Pharmacotherapy in Psychiatry
advertisement

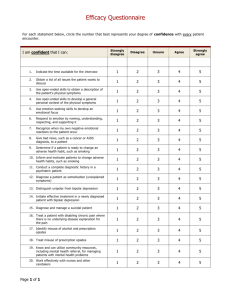
Pharmacotherapy in Psychiatry Depression Schizophrenia Bipolar disorders Contents Schizophrenia and antipsychotics Depression and antidepressants Bipolar disorders and mood stabilizers Schizophrenia and antipsychotics Schizophrenia Characterized by psychosis, hallucinations, delusions, cognitive defects, occupational and social dysfunction Chronic psychotic illness Episodic exacerbations and remissions with residual symptoms Complete remission is not common Schizophrenia Epidemiology Lifetime prevalence is 1% in United States Onset in late teens or early 20s in males; sometime later in females Suicide rate comparable to depressive illness (approx 10%) Schizophrenia Etiology Exact etiology unknown Genetic predisposition Intrauterine, birth or postnatal complications Viral CNS infections Environmental stressors (biochemical or social) No evidence of association with poor parenting Schizophrenia Pathophysiology No consistent neuropathology or biomarkers for schizophrenia ? Increased dopamine in mesolimbic pathways causes delusions and hallucinations ? Dopamine deficiency in mesocortical and nigrostriatal pathways causes negative symptoms (apathy, withdrawal) Hallocinogens produce effect through action on 5-HT2 receptors Schizophrenia Positive symptoms Hallucinations Delusions Disordered thinking Disorganized speech Combativeness Agitation Paranoia Negative symptoms Social withdrawal Emotional withdrawal Lack of motivation Poverty of speech Blunted affect Poor insight Poor judgement Poor self-care Schizophrenia Antipsychotics Typical / Conventional antipsychotics Atypical antipsychotics Typical / conventional antipsychotics Chlorpromazine (Largactil®) Flupenthixol (Fluanxol®) Haloperidol (Serenace®, Haldol®) Pericyazine (Neulactil®) Pimozide (Orap®, Orap Forte®) Sulpiride (Dogmatil®) Thioridazine (Melleril®) Trifluoperazine (Stelazine®) Thiothixene (Navane®) Typical / conventional antipsychotics Refers to agents introduced in US before 1990 Also known as “Dopamine receptor antagonists” Pharmacologic activity at blocking central dopamine receptors (esp. D2 receptors) “Neuroleptics” Due to tendency to cause neurologic Adverse effects “Major tranquilizers” Inappropriate as these agents (esp. high potency) can improve psychosis without sedating or making patients tranquil Typical / conventional antipsychotics Dopamine receptors in various tracks Track Origin Innervations Function Antipsychotic effect Mesolimbic Midbrain, Ventral tegmental Limbic structure, nucleus accumbens Emotional and intellectual Hallucinations, deulsions, disordered cognition Mesocortical Ventral tegmental Frontal cortex Nigrostriatal Substantia nigra Basal ganglia Extrapyramidal system movement Motor symptomatology Tuberoinfundubular Hypothalamus Pituitary gland Plasma prolactin levels Regulate endocrine functions Typical / conventional antipsychotics Mechanism of action Blocks receptors for dopamine, acetylcholine, histamine and norepinephrine Current theory suggests dopamine2 (D2) receptors suppresses psychotic symptoms All typical antipsychotics block D2 receptors Close correlation between clinical potency and potency as D2 receptor antagonists Typical / conventional antipsychotics Properties Effective in reducing positive symptoms during acute episodes and in preventing their reoccurrence Less effective in treating negative symptoms Some concern that they may exacerbate negative symptoms by causing akinesia Higher incidence of EPS / sedation / anticholinergic Adverse effects Typical / conventional antipsychotics Potency All have same ability to relieve symptoms of psychosis Differ from one another in terms of potency i.e. size of dose to achieve a given response When administered in therapeutically equivalent doses, all drugs elicit equivalent antipsychotic response Typical / conventional antipsychotics Low potency Chlorpromazine, thioridazine Medium potency Perphenazine High potency Trifluoperazine, thiothixene, fluphenazine, haloperidol, pimozide Typical / conventional antipsychotics Potency Drug Low Equiv oral dose (mg) EPS Sedation Anticholinergic s/e Chlorpromazine 100 Moderate High Moderate Pericyazine NA Low High Low Thioridazine 100 Low High High Moderate Perphenazine 10 Moderate Moderate Low High Trifluoperazine 5 High Low Low Thiotheixene 2 High Low Low Fluphenazine 2 High Low Low Haloperidol 2 High Low Low Pimozide 0.5 High Moderate Moderate Sulpiride 200 Low Moderate Low Typical / conventional antipsychotics Comparison of representative antipsychotics Drug Advantages Disadvantages Chlorpromazine Generic, inexpensive Many adverse effects (esp. autonomic) Thioridazine Slight EPS, generic Cardiotoxicity (QT prolongation) Fluphenazine Generic, depot available (?) increased tardive dyskinesia Thiothixene (?) decreased tardive dyskinesia Uncertain Haloperidol Generic, injection and Prominent EPS depot A/V, few autonomic s/e Typical / conventional antipsychotics Receptor blockade and Adverse effects Receptor type Consequence of blockade D2 dopaminergic Extrapyramidal symptoms; prolactin release H1 histaminergic Sedation Muscarinic