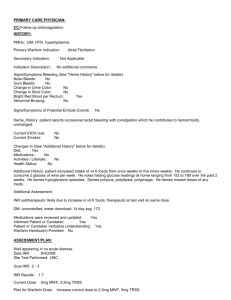
Vitamin K 1
advertisement

WARFARIN THERAPY Nicolas Novitzky The Ideal Oral Anticoagulant Ideally, an oral anticoagulant would: Have high efficacy in reducing thromboembolic events Reach therapeutic levels within several hours Oral and/or IV administration Ability to inhibit free and clot bound thrombin Require no remote monitoring Have little interaction with food or other drugs Offer a good safety profile with regard to bleeding risk Availability of an antidote Antithrombotic Agents: Mechanism of Action Anticoagulants: prevent clot formation and extension Heparins, LNWH, huridin Warfarin Direct anti thrombin inhibitors Dabigatran Direct factor Xa inhibitors Rivaroxaban, apixaban Antiplatelet drugs: interfere with platelet activity Thrombolytic agents: dissolve existing thrombi Coagulation Cascade Warfarin typically works on several calcium-dependent clotting factors, including factors II, VII, IX (not shown), and X. Vitamin K-Dependent Clotting Factors Warfarin: Indications Prophylaxis and /or treatment of: Venous thrombosis and its extension Pulmonary embolism Thromboembolic complications associated with AF and cardiac valve replacement Prophylaxis of recurrent thrombosis in APS Post MI, to reduce the risk of death, recurrent MI, stroke Systemic embolization Prophylaxis of genetic thrombophilia Relative Contraindications to Warfarin Therapy Pregnancy Situations where the risk of hemorrhage is greater than the potential clinical benefits of therapy Uncontrolled alcohol/drug abuse Unsupervised dementia/psychosis The Dilemma of Anticoagulation Management Narrow therapeutic window of effectiveness & safety. Frequent monitoring is required to maintain patients in the therapeutic window. Many factors influence a patient’s stability within that window. Monitoring is labour intensive and complex • • Consequences Increased adverse events with poor management Physicians avoid warfarin use because of its complexity Successful Anticoagulation Team work in monitoring anticoagulation Correct indication Patient education Compliance Understanding coagulation results Diet Drug interactions Toxicity, bleeding Laboratory testing Point of care testing Doctor’s office Patient self testing Disadvantages of Warfarin Narrow therapeutic index Need for frequent monitoring Slow onset & offset of action Large inter-individual dosing differences Drug-Drug and drug-food interactions Genetic polymorphisms Warfarin skin necrosis Warfarin embryopathy Factors that may influence bleeding risk: Intensity of anticoagulation Concomitant clinical disorders Concomitant use of other medications Quality of management Conversion from Heparin to Warfarin Initiate AC with heparin Heparin bolus dose 5000u 333u / kg and as per aPTT Enoxaparin (Clexane) 1 mg/kg BD May begin concomitantly with heparin therapy Heparin should be continued for a minimum of four days Time to peak antithrombotic effect of warfarin is delayed 96 hours (despite INR) When INR reaches therapeutic range, discontinue heparin Individualize warfarin dose according to patient response (as indicated by INR) Use of large loading dose not recommended* Increases hemorrhagic complications Does not offer more rapid protection Low initiation doses are recommended for elderly/frail/liver-diseased / malnourished patients *Harrison L, et al. Ann Intern Med 1997;126:133-136. Loading Dose Then Maintenance Dose Daily Dose Maintenance Dose Only Daily Dose Prothrombin Time (PT) Historically, a most dependable “relied upon” clinical test; but: Concept of correct “intensity” of anticoagulant therapy has changed significantly (low intensity) Many thromboplastin reagents with widely varying sensitivities to low levels of vitamin K-dependent clotting factors available Problem addressed by use of INR (International Normalized Ratio) INR: International Normalized Ratio A mathematical “correction” (of the PT ratio) for variations in the sensitivity of thromboplastin reagents (ISI) Allows for evaluation of results between labs and standardizes reporting of the PT Relies upon “reference” thromboplastin ( Patient’s PT in Seconds INR = Mean Normal PT in Seconds ) ISI INR = International Normalized Ratio ISI = International Sensitivity Index known sensitivity to antithrombotic effects of warfarin INR is the PT ratio obtained if “reference” thromboplastin was used J Clin Path 1985; 38:133-134; WHO Tech Rep Ser. #687 983. Trusting the INR Result Ortho 1.00 BFA DADE 1.03 BFA Thromboplastin — Reagent combinations and observed variation in INR 5.5 Behring 1.08 BFA Pacific Hem 1.20 BFA IL Test 1.43 BFA DADE 1.96 BFA 5 Ortho 1.00 ACL 4.5 4 3.5 DADE 1.03 ACL