Morning Report
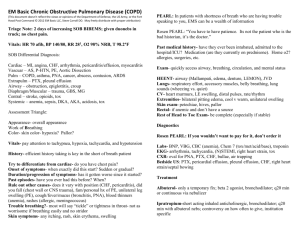
advertisement

Good Morning Morning Report July 23, 2013 Semantic Qualifiers Symptoms Acute /subacute Chronic Localized Diffuse Single Multiple Static Progressive Constant Intermittent Single Episode Problem Characteristics Ill-appearing/ Toxic Well-appearing/ Non-toxic Recurrent Localized problem Systemic problem Abrupt Gradual Acquired Congenital Severe Mild New problem Recurrence of old problem Painful Nonpainful Bilious Nonbilious Sharp/Stabbing Dull/Vague Illness Script Predisposing Conditions Age, gender, preceding events (trauma, viral illness, etc), medication use, past medical history (diagnoses, surgeries, etc) Pathophysiological Insult What is physically happening in the body, organisms involved, etc. Clinical Manifestations Signs and symptoms Labs and imaging Predisposing Conditions Incidence: 35-40/1000 in <5yo, 7/1000 in older children and adolescents Boys > girls List 2 environmental risk factors for PNA Lower socioeconomic status Smoke exposure-cigarette smoke or wood smoke Cold weather Alcohol Question B….aspiration Predisposing Conditions Name 4 medical conditions that increase PNA risk Medical history Sickle cell BPD GERD Cystic Fibrosis Heart disease Immunodeficiency Increased aspiration Neuromuscular disorder Seizure disorder Question E. Viral agents are the most common cause of PNA in infants and young children Pathophysiology What method of transmission is reponsible for the spread of PNA? Spread by droplets Typically follows URI Mechanism Colonization of nasopharynx with further inhalation of microorganisms, leading to a pulmonary focus of infection Less commonly…bacteremia results from the initial upper airway colonization with subsequent seeding of lungs Pathophysiology What is the most common organism causing bacterial PNA? Streptococcus pneumonia What are 3 additional pathogens that cause bacterial PNA? S. aureus, Group A Strep, GNR (<3mo), anaerobes 6 week old, afebrile infant with tachypnea, cough, and CXR showing interstitial changes? Chlamydia pneumoniae What are 2 viral causes of PNA? RSV, Parainfluenza, Influenza, Metapneumovirus, etc. Pathophysiology Question C. Mycoplasma pneumoniae Microbiology of PNA changes based on the age of the patient, and this should be kept in mind when making management decisions! Clinical Manifestations Bacterial PNA Abrupt onset High fever Cough Sometimes productive Focal findings on lung exam Crackles Diminished breath sounds Bronchial breath sounds Egophany Toxic appearance Respiratory distress Tachypnea (most sensitive/specific) Retractions Nasal Flaring Grunting Hypoxia Chest pain Emesis and abdominal pain Clinical Manifestations Atypical PNA School age or older Constitutional symptoms Fever Malaise Myalgias Headache Gradual development of dry cough later in the illness as other symptoms improve Clinical Manifestations Bacterial Atypical Tuberculosis Clinical Manifestations Question C. Development of an empyema Name 3 possible complications of pneumonia Lung abscess Pleural effusion Empyema Necrotizing pneumonia Pneumothorax Sepsis Bronchopulmonary fistula Pneumatoceles Complications Lung abscess Often develop following aspiration Thick-walled cavity with air/fluid level TB should be considered Needle aspiration for culture Necrotizing pneumonia Rare complication of bact PNA Liquefaction/necrosis caused by toxins of virulent organisms VERY ill IV abx for at least 4 weeks Complications Sterile para-pneumonic effusion Purulent effusions with resultant empyema Persistent fever, ill-appearing, tachypnea, increased WOB, chest pain and splinting Dullness to percussion/decreased air entry CXR with decubitus, US, CT Treatment Question C. Outpatient treatment with high dose Amoxicillin Outpatient therapy (7-10days total) First line: High dose Amoxicillin at 80-100mg/kg/day Penicillin allergy? Cephalosporin (non-type 1) Clindamycin/Azithromycin (type 1 allergy) Atypical organisms: Azithromycin x 5 days Aspiration PNA: Augmentin or Clindamycin Inpatient therapy (duration varies) Ceftriaxone or Ampicillin More extensive disease/failed treatment Vancomycin, Clindamycin Azithromycin (adjunctive coverage sometime given) Treatment Admission Criteria for admission <3 months Respiratory distress Hypoxemia Dehydrated Highly febrile/toxic Underlying disease Testing (once admitted) CBC Blood culture CXR +/- Sputum culture Treatment Tests to consider for patient who is not improving clinically? Bronchoscopy, lung aspiration, open lung biopsy MORE CONTENT SPECS Recurrent PNA: >1 episode/year, >3 episodes in lifetime Anatomic lesions: vascular rings, cysts, pulmonary sequestration Respiratory tract disorders: CF, GERD, aspiration Immunodeficiency: HIV, CGD, hypogammaglobulinemia **REFER if documented Congenital lesions of the lung (CCAM, sequestration, etc) can mimic PNA Prevention of PNA Good handwashing, personal respiratory hygeine, proper immunization, breastfeeding, limiting sick contacts, decrease smoke exposure Thanks!! Almost every content spec “Pneumonia.” Pediatrics in Review. 2008, volume 29, p147 Class Housestaff Today! 1st years – Board Room B 2nd years – Board Room A 3rd years – 2 center Bon Voyage Rocky! He’s headed to Indonesia on a medical service trip!!!