cholinergic Dry mouth, blurred vision, urinary retention, constipation, tachycardia Alpha1-adrenergic Orthostatic hypotension; reflex tachycardia 5-HT2 serotonergic Weight gain Typical / conventional antipsychotics Adverse effects Extrapyramidal symptoms (EPS) Early reactions – can be managed with drugs Acute dystonia Parkinsonism Akathisia Late reaction – drug treatment unsatisfactory Tardive dyskinesia (TD) Early reactions occur less frequently with low potency drugs Risk of TD is equal with all agents Typical / conventional antipsychotics Adverse effects Acute dystonia Develops within a few hours to 5 days after first dose Muscle spasm of tongue, face, neck and back Oculogyric crisis (involuntary upward deviation of eyeballs) Opisthotonus (tetanic spasm of back muscles, causing trunk to arch forward, while head and lower limbs are thrust backwards) Laryngeal dystonia can impair respiration Management Anticholinergics (Benztropine, diphenhydramine IM/IV) Lower or split dosing Switch agent Add scheduled benztropine / diphenhydramine with antipsychotic Typical / conventional antipsychotics Adverse effects Parkinsonism (neuroleptic induced) Occurs within first month of therapy Bradykinesia, mask-like facies, drooling, tremor, rigidity, shuffling gait, cogwheeling, stooped posture Shares same symptoms with Parkinson’s disease Management Centrally acting anticholinergics (scheduled benztropine / diphenhydramine / benzhexol with antipsychotics) and amantadine Avoid levodopa as it may counteract antipsychotic effects Switch to atypical antipsychotics for severe symptoms Typical / conventional antipsychotics Adverse effects Akathisia Develop within first 2 months of therapy Compulsive, restless movement Symptoms of anxiety, agitation Management Beta blockers (propranolol) Benzodiazepines (e.g. lorazepam) Anticholinergics (e.g. benztropine, benzhexol) Reduce antipsychotic dosage or switch to low potency agent Typical / conventional antipsychotics Adverse effects Tardive dyskinesia (TD) Develops months to years after therapy Involuntary choreoathetoid (twisting, writhing, worm-like) movements of tongue and face Can interfere with chewing, swallowing and speaking Symptoms are usually irreversible Typical / conventional antipsychotics Adverse effects Tardive dyskinesia (TD) Management Some manufacturers suggest drug withdrawal at earliest signs of TD (fine vermicular movements of tongue) may halt its full development Gradual drug withdrawal (to avoid dyskinesia) Use lowest effective dose Atypical antypsychotic for mild TD Clozapine for severe, distressing TD Inconsistent results with Diazepam, clonazepam, valproate Propranolol, clonidine Vitamin E Typical / conventional antipsychotics Other Adverse effects Neuroleptic malignant syndrome (NMS) Rare but serious reaction, 0.2% of patients on neuroleptics High fever, autonomic instability, mental status changes, leaden rigidity, elevated CK, WBC, myoglobinuria Management Discontinue antipsychotic Paracetamol for hyperthermia IV fluids for hydration Benzodiazepines for anxiety Dantrolene for rigidity and hyperthermia Bromocriptine for CNS toxicity Typical / conventional antipsychotics Other Adverse effects Neuroleptic malignant syndrome (NMS) After symptom resolution Some suggest to wait for at least 2 weeks before resuming Use lowest effective dose Avoid high potency agents Consider atypical antipsychotics However, NMS has been reported from patients taking clozapine, risperidone, olanzapine and quetiapine Typical / conventional antipsychotics Other Adverse effects Prolactinemia D2 receptor blockade decreases dopamine inhibition of prolactin Results in galactorrhea, amenorrhea, loss of libido Managed with bromocriptine Sedation Administer once daily at bedtime Seizures Haloperidol has a lower risk of seizures Anticonvulsants (beware or possible interaction with antipsychotic) Atypical antipsychotics Refers to newer agents Also known as “Serotonin-dopamine antagonists” Postsynaptic effects at 5-HT2A and D2 receptors Atypical antipsychotics Amisulpiride (Solian®) Quetiapine (Seroquel®) Ziprasidone (Zeldox®) Risperidone (Risperdal®) Olanzapine (Zyprexa®) Clozapine (Clozaril®) Aripiprazole (Abilify®) Atypical antipsychotics Mechanism of action Similar blocking effect on D2 receptors Seem to be a little more selective, targeting the intended pathway to a larger degree than the others Also block or partially block serotonin receptors (particularly 5HT2A, C and 5HT1A receptors) Aripiprazole: dopamine partial agonist (novel mechanism) Atypical antipsychotics Properties Available evidence to show advantage for some (clozapine, risperidone, olanzapine) but not all atypicals when compared with typicals At least as effective as typicals for positive symptoms May be more efficacious for negative and cognitive symptoms (still under debate) Atypical antipsychotics Properties Less frequently associated with EPS More risk of weight gain, new onset diabetes, hyperlipidemia Novel agents, more expensive Atypical antipsychotics Potency All atypical antipsychotics are equally effective at therapeutic doses Except clozapine Most effective antipsychotic For resistant schizophrenia 2nd