My belly hurts.
advertisement

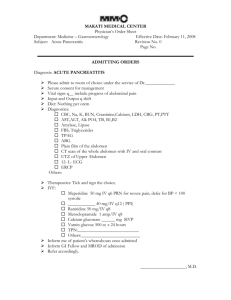
CC: ABDOMINAL PAIN HPI 42 year old male presents to the Emergency Department with severe epigastric pain that started 3 days ago. He describes the pain as constant and epigastric. It has been severe since its onset, and also is described as band-like and radiating to his back. He also complains of nausea and vomiting that started yesterday. His wife is present and reports increased agitation since he quit drinking alcohol after one last binge 1 week ago. She also reports that he has a hx of gall stones and was recently stung by a scorpion during a trip to Arizona. Denies fever, rash or headache. Denies diarrhea or constipation. No hx of GI bleeding. HPI Past Medical Hx: Family and Social Hx: Mother with hx Hx alcohol dependence Hx of choledocholithiasis tx with ERCP Hx of scorpion sting 1 week ago Hx of migraine headaches No other past surgical hx cholecystitis, hx of HTN and CAD. Father has hx of obesity and alcohol dependence. 2 Brothers who are healthy Married, lives at home with wife, two children and dog. Recent travel to Arizona for a hiking trip. Works in a beer bottling factory as a quality assurance engineer. DIFFERENTIAL DIAGNOSIS Acute cholecystitis or cholangitis Penetrating duodenal ulcer Pancreatic pseudocyst Ischemic colitis Small bowel obstruction Abdominal aortic aneurysm Kidney stone Nonpancreatic causes of increased amylase PHYSICAL EXAM VITALS: BP 115/80, T 38.0, R 16, HR 95 GEN: Appears to be in moderate distress secondary to pain. HEENT: Normocephalic, atraumatic (NCAT), pupils equal, round and reactive (PERRL) and extraocular movements intact (EOMI). Moist mucous membranes. Oropharynx clear and patent, no erythema. CV, RESP: Regular rate and rhythm, no murmurs, rubs or gallops. Breath sounds are clear to auscultation bilaterally (CTAB), no crackles or ronchi, and symmetrical chest rise, though breathing is noticeably shallow. ABDOMINAL: Soft, mildly distended abdomen, voluntary guarding no rebound tenderness. Abdominal tenderness on exam is out of proportion to the patient’s level of discomfort. Negative Murphy’s sign. RECTAL: DRE is negative for gross and occult blood. Perianal area is intact without lesions. NEURO: Alert, awake and oriented to person, place and time. (AAOx3). CN II-VII intact. Strength 5/5 and sensation intact over all extremities. Classic and Other Concerning Symptoms •Grey-Turner’s Sign: ecchymotic discoloration in the flank. •Cullen’s Sign: ecchymotic discoloration in the periumbilical region. •These signs occur in 1% of cases and reflect intraabdominal hemorrhage and are associated with poor prognosis. •Jaundice is seen in cases of pancreatitis where inflammation is secondary to choledocholithiasis or edema at the head of the pancreas from obstruction of the common bile duct. •Epigastric mass may be palpable due to pseudocyst formation. •Subcutaneous nodular fat necrosis, thrombophlebitis in the legs and polyarthritis are also less commonly seen. LABORATORY TESTS CBC: normal WBC: 16,000 CMP: normal, Calcium 2, AST 220, ALT 80, Alk phos 150, Albumin 25, tBili 6, Amylase 320 UA: Negative for WBC, RBC, protein, leukocyte esterase and nitrites. What would you like to do next? Acute Abdominal Series Abdominal Plain Film : helps to exclude other causes of abdominal pain, including bowel obstruction or bowel perforation. Localized ileus of a segment of the small intestine, aka “sentinal loop” may be seen. Generalized ileus can occur in severe disease. Ground glass appearance may indicate ascites. Chest Film: May see elevation of hemidiaphragm, pleural effusion or basal atelectasis, left sided or bilateral. LOCALIZED ILEUS WITH SENTINAL LOOP SIGN Abdominal CT Scan