PBL summary week 28
advertisement

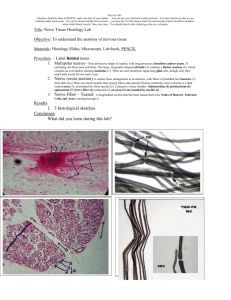
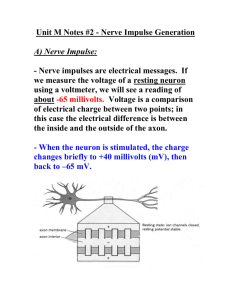
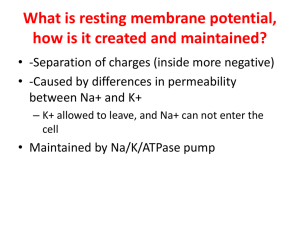
Outline of Key Learning Areas related to PBL Case Week 28 – ‘Get a grip’ Relevant Symptoms (incl. relevant negatives) 27 year old male ‘Tony’ presented to ED with a 10 cm laceration to R medial forearm Complains of numbness and difficulty moving fingers Other Significant History Carpenter Right handed Had tetanus shot in high school Examination and Signs Initially abusive, so examination delayed for an hour Clean wound, no contamination visible Negative signs: Unable to adduct or abduct fingers of R hand Unable to flex middle, ring and little fingers No reaction to pinprick stimuli on little and ring fingers Positive signs: Shoulder bruised and tender Peripheral circulation normal. Provisional Diagnosis Differential Diagnoses Severed R ulnar nerve Severed R flexor tendons Risk Factors and Aetiology Intoxication Young male Key Basic Science Learning Issues 1) Anatomy 3) Microbiology Tetanus Caused by Clostridium tetani, grampositive obligate anaerobic bacteria • Spread by deep wounds, leading to invasion of bacteria into deep tissue • Incubation period: ~ 8 days • Pathogenesis of infection Bacteria release endotoxin 4) Pathophysiology Nerve injury Segmental Demyelination Schwann cell dysfunction or myelin sheath damage, with the axon remaining intact Degenerating myelin is initially engulfed by Schwann cells and later by macrophages Axonal Degeneration Primary destruction of the axon and secondary destruction of the myelin sheath Wallerian degeneration: degeneration of a nerve fibre from the point of damage forwards Triggered by severe nerve injury – trauma, transaction, toxins, inflammation, demyelination Local Schwann cells break down myelin and engulf axonal fragments Nerve damage can also lead to degeneration of cells that share synapses with the injured cell – anterograde or retrograde transneuronal Neuron regeneration Peripheral Nervous System Axonal sprouting occurs at the proximal stump within 96 hours Axon eventually reaches target, and functional connection(e.g. NMJ) is reformed Axonal growth proceeds at a rate of 1mm/day Central Nervous System CNS neurons are post-mitotic so are not able to divide or regenerate CNS axons are capable of regenerating, but the surrounding environment is inhibitory Glial cells form scar tissue and secrete inhibitory factors, preventing axonal growth Astrocytic proliferation, activation of microglia, inflammation, and invasion of immune cells also contribute to a poor environment for regeneration Treatment is currently focused on rehabilitation rather than repairing injury 2) Physiology/Biochemistry Mechanism of muscle contraction Ulnar claw Interossei do DAB and PAD – and work with lumbricles to extend the PIP and DIP while flexing the MCP Extensor digitorum tendon extends down dorsum of hand – attaches with lumbricles and interossi. Pincer/writing position = interosseus muscle action – flexion of proximal and extension of distal two. Without this you get the opposite – extension MCP and flexion of DIP and PIP This will compromise his ability to work as a carpenter – pincer grip to power grip. He also appears to have muscle wasting Resting muscle tone in dorsal and palmar interossei is gone The paired muscles on the other side of the hand are unopposed Complex regional pain Acute and dramatic autonomic effects persist beyond expected limits Prevalent in distal extremities – affects pain perception in response to smaller stimuli. It may also cause hyper-inflated sweat response, hirsutism, abnormal control of vasculature. Absence of sweating ANS damage – sympathetic nerve input is compromised Mechanism of nerve conduction Steps in the Generation of an Action Potential 1. Resting state (before stimulation) Na+ and K+ voltage- gated ion channels (primarily located in axon hillock and axon) are closed 2. Beginning of stimulation Na + arrives at axon hillock, depolarizing the membrane at that point (steadily rising LP). For anything more to happen, this LP must rise to a critical voltage called the threshold (about 60mV) in order to open voltage gates at trigger zone. 3. Depolarisation Phase: At threshold the neuron “fires” producing an AP. Here voltage-gated Na + gates open quickly while K+ gates open more slowly. Positive feedback were more and more Na+ gates open, causing membrane voltage to rise rapidly. 