line due to life-threatening side effect Atypical antipsychotics Relative receptor-binding of atypical antipsychotics Drug D1 D2 5-HT2 1 Clozapine ++ ++ +++ Risperidone - +++ +++ +++ - Olanzapine ++ ++ +++ ++ Quetiapine - + ++ +++ + + Ziprasidone +/- ++ +++ ++ - + Aripiprazole + +++ ++ ++ - + M1 H1 +++ +++ + + +++ ++ Atypical antipsychotics Comparison of representative atypical antipsychotics Drug Advantages Disadvantages Clozapine For treatment-resistant cases, little EPS Risk of fatal agranulocytosis Risperidone Broad efficacy, little or no EPS EPS and hypotension at high at low doses doses Olanzapine Effective with positive and negative symptoms, little or no EPS Weight gain Quetiapine Similar to risperidone, maybe less weight gain Dose adjustment with associated hypotension, bd dosing Ziprasidone Perhaps less weight gain than clozapine, Inj A/V QT prolongation Aripiprazole Less weight gain, novel mechanism potential Uncertain Atypical antipsychotics Relative incidence of Adverse effects Drugs Sedatio n EPS Anticholinergic Orthostasis Seizure Prolactin elevation Weight gain Clozapine ++++ + ++++ ++++ ++++ 0 ++++ Risperidone +++ + ++ +++ ++ 0 to ++++ ++ Olanzapine +++ + +++ ++ ++ + +++ Quetiapine +++ + ++ ++ ++ 0 ++ Ziprasidone ++ + ++ ++ ++ 0 + Aripiprazole ++ + ++ ++ ++ 0 + Atypical antipsychotics 1st line atypical antipsychotics All atypicals except clozapine NICE recommendations Atypical antipsychotics considered when choosing 1st line treatment of newly diagnosed schizophrenia Treatment option of choice for managing acute schizophrenic episode Considered when suffering unacceptable Adverse effects from a conventional antipsychotic Changing to an atypical not necessary if typical controls symptoms adequately and no unacceptable Adverse effects Atypical antipsychotics 2nd line atypical antipsychotic Clozapine Most effective antipsychotic for reducing symptoms and preventing relapse Use of clozapine effectively reduce suicide risk 1% risk of potentially fatal agranulocytosis Acute pronounced leukopenia with great reduction in number of neutrophil NICE recommendations Clozapine should be introduced if schizophrenia is inadequately controlled despite sequential use of 2 or more antipsychotic (one of which should be an atypical) each for at least 6-8 weeks) Atypical antipsychotics Clozapine BNF 52 (September 2006) Leucocyte and differential blood count normal before starting Monitor counts Q week for 18 weeks, then at least Q 2 weeks after 1 year At least Q 4 weeks after count stable for 1 year (for 4 more weeks after discontinuation) If leucocyte count < 3000/mm3, or if ANC < 1500/mm3, discontinue immediately and refer to hematologist Patient should report immediately symptoms of infection, esp. flu-like illness (fever, sore throat) Atypical antipsychotics Clozapine Rare cases of myocarditis and cardiomyopathy Fatal Most commonly in first 2 months CSM recommendations Physical exam and medical history before starting Persistent tachycardia esp. in first 2 weeks should prompt observation for cardiomyopathy If myocarditis or cardiomyopathy, stop clozapine Inform patients for unexplained fatigue, dyspnea, tachypnea, chest pain, paipitation and ask them to report these signs and symptoms immediately Atypical antipsychotics Clozapine Contraindication History of clozapine-induced agranulocytosis Bone marrow suppression On myelosuppressive drugs Caution Seizure disorders Diabetes Antipsychotic oral-dispersible and solution preparations Oral-dispersible preps available for 2 atypicals Risperidone (Risperdal Quicklet®) Olanzapine (Zyprexa Zydis®) Carefully peel off packing, allow tablet to dissolve on tongue and swallow Do not break the tablet Some may be dispersed in fluids (consult manufacturer literature) Solutions available for 1 typical Haloperidol (Haldol® drops) 1 atypical Risperidone (Risperdal® solution) Very concentrated, avoid from contact with skin (dermatitis) Antipsychotic injections Available for 2 typicals Chlorpromazine (Largactil®) Haloperidol (Haldol®) 2 atypicals Olanzapine (Zyprexa®) Ziprasidone (Zeldox®) Useful for acutely agitated patients Antipsychotic depot injections Available for 4 typicals Haloperidol decanoate (Haldol Decanoate®) Fluphenazine decanoate (Modecate®) Flupenthixol (Fluanxol®) Zuclopenthixol (Clopixol Depot®) 1 atypical Risperidone (Risperdal Consta®) Used for chronic illness and history of noncompliance Trial of oral meds first to assess tolerability Non-antipsychotic agents Benzodiazepines Useful in some studies for anxiety, agitation, global impairment and psychosis Schizophrenic patients are prone to BZD abuse Limit use to short trials (2-4 weeks) for management of severe agitation and anxiety Lithium Limited role in schizophrenia monotherapy Improve psychosis, depression, excitement, and irritability when used with antipsychotic in some studies Non-antipsychotic agents Carbamazepine Weak support when used alone and with antipsychotic Alters metabolism of antipsychotic NOT to be used with clozapine (risk of agranulocytosis) Valproate Concurrent administration with risperidone and olanzapine resulted in early psychotic improvement in recent investigation