Behring 1.08 ACL Pacific Hem 1.20 ACL IL Test 1.43 ACL DADE 1.96 ACL 3 Ortho 1.00 MLA 2.5 2 1.5 DADE 1.03 MLA Behring 1.08 MLA Pacific Hem 1.20 MLA IL Test 1.43 MLA DADE 1.96 MLA Courtesy A. Jacobson Potential Problems with the INR Limitations Solutions Unreliable during induction Loss of accuracy with high ISI thromboplastin Incorrect ISI assignment by manufacturer Incorrect calculation of INR due to failure to use proper mean normal plasma value to derive PT ratio Thromboplastin reagents with low ISI values (less than 1.5) Use plasma calibrates with certified INR values Use “mean normal” PT derived from normal plasma samples for every new batch of thromboplastin reagent Optimal Frequency of INR Monitoring* vs % In Range 90 % in Range Test Interval 100 80 70 60 50 40 30 More Frequent testing increases % in range 20 10 0 0 7 14 21 28 35 42 49 Days Between Tests Summary 18 published studies: PST Coalition Report, July 2000 Warfarin: Current Indications/Intensity Indication INR Range Target Prophylaxis of venous thrombosis (high-risk surgery) Treatment of venous thrombosis Treatment of PE Prevention of systemic embolism Tissue heart valves AMI (to prevent systemic embolism) Valvular heart disease Atrial fibrillation 2.0–3.0 2.5 Mechanical prosthetic valves (high risk) Certain patients with thrombosis and the antiphospholipid syndrome AMI (to prevent recurrent AMI) 2.5–3.5 3.0 Bileaflet mechanical valve in aortic position, NSR 2.0–3.0 2.5 Optimal INR in AF Adapted from Hylek EM et. al. An analysis of the lowest effective intensity of prophylactic anticoagulation for patients with nonrheumatic atrial fibrillation. NEJM 1996; 335(8):540-6 and Hylek EM and Singer DE. Risk factors for intracranial hemorrhage in outpatients taking warfarin. Ann Intern Med 1994; 120(11):897-902. Signs of Warfarin Over-dosage Any unusual bleeding: Blood in stools or urine Excessive menstrual bleeding Bruising Excessive nose bleeds/bleeding gums Persistent oozing from superficial injuries Bleeding from tumor, ulcer, or other lesion Dosage Adjustment Algorithm Current Daily Dose (mg) 2.5 5.0 7.5 10.0 12.5 INR 1.0-2.0 2.0-3.0 3.0-6.0 6.0-10.0† 10.0-18.0§ >18.0§ † Consider Warfarin Dose Adjustment* Adjusted Daily Dose (mg) Increase x 2 days 5.0 7.5 10.0 12.5 15.0 No change — — — — — Decrease x 2 days 1.25 2.5 5.0 7.5 10.0 Decrease x 2 days 0 1.25 2.5 5.0 7.5 Decrease x 2 days 0 0 0 0 2.5 Discontinue warfarin and consider hospitalization/reversal of anticoagulation oral vitamin K, 2.5–5 mg Oral vitamin K, 2.5–5 mg * Allow 2 days after dosage change for clotting factor equilibration. Repeat prothrombin time 2 days after increasing or decreasing warfarin dosage and use new guide to management (INR = International Normalized Ratio). After increase or decrease of dose for two days, go to new higher (or lower) dosage level (e.g., if 5.0 qd, alternate 5.0/7.5; if alternate 2.5/5.0, increase to 5.0 qd). § Managing Patients with High INR Values Minor or No Bleeding Clinical Situation Guidelines INR >therapeutic range but <5.0, no clinically significant bleeding, rapid reversal not indicated for reasons of surgical intervention Lower the dose or omit the next dose; resume warfarin therapy at a lower dose when the INR approaches desired range INR >5.0 but <9.0, no clinically significant bleeding Patients with no additional risk factors for bleeding; omit the next dose or two of warfarin, monitor INR more frequently, and resume warfarin therapy at a lower dose when the INR is in therapeutic range If the INR is only minimally above therapeutic range, dose reduction may not be necessary Patients at increased risk of bleeding: omit the next dose of warfarin, and give vitamin K1 (1.0 to 2.5 mg orally) Patients requiring more rapid reversal before urgent surgery or dental extraction: vitamin K1 (2–4 mg orally); if the INR remains high at 24 h, an additional dose of 1–2 mg Managing Patients with High INR Values & Bleeding Clinical Situation Guidelines INR >9.0, no clinically significant bleeding Vitamin K1 (3–5 mg orally); closely monitor the INR; if the INR is not substantially reduced by 24 h, the vitamin K1 dose can be repeated Serious bleeding, or major warfarin overdose (e.g., INR >20.0) requiring very rapid reversal of anticoagulant effect: Vitamin K1 (10 mg by slow IV infusion), with fresh plasma transfusion or prothrombin complex concentrate, depending upon urgency; vitamin K1 injections may be needed q12h Life-threatening bleeding or serious warfarin overdose Continuing warfarin therapy indicated after high doses of vitamin K1 Prothrombin complex concentrate, with vitamin K1 (10 mg by slow IV infusion); repeat if necessary, depