigation it was found that the pacemaker was only pacing the right ventricle), and a pelvic CT revealed a renal mass that is suspicious of renal carcinoma Genitourinary: Risk for infection r/t urinary catheter Pt. has had a Foley catheter in place for 2 days. Pt’s temp is 96.7° F, WBC count is 10.1. Interventions: Follow EAMC protocol for catheter and perineal care, monitor urinary output Q2H, monitor pt.’s temp. and WBC count Goals: Pt. will remain free of infection AEB: normal temp. and WBC count within normal limits. Goals partially met Present Illness: Pt. was discharged from EAMC on 9/28 after an exacerbation of his CHF. Late on 9/28, the pt. became short of breath and was brought to Clay County hospital which then transferred him to EAMC. At the time of admission, pt.’s RR was 40, BP was 130/80, K was 6.3, BNP > 5000, and troponin was 1.9 Gastrointestinal: Risk for constipation Pt. has not had a BM since admission to the ICU. Pt. does have a soft, rounded abdomen and has been passing gas. Pt. also has limited mobility r/t his heart catheterization earlier today. Interventions: Provide pt. with a high fiber diet, administer stool softeners per MD order, continue to palpate pt.’s abdomen for distention and auscultate for bowel sounds. Goals: Pt. will not experience constipation AEB: pt. maintains passage of soft, formed stool Q1-2 days without straining; absence of abdominal distention and pain. Goals not yet met Integumentary: Risk for infection Pt. had a heart catheterization performed earlier today. Pt’s temp is 96.7° F, WBC count is 10.1. Interventions: Assess for and report signs of site infection such as: fever, redness, swelling, and pain at the site; unusual site drainage; and an elevated WBC count. Perform actions to reduce introduction of pathogens to the site by: maintaining good hand hygiene and instructing pt. to refrain from touching site Goals: Pt. remains free from infection at the catheterization site AEB: absence of fever, heat, redness, and pain at the site; usual drainage from site; and WBC count within normal range. Goals partially met