Propranolol Research showed improvement in chronic aggression Treat aggression or enhance antipsychotic response Reasonable trial 240mg/day Antipsychotics in schizophrenia Selection of typical antipsychotics Equally efficacious Chosen by side effect profile Atypical antipsychotics may be appropriate if Adverse effect is a particular concern Additional benefits for negative and cognitive symptoms required Clozapine 2nd line treatment when other agents are ineffective or not tolerated Antipsychotics in schizophrenia Depot antipsychotic preparations Useful for noncompliant patients with poor insight Antidepressents and mood stabilisers In schizoaffective disorders Patients with secondary mood symptoms or aggressivity Differentiate between adverse effects and signs of disease progression E.g. Parkinsonism vs. psychotic hysteria, Akathisia vs. exacerbation of psychosis Antipsychotics in schizophrenia Oral administration Divided daily doses at initial phase Once daily at bedtime when stabilized Promoting sleep and reducing daytime sedation Smallest effective dose employed Oral-dispersible and solution preparations For unreliable patients Injections Usually deltoid or gluteal muscle (or according to manufacturer) Depot injections At intervals of 1 to 4 weeks Generally not more than 2-3ml oily injection at one site Correct injection technique (z-track) and injection site rotation Antipsychotics in schizophrenia Treatment response First 7 days Decreased agitation, hostility, combativeness, anxiety, tension and aggression Normalization of sleep and eating habits First 2-3 weeks Increased socialization, improvement in self-care 6-8 weeks Improvement in formal thought disorder Antipsychotics in schizophrenia Acute phase Initiate therapy Titrate as tolerated to average effective dose Stabilization phase Dose titration within the therapeutic range Maintenance phase Therapy should be continued for at least 12 months after remission of 1st episode Good treatment responders should be treated for at least 5 years Continuous lifetime maintenance required in the majority of patients to prevent relapse Lowest effective and tolerable dose Depression and antidepressants Depression Depressed mood and/or decrease in interest in things that used to give pleasure Sadness severe enough or persistent enough to interfere with function DSM-IV: Major depressive disorder / major depression Dysthymia Depression for most of the day, more days than not Depressive disorder not otherwise specified Depressive disorder due to a general physical condition Substance-induced depressive disorder Depression Epidemiology Life prevalence 3-17% Onset in late 20s Highest in 25-44 years Elderly in community Female vs male = 2:1 Female 10-25% lifetime risk Male 5-12% lifetime risk Depression Epidemiology 4th most common reason to visit family physician Most common in elderly and difficult to diagnose Coexists with dementia or delirium frequently Recurrence rate of major depression After single episode = 50% After second episode = 70% After third episode = 90% Approx 10-15% of patients with major depressive or bipolar disorder complete suicide Depression Signs and symptoms Depressed mood Sleep (insomnia or hypersomnia) Loss of interest (including libido) Guilt Energy loss Concentration loss Appetite (loss or gain) Psychomotor (agitation or retardation) Suicide (ideation) Depression Etiology Etiology unknown Uncertain with heredity History of child abuse or other major life stresses Changes in neurotransmitter/neurohormone levels Cholinergic, noradrenergic/dopaminergic and serotonergic neurotransmission Deregulation with hypothalamic-pituitary-adrenal axis, hypothalamic-pituitary-thyroid axis and growth hormone Life stresses (e.g. Separation and losses) Depression Pathophysiology Exact course unknown Changes in receptor-neurotransmitter relationship in limbic system Serotonin, norepinephrine, sometimes dopamine Increased pump uptake of neurotransmitter Reabsorption into neuron Destroyed by monoamine oxidase in mitochondria Lack of neurotransmitters Antidepressants Tricyclic and related antidepressants (TCA) E.g. amitriptyline, imipramine, doxepin, mianserin, trazodone Monoamine-oxidase inhibitors (MAOI) E.g. moclobemide, phenelzine, isocarboxazid, tranylcypromine Selective serotonin reuptake inhibitors (SSRI) E.g. fluoxetine, paroxetine, sertraline, citalopram Other antidepressants E.g. mirtazapine, venlafaxine, duloxetine, flupentixol Tricyclic and related antidepressants (TCA) Amitriptyline (Saroten®) Clomipramine (Anafranil®) Dothiepin (a.k.a. dosulepin, Prothiaden®) Doxepin (Sinequan®) Imipramine (Tofranil®) Mianserin (Tolvon®) Nortriptyline (Nortrilen®) Trazodone (Trittico®) Trimipramine (Surmontil®) Tricyclic and related antidepressants (TCA) Mechanism of action Blocks neuronal uptake or norepinephrine and serotonin Initial response develops in 1-3 weeks Maximal response develops in 1-2 months Older tricyclics Marked anticholinergic Adverse effects Risk of cardiotoxicity Tricyclic-related drugs (e.g. trazodone) Fewer anticholinergic Adverse effects Sedation, dizziness, priapism (persistent penile erection accompanied by pain and tenderness) Tricyclic