3. Repolarisation Phase: As rising MP passes 0 mV, Na+ gates begin to slowly close and by time they are fully closed the voltage peaks at +35 mV. Membrane now positive on inside and negative on out (reversed to RMP). By this peak, the Na+ gates are closed and the slow K+ gates are fully open and there is an efflux of K+ as they are repelled by the positive ICF. This causes the repolarisation (shifting back to negative numbers) 4. Hyperpolarisation: K+ gates stay open longer than Na+ gates, so the amount of K+ leaving is greater than amount of Na+ that entered. Thus membrane voltage drops 1-2 mV. This is restored by Na+/K+ pump and simple diffusion of K+ back into the cell. Continuous conduction occurs along unmyelinated axons. It is a step=by-step depolarization where the resulting depolarization excites voltage-regulated gates immediately distal to the AP Saltatory conduction occurs in neurons that are myelinated. These neurons have gaps in between the myelin sheaths called Nodes of Ranvier. These gaps contain the highest concentration of voltage-gated Na+ and K+ channels. Therefore, impulse jumps from node to node. Functional features of forearm manual anatomy Free Motion Power grasping Precision handling Pinching Investigations and Results Other possible investigations 1) Blood tests 1) Blood tests 2) Imaging X-rays of upper limb including shoulder showing no fracture or foreign body 2) Imaging X-ray would show glass it reflects the rays 3) Other 3) Other Management Plan Problem Goal/desired outcome Method (incl. patient actions) Severed ulnar nerve and flexor tendons Damaged artery Wound thoroughly debrided before suturing Surgery Resources/health professional s involved Surgeon… Small artery ligated Hand vulnerable while regeneration occurring Relief of tensile load upon tissues undergoing repair. You don’t want to challenge these tissues by extra loading Forearm and hand immobilized in a brace in the flexed position Potential exposure to C. tetanii Immunity Inability to use dominant hand Rehabilitation Financial strain – four dependent children Medications Financial aid Return to work facilitated Mode of action Vaccination administered Stimulation of neuromuscular pathways through passive and active exercises Centrelink /Community assistance Side effects Antibiotics Prevent spread of bacterial infection Analgesia Various, previously outlined Saline administered intravenously Blood loss replacement (?) Occupational therapist Physiotherapist GP Rehab team Social worker Any specific monitoring required? Other Psychosocial/ethical/legal/patient-centred considerations Depression common following disabling injury – inability to function or work as previously able Mental assessment + 12 months still ulnar claw and weakened grip in R hand – after 12 months you’re unlikely to get much more improvement PPH implications Tetanus immunisation programme 1. Infancy: DTPw (diphtheria, tetanus, pertussis) is given at 2 months with boosters at 4, 6 and 18 months 2. Childhood: the DTPw vaccination is given before school entry (4-5 years) 3. Adulthood: ADT (adult tetanus/diphtheria) is given before leaving school and once every 10 years If patient hasn’t had received immunisations, and exposure to bacterium is considered a possibility, passive immunity should be administered via immunoglobulin. Alcohol and injury 1 in 5 Australians drink at short-term/high risk (binge drinking) levels at least once a month (this goes to about 1 in 4 in young adults aged 2029) Approximately 10-18% of all injured patients arrive at the emergency room due to alcohol-related causes Most are males under 35 (mostly late teens/young adults) of middle socioeconomic status Alcohol-related injuries mostly occur in public places, during leisure activities and intentionally caused by a friend/acquaintance Responsible for 5% of male injuries and 1.5% injuries in females Most common cause of death due to intoxication is road crash and among chronic condition alcohol-related liver cirrhosis accounts for majority of deaths Prevention Ineffective Strategies (though often popular) Voluntary Industry Codes e.g. of bar practice Alcohol education and persuasion Public service messages Non-specific warning labels Promoting alternativeness e.g. alcohol free activities Designated drivers and ride services Effective Strategies Regulating physical availability of alcohol – restricting hours and days of sale, restriction on density of outlets, restricting availability by alcohol strength, sales bans (e.g. cask wines and cask fortified wines in indigenous population), Minimum legal purchase age Government monopoly of retail sales Increase taxes and pricing for alcohol Drink driving countermeasures – lower BAC limits, RBT’s, license suspension Treatment and intervention for hazardous drinkers – can be at the level of health setting and workplace. Pharmacotherapy has also been proven to be effective Resources used/discovered