here - Northland DHB
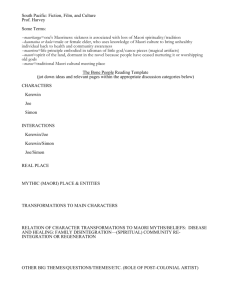
advertisement

Guide for proposers Proposal name Summary of proposal in 150 words including rationale, aims, costs and benefits. Population Health Criteria Amount Existing/ expanded service New service Type of funding Pilot project/ service If sustainable, for how long? One Off Sustainable Requirements (address any or all as appropriate) Reducing inequities – Maori All else being equal, a proposal that is targeted to and delivered by Maori is given a higher score. A mainstream service that serves many Maori patients or clients but doesn’t specifically target the service to their needs will not score as highly. Reducing inequities – other vulnerable populations All else being equal, a proposal that is targeted to other vulnerable groups and delivered by the other vulnerable group is given a higher score. A mainstream service that serves many other vulnerable patients or clients but doesn’t specifically target the service to their needs will not score as highly. Volume The number of users or patients expected to benefit from the proposal annually. A service which benefits more people is given a higher score. Early intervention Likelihood the proposal will promote a wellness model and achieve ‘upstream’ changes. These might be: Primary prevention e.g. in the context of rheumatic fever: throat swabbing to avoid/detect disease Secondary prevention e.g. in the context of rheumatic fever: penicillin injections to prevent recurrences Tertiary prevention e.g. in the context of rheumatic fever: heart valve replacements, lifestyle changes. Benefit/ individuals and groups This assesses health benefits or outcomes identified in the proposal accrued by individuals and their family and carers due to the intervention. Benefits should be quantified if possible including evidence of quantifiable benefits. Effects on health service demand Proposals should identify any effects on demand on other health services. A proposal which impacts on other health services positively is given a higher score. Intersectoral Collaboration Patient Experience Type of proposal The proposal should identify any collaboration with services provided in other sectors (non-health). A proposal which demonstrates collaboration with other sectors to achieve better outcomes is given a higher score. Service design How the proposed initiative will improve: integration models of care scope of practice clinical pathways. Acceptability to stakeholders Demonstrates, at this initial stage, acceptability to (not just engagement with) stakeholders, including consumers, providers and other agencies (health and intersectoral). Evidence of effectiveness All else being equal, a proposal for a service with strong evidence of effectiveness will be given a higher score. Access – geographical A proposal that improves geographical access (that is, provide services closer to home) is given a higher score. Access – cost for patient/ user A proposal that reduces costs to the patient or user is given a higher score. Access – timeliness A proposal which makes interventions more timely is given a higher score. Cultural safety A proposal which demonstrates cultural safety in the provision of services is given a higher score. Timing of benefit A proposal identifying that health benefits or outcomes will occur more quickly will receive a higher score. Cost & productivity Quality, safety improvements A proposal which achieves significant quality and/or safety improvements is given a higher score. Cost savings Interventions with larger cost savings or offsets are scored higher than those with low cost savings or offsets. Timing of cost savings A proposal whose savings occur more quickly will receive a higher score. Cost/ person Lower-cost interventions are scored more highly than costly interventions. Efficiency, productivity A proposal that identifies larger cost efficiencies or productivity gains will score more highly. Project Initiation Document A Project Initiation Document must accompany the proposal. This criteria assesses how complete and robust it is. It is either considered adequate or inadequate. Other critical criteria Other factors that have not been captured in the standard set of criteria above, but are considered by the SIF PG to be critical in judging the merits of the proposal. The SIF PG will describe these. Prioritisation proposal form (to be completed by Proposer) Proposal name Summary of proposal in 150 words including rationale, aims, costs and benefits. Criteria Population Health Reducing inequities- Maori Reducing inequities – other vulnerable populations Volume Early intervention Benefit/ individuals and groups Effects on health service demand Intersectoral Collaboration Service design Evidence of effectiveness Patient Experience Access – geographical Access – cost for patient/ user Access – timeliness Cultural safety Timing of benefit Quality, safety improvements Acceptability to stakeholders Cost & productivity Cost savings Timing of cost savings Cost/ person Efficiency, productivity Type of proposal Amount Existing/ expanded service New service Type of funding Pilot project/ service If sustainable, for how long? Requirements (address any or all as appropriate) One off Sustainable Service Priority Assessment Tool (used by the Prioritisation Group) Summary of proposal in 150 words including rationale, aims, costs and benefits. Type of proposal Existing/ expanded service New service Type of funding Pilot project/ service If sustainable, for how long? Criteria Reducing inequities – Maori Population Health Patient Experience n/a 0 1 22 3 4 Service with no targeting for Maori Service with little targeting to Maori Service mostly targeted to Maori Service fully targeted to Maori Service fully targeted to Maori and Maoriprovided Untargeted service Untargeted service but serving a high need, poor health population Some targeting to those with poor health and high need Fully targeted to those with the poor health and high need Fully targeted to those with poor health and high need and engages this population in service planning and/or delivery Volume Not quantified <100 100-999 1,000-5,000 >5,000 Early intervention Not quantified Minimal Mixed Predominant Solely Benefit/ individuals and groups Little, if any, direct benefit Some unquantifiable benefit to a small number of people Some quantifiable benefit to a small number of people Significant unquantifiable benefit to a large number of people Significant quantifiable benefit to a large number of people Effects on health service demand Negative Neutral Mildly positive Moderately positive Significantly positive Intersectoral Collaboration Not at all Minimal Moderate based on existing intersectoral relationships Significant based on existing intersectoral relationships Significant and establishes a new collaborative relationship Service design Not at all Minimal Some in one of the four areas of redesign Significant in one or two of the four areas of redesign Significant in three or four of the areas of redesign No evidence or consensus of clinical opinion Consensus of clinical opinion but no evidence Some evidence Good international evidence Good New Zealand evidence Accessibility – geographical Not quantified May have minimal impact Will have some impact May have high impact Will have high impact Access – cost for patient/ user Not quantified May have minimal impact Will have some impact May have high impact Will have high impact Access – timeliness Not quantified May have minimal impact Will have some impact May have high impact Will have high impact Not May have minimal impact Will have some impact May have high impact Will have high impact >10 years 5-10 years 3-4 years 1-2 years <1 year Quality/safety improvements Not quantified May have minimal impact Will have some impact May have high impact Will have high impact Acceptability to stakeholders Not shown Minimal Moderate High Stakeholder driven Evidence of effectiveness Cost & productivity One Off Sustainable Scoring criteria N/a Reducing inequities – other vulnerable populations Amount n/a Cultural safety Timing of benefit Don’t know Cost savings n/a Costs will increase or are not quantified Neutral effect Up to $100k net cost reduction Up to $500k net cost reduction >$500k net cost reduction Timing of cost savings n/a >10 years 6-9 years 3-5 years 2 years Within 1 year Cost/ person >$5,000 per person $1,000-$5,000 per person $100-$999 per person $10-99 per person $0-9 per person Efficiency, productivity Not quantified Minimal Some Moderate High Other critical criteria Score Proposal name