and related antidepressants (TCA) Properties Inexpensive, generic Some with off-label use, e.g. Neuropathy with amitriptyline Refractory skin diseases with doxepin Very dangerous in overdose Life threatening Lethal dose only 8 times average daily dose Acutely depressed patients should not be given more than 1-week TCA supply at one time Tricyclic and related antidepressants (TCA) Adverse effects Orthostatic hypotension Reduced by moving slowly when assuming upright posture Sit or lie down if symptoms (dizziness, lightheadedness) occur Divided doses and slow titration Anticholinergic effects Dry mouth, blurred vision, photophobia, constipation, urinary retention, tachycardia Tolerance may develop as treatment persists Divided doses and slow titration Sedation Dose at bedtime Tricyclic and related antidepressants (TCA) Adverse effects Cardiac toxicity Arrhythmias and heart block ECG recommended before initiation Do not use in heart block Seizures Lowered seizure threshold Hypomania (mild mania) Elevated mood Patient should be evaluated to determine dose reduction or bipolar disorder Diaphoresis Paradoxical effect Tricyclic and related antidepressants (TCA) Drug interactions CNS depressants Narcotics, benzodiazepines Additive CNS depression Anticholinergics Additive anticholinergic effects P450 enzyme inducers/inhibitors Monoamine-oxidase inhibitors (MAOI) Moclobemide (Aurorix®) Not registered in Hong Kong Phenelzine Isocarboxazid Tranylcypromine Monoamine-oxidase inhibitors (MAOI) Mechanism of action Inhibit both MAO-A and MAO-B Phenelzine, tranylcypromine Selective & reversible inhibitor of MAO-A Moclobemide Monoamine-oxidase inhibitors (MAOI) Properties Useful in atypical depression (somnolence and weight gain), refractory disorders and certain types of anxiety disorders Less prescribed than tricyclics, SSRIs and other antidepressants Danger of dietary and drug interactions Monoamine-oxidase inhibitors (MAOI) Properties Drug interactions Other antidepressants should not be started for 2 weeks after MAOI has been stopped (3 weeks for clomipramine or imipramine) MAOI should not be started for 7-14 days after a tricyclic or related antidepressant (3 weeks for clomipramine or imipramine) MAOI should not be started for at least 2 weeks after a previous MAOI Monoamine-oxidase inhibitors (MAOI) Adverse effects Hypertensive crisis Severe occipital headache, photophobia, palpitation, sharply increased in BP due to additive effect between MAOI and adrenergic stimulants Tyramine-rich food e.g. cheese, wine, smoked/aged/picked meat or fish, alcohol Amphetamins Pseudoephedrine Monoamine-oxidase inhibitors (MAOI) Adverse effects Orthostatic hypotension Insomnia Weight gain Sexual dysfunction Selective serotonin reuptake inhibitors (SSRI) Fluoxetine (Prozac®) Fluvoxamine (Faverin®) Paroxetine (Seroxat®) Sertraline (Zoloft®) Citalopram (Cipram®) Escitalopram (Lexapro®) Selective serotonin reuptake inhibitors (SSRI) Mechanism of action Inhibits reuptake of serotonin (5-HT) presynaptic uptake Increases availability of serotonin at synapses Selective serotonin reuptake inhibitors (SSRI) Properties Overdose less likely to be fatal Less anticholinergic side effects But more GI side effects Seems to be better tolerated Selective serotonin reuptake inhibitors (SSRI) Properties Fluoxetine Most stimulating SSRI Indicated for premenstrual dysphoric disorder (PMDD) (as Sarafem®) Long half-life, ensure 5 week washout before MAOI (2 week for other SSRI) Some SSRIs also indicated for Obsessive-compulsive disorder (OCD) Panic disorder Eating disorders Social phobia Post traumatic stress disorder (PTSD) Selective serotonin reuptake inhibitors (SSRI) Adverse effects Headache GI Nausea, diarrhoea, loss of appetite Titrate dose to minimize side effect May be taken with food Anticholinergic Adverse effects Fever than TCA Tend to see more with paroxetine Selective serotonin reuptake inhibitors (SSRI) Adverse effects Somnolence or insomnia Dose in morning for insomnia Increase in anxiety, agitation, akathisia early in treatment (esp. fluoxetine) Agitation or nervousness Sexual dysfunction Selective serotonin reuptake inhibitors (SSRI) Adverse effects Serotonergic syndrome Rare but potentially fatal interaction between 2 or more drugs that enhance serotonin Anxiety, shivering, diaphoresis, tremor, hyperflexia, autonomic instability (BP, pulse) Fatal if malignant hyperthermia Management Mild: resolve in 24-48 hours after discontinuing offending agent Severe: 5-HT antagonist, cyproheptidine, propranolol, methysergide, dantrolene (hyperthermia) Serotonin norepinephrine reuptake inhibitor (SNRI) Duloxetine (Cymbalta®) Venlafaxine (Efexor®, Efexor XR®) Mechanism of action Inhibits norepinephrine and serotonin reuptake Potentiates neurotransmitter activity in the CNS Serotonin norepinephrine reuptake inhibitor (SNRI) Duloxetine (Cymbalta®) Properties and Adverse effects More potent than venlafaxine Also indicated for diabetic neuropathy Insomnia, nausea, headache Serotonin norepinephrine reuptake inhibitor (SNRI) Venlafaxine (Efexor®, Efexor XR®) Properties and Adverse effects Also for anxiety disorders Lacks sedative and