Most important imaging study for diagnosis of acute pancreatitis, intraabdominal complications and to assess severity. The severity of acute pancreatitis based on non-contrast CT findings: Grade A – Normal pancreas consistent with mild pancreatitis Grade B – Focal or diffuse enlargement of the gland, including contour irregularities and inhomogeneous attenuation but without peripancreatic inflammation Grade C – Abnormalities seen in grade B plus peripancreatic inflammation Grade D – Grade C plus single fluid collection Grade E – Grade C plus two or more peripancreatic fluid collections or gas in the pancreas or retroperitoneum Non-Contrast CT with peripancreatic fat stranding. Pancreatitis Although measurement of amylase and lipase are useful for diagnosis of pancreatitis, serial measurements are not useful to predict prognosis or to guide management. Important radiologic features may be seen on a plain film of the abdomen, chest radiograph, and spiral (helical) CT scan. CT scan is the most important imaging test for the diagnosis of acute pancreatitis and its intraabdominal complications and also for assessment of severity. And CT is best utilized in patients who do not improve with conservative management or in whom you suspect complications. Histological Interpretations Acute pancreatitis morphology ranges from mild inflammation and edema to severe extensive necrosis and hemorrhage. Findings include: 1. Microvascular leakage causing edema 2. Necrosis of fat by lipolytic enzymes 3. Acute inflammation 4. Proteolytic destruction of pancreatic parenchyma 5. Destruction of blood vessels and subsequent interstitial hemorrhage Histological Features Cont’d Below see regions of fat necrosis and focal pancreatic parenchymal necrosis. Gross specimens reveal dark areas of hemorrhage in the head of the pancreas and focal areas of pale fat necrosis Treatment Acute pancreatitis can be divided into two broad categories: edematous, interstitial or mild acute pancreatitis and necrotizing or severe acute pancreatitisTreatment varies depending on the severity of the condition. Mild pancreatitis is treated for several days with supportive care including pain control, intravenous fluids, correction of electrolyte and metabolic abnormalities, and nothing by mouth. In severe pancreatitis, intensive care unit monitoring and support of pulmonary, renal, circulatory, and hepatobiliary function may minimize systemic sequelae. In patients with gallstone pancreatitis, we recommend early ERCP and sphincterotomy for those who have a high suspicion of cholestasis and those with cholangitis. Cholecystectomy should be performed after recovery in all patients with gallstone pancreatitis. The anatomic changes of acute pancreatitis strongly suggest autodigestion of the pancreatic substance by inappropriately activated pancreatic enzymes. Summary References: Kumar, Vinay, Abul K. Abbas, Nelson Fausto, Stanley L. Robbins, and Ramzi S. Cotran. "Chapter 19 The Pancreas." Robbins and Cotran Pathologic Basis of Disease. Philadelphia: Elsevier Saunders, 2005. 893-897. Print. Vege, Santhi S., MD. "Clinical Manifestations and Diagnosis of Acute Pancreatitis." Clinical Manifestations and Diagnosis of Acute Pancreatitis. N.p., 13 Nov. 2012. Web. 20 Dec. 2012. <http://www.uptodate.com.proxy.medlib.iupui.edu/contents/clinic al-manifestations-and-diagnosis-of-acute-pancreatitis?source= search_result&search=pancreatitis&selectedTitle=1~150>. Vege, Santhi S., MD. "Treatment of Acute Pancreatitis." Treatment of Acute Pancreatitis. N.p., 25 Oct. 2012. Web. 20 Dec. 2012. <http://www.uptodate.com.proxy.medlib.iupui.edu/contents/treat ment-of-acute-pancreatitis?source=search_result&search= pancreatitis&selectedTitle=2~150>.