anticholinergic effects predominant with TCAs Nausea, dizziness, sexual dysfunction, hypertension (when > 300mg/day) Mixed serotonin norepinephrine effects Mirtazapine (Mirtazon®, Remeron®, Remeron SolTab®) Mechanism of action Presynaptic α2-antagonist Increases central noradrenergic and serotonergic neurotransmission Mixed serotonin norepinephrine effects Mirtazapine (Mirtazon®, Remeron®, Remeron SolTab®) Properties and Adverse effects Fewer anticholinergic effects Marked sedation during initial treatment Stimulating as dose increases Increased appetite and weight gain Constipation, dry mouth Norepinephrine dopamine reuptake inhibitor (NDRI) Bupropion (Wellbutrin SR®) Mechanism of action Inhibits weakly the neuronal uptake of dopamine, norepinephrine and serotonin Does not inhibit monoamine oxidase Norepinephrine dopamine reuptake inhibitor (NDRI) Bupropion (Wellbutrin SR®) Properties and side effects GI side effects, confusion, dizziness, headache, insomnia, tremor Seizure risk at high doses Minimal risk of sexual dysfunction Also licensed for smoking cessation (Zyban®) Other antidepressants Flupenthixol (Fluanxol®) Typical antipsychotic Antidepressant effect at low doses Antipsychotic dose: 3-9mg twice daily Antidepressant dose: 1-3mg daily Combined with another antidepressant as Deanxit® Flupenthixol 0.5mg + melitracen 10mg For depression and anxiety Non-antidepressants Anxiolytics Antipsychotics Use may mask the true diagnosis Used with caution But are still useful adjuncts in agitated patients Lithium and thyroid To potentiate effect of antidepressants in refractory cases Lithium: plasma level 0.4-0.8mEq/L Thyroid supplement: 25mcg/day Antidepressants in depression Choice of agents All are equally efficacious for depression Selection based on Side effect profile Potential drug interaction Response failure to an antidepressant does not predict response to another drug class or another drug within class Antidepressants in depression Geriatrics Reduce initial dose by half Gradual dose titration Risk of dizziness and syncope Hyponatremia Pediatrics Decrease initial dose by half Recent evidence links SSRIs with suicide in adolescents Antidepressants in depression Treatment response Weeks 1-2 Physical responses Improvement in appetite and sleep Weeks 3-4 Energy and cognitive responses Improvement in energy Improvement in guilt, concentration Weeks 5-6 Emotional responses Improvement in mood Antidepressants in depression Continuation therapy To prevent relapse 4-9 months after complete remission of symptoms At therapeutic doses Lifelong maintenance therapy Recommended by some investigators for patients at greater risk or reoccurrence < 40 years with ≥ 2 prior episodes Any age with ≥ 3 prior episodes Bipolar disorders and mood stabilizers Bipolar disorders Cyclic disorder with recurrent fluctuations in mood, energy and behaviour, “mood swings” Episodes of mania and/or hypomania, and major depression that cause marked impairment and/or hospitalization Devastating long term illness Deterioration in functioning Suicidal ideation Substance abuse Noncompliance to meds Bipolar disorders DSM-IV: Bipolar I disorder ≥1 manic or mixed episode Bipolar II disorder Recurrent major depressive episodes with hypomanic episodes Bipolar disorder not otherwise specified Cyclothymic disorder Both hypomanic and depressive episodes not meeting criteria for a major depressive epidose Mood symptoms have persisted for 2 years without > 2 months of remission at a time Bipolar disorder due to their general physical condition Substance-induced bipolar disorder Bipolar disorders Epidemiology Prevelance 1-2% Male = female Average age of onset 20 to 30 10-15% rate of suicide Bipolar disorders Epidemiology 5-15% of adults diagnosed with major depressive disorder eventually meet criteria for bipolar I disorders 60-70% of manic or hypomanic episodes occur immediately before or after major depressive episode Period of euthymia (normal mood) Bipolar disorders Etiology Exact cause unknown Genetic predisposition Life stressors Can occur with several physical disorders As adverse effects of many drugs As part of several mental disorders Bipolar disorders Pathophysiology Neurotransmitters known to be involved Serotonin Norepinephrine Dopamine Brain structures most involved MRI findings suggests abnormalities in prefrontal cortical areas, striatum, and amygdala predate illness onset Bipolar disorders Signs and symptoms Mania Distractability Insomnia Grandiosity or inflated selfesteem Flight of ideas or subjective experience that thoughts are racing Agitation or increase in goal-directed activity Speech pressured/more talkative than usual Taking risks Hypomania Distinct period of persistently elevated, expansive, or irritable mood Lasting throughout at least 4 days < 1 week for mania Different from usual nondepressed mood But not severe enough to cause marked impairment in social or occupational functioning Bipolar disorders Signs and symptoms Mixed episode Simultaneous occurrence of manic and depressive symptoms nearly every day for aat least 1 week Poorer prognosis More seen in younger and older patients Less likely to respond to mood stabilizer monotherapy Rapid cyclers > 4 major depressive or manic episodes (manic, mixed or hypomanic for 12 months) Frequent and severe episodes of depression Poorer prognosis Often require combination therapies Mood stabilizers Lithium Anticonvulsants Valproate Carbamazepine Lamotrigine Antipsychotics, antidepressants and others Lithium Mechanism of action Not fully understood Mood-stabilizing effect has been postulated to reduction of catecholamine neurotransmitter concentration Possibly related to Na-K-ATPase to improve membrane transport of Na ion Alternative postulate that Li may decrease cyclic AMP concentrations, which would decrease sensitivity of hormonal-sensitive adenylcyclase receptors Lithium Properties Manic episode Approved for manic episodes and maintenance therapy About 70% patients show at least partial reduction of mania Full effect takes 1-2 weeks Depressive episode As adjunct to antidepressant for refractory patients Onset 4-6 weeks Long term use reduces suicide risk and mortality Narrow therapeutic index Lithium Dosing Start with low divided doses to minimize Adverse effects Gradual titration Adjusted to achieve serum lithium Acute manic episode: 1.0-1.5 mmol/L Maintenance: 0.6-1.2 mmol/L Lithium Adverse effects Early, dose related Adverse effects GI distress Sedation, weight gain Muscle weakness Polyuria, polydipsia Impaired cognitive funciton Tremor Tolerance may develop Management Take with meal Beta blocker for tremor Late Adverse effects Psoriasis / acne exacerbation Nephrogenic diabetes insipidus Hypothyroidism Cardiac T-wave flattening or inversion Bradycardia AV block Leukocytosis Lithium Adverse effects Nephrogenic diabetes insipidus (DI) Reduced renal response to aldosterone (ADH) Low osmolality polyuria > 3L urine output per day Urine specific gravity < 1.005 Management Lowest effective dose Adequate hydration Once-daily bedtime dose Thiazides (lithium dose to 50%) or amiloride Lithium Lithium toxicity (serum level > 1.5-2.5 mmol/L) Mild toxicity Moderate toxicity Severe toxicity (< 1.6 mmol/L) (< 2.5 mmol/L) (> 2.5 mmol/L) Apathy Blurred vision Cardiovascular collapse Irritability Confusion Coma Lethargy Drowsiness Seizure Muscle weakness Progressing tremor Nausea Slurred speech Unsteady gait Lithium Toxicity Discontinue lithium NaCl infusion, rehydration, electrolyte Monitor lithium level q3h Electrolyte panel, renal function labs Hemodialysis if patient not clearing lithium well or lithium level > 3 mmol/L Supportive care Lithium Interactions Numerous drug interactions! Dietary sodium, soda, coffee, tea, caffeine lithium clearance Acute mania lithium clearance Lithium Formulation Regular release tablets As lithium carbonate 250mg and 400mg (e.g. Camcolit®) More adverse effects due to higher peak levels More convenient for small dose increments Sustained release tablets As lithium sulphate 660mg (e.g. Lithiofor®) Fewer Adverse effects More expensive Anticonvulsants Carbamazepine (Tegretol®, Tegretol CR®) Lamotrigine (Lamictal®) Valproate (Epilim EC®, Epilim Chrono®) Carbamazepine Properties Approved for acute mania and mixed episodes in bipolar I disorder As Equetro® extended-release capsules Preferred when response to lithium is poor Rapid cyclers Mixed mania episodes Not recommended as monotherapy for bipolar depression P450 enzyme inducer Carbamazepine Adverse effects Weight gain Neurotoxicity Diplopia, drowsiness, blurred vision, vertigo Transient and reversible with dose reduction Mild elevation of liver enzymes Hypersensitivity rash Uncommon Carbamazepine Adverse effects Hematologic effects Rare: agranulocytosis, blood dyscrasia Discontinue when Fever, sore throat, rash, mouth ulcers, bruising or bleeding Syndrome of inappropriate antidiuretic hormine (SIADH) Cardiac conduction abnormalities (sometimes arrhythmia) Lamotrigine Properties Approved for maintenance of bipolar I disorder To delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) Significant antidepressant effect without increase in cycling May not be effective for severe mania Significant drug interactions with other anticonvulsants Lamotrigine Dosing of lamotrigine in bipolar disorders Weeks 1-2 Weeks 3-4 Week 5 Maintenance dose Lamotrigine monotherapy 25mg qd 50mg qd 100mg qd 200mg/day Lamotrigine added to valproate 25mg qod 25mg qd 50mg qd 100mg/day Lamotrigine added to enzyme inducers w/o valproate 50mg qd 100mg/day in divided doses 200mg/day for Increase up 1 week, then to 300mg/day for 400mg/day 1 week (both in divided doses ) Lamotrigine Adverse effects Skin rash Stevens-Johnson’s Syndrome, toxic epidermal necrosis, hypersensitivity syndrome Consider withdrawal if rash or signs of hypersensitivity occur Increased risk of serious skin reactions with Concomitant use of valproate Initial lamotrigine doses higher than recommended dose Dose escalation more rapid than recommended Lamotrigine Adverse effects GI Abdominal pain, indigestion, nausea, vomiting Asthenia, pain Ataxia, dizziness, headache, somnolence Valproate Properties Approved for treatment of mania in bipolar disorder As divalproex sodium (Depakote® and Depakote® ER) Delayed release (Depakote®): manic episode Extended release (Depakote® ER): acute mania and mixed episodes Preferred when response to lithium is poor Substance abusers Rapid cyclers Mixed mania episodes P450 enzyme inhibitor Valproate Adverse effects GI: anorexia, indigestion, nausea, vomiting, heartburn, diarrhoea Decrease dose, antacid or H2-antagonist Irreversible but rare hepatotoxicyt Weight gain, increased appetite Decrease dose, monitor weight Valproate Adverse effects Neutropenia and thrombocytopenia Sedation, tremor Decrease dose Beta blocker for tremor Menstrual disturbances and polycystic ovaries is posssible Transient alopecia Other anticonvulsants Oxcarbazepine (Trileptal®) Topiramate (Topamax®) No FDA approval Tested in some clinical studies Less used than carbamazepine, lamotrigine and valproate Other drugs for bipolar diseases Antipsychotics Effective as adjunctive treatment of acute mania Should be used when patient is psychotic Novel ones preferred Monotherapy may be used in acute nonpsychotic mania, but effectiveness of mood stabilization in maintenance phase not well established Other drugs for bipolar diseases Antipsychotics Olanzapine Risperidone FDA approval: acute mania, mixed episodes, maintenance Aripiprazole Ziprasidone FDA approval: acute mania, mixed episodes Quetiapine FDA approval: acute mania, depressed phase Other drugs for bipolar diseases Antidepressants May improve acute depression in short term Ineffective for long term Monotherapy (TCAs in particular) can precipitate manic episodes or rapid cycling May be used as adjunct with mood stabilizers if patient has a history of refractory depression and manic episodes that are relatively responsive Other drugs for bipolar diseases Benzodiazepines As adjunct to treat acute agitation, anxiety and insomnia For severely ill patients Short term use only Mood stabilizers in bipolar disorders Acute manic or mixed episode Mild to moderate 1) Stabilize with lithium / valproate / antipsycotic (e.g. olanzapine, quetiapine, risperidone) Alternative anticonvulsant: carbamazepine, lamotrigine or oxcabazepine 2) If inadequate response, adjunctive benzodiazepines for anxiety or insomnia 3) If still inadequate response, consider two-drug therapy Lithium + anticonvulsant / antipsychotic Anticonvulsant + anticonvulsant / antipsychotic Mood stabilizers in bipolar disorders Acute manic or mixed episode Moderate to severe 1) Stabilize with lithium / valproate PLUS antipsychotic for short term adjunctive treatment (e.g. olanzapine, quetiapine, risperidone) Alternative anticonvulsant: carbamazepine, lamotrigine or oxcabazepine 2) If inadequate response, adjunctive benzodiazepines for anxiety or insomnia Lorazepam recommended for catatonia Mood stabilizers in bipolar disorders Acute manic or mixed episode Moderate to severe 3) If still inadequate response, consider 2-drug therapy Lithium + anticonvulsant / antipsychotic Anticonvulsant + anticonvulsant / antipsychotic 4) If still inadequate response, electroconvulsive therapy or add clozapine for refractory illness 5) If still inadequate response, consider adjunctive therapies α2-adrenergic agonist, calcium channel blockers (nimodipine, verapamil), newer anticonvulsants (e.g. gabapentin, topiramate) Mood stabilizers in bipolar disorders Depressive episode Mild to moderate Stabilize with lithium or lamotrigine Alternative anticonvulsant: carbamazepine, oxcabazepine or valproate Mood stabilizers in bipolar disorders Depressive episode Moderate to severe 1) Stabilize with 2-drug therapy Lithium / lamotrigine PLUS antidepressant Lithium PLUS lamotrigine Alternative anticonvulsant: carbamazepine, oxcabazepine or valproate 2) If inadequate response, short-term adjunctive atypical antipsychotic if needed Mood stabilizers in bipolar disorders Depressive episode Moderate to severe 3) If still inadequate response, consider 3-drug therapy Lithium + anticonvulsant + antipsychotic Lamotrigine + anticonvulsant + antidepressant 4) If still inadequate response, electroconvulsive therapy (ECT) for refractory illness and depression with psychosis or catatonia 5) If still inadequate response, consider adjunctive therapies α2-adrenergic agonist, calcium channel blockers (nimodipine, verapamil), newer anticonvulsants (e.g. gabapentin, topiramate) Mood stabilizers in bipolar disorders Initial therapy If first line agent(s) not effective for 2-4 weeks, add a second agent to augment mood stabilization Maintenance therapy Maintain with a mood stabilizer for both bipolar I and II disorders for 6-month continuation phase First line: lithium or valproate Alternative: carbamazepine, lamotrigine, oxcabazepine Taper off adjunctive therapy and discontinue Patient with only 1 manic episode should continue maintenance therapy for 12 months Gradually taper off over several months (usually 6 months after complete remission) Mood stabilizers in bipolar disorders Lifelong prophylaxis Consider with mood stabilizers for Patients after 2 manic episodes After 1 severe episode Strong family history of bipolar disorder Frequent episodes (> 1 per year) Rapid onset of manic apisodes Bipolar II After 3 hypomanic episodes Patients who become hypomanic with antidepressants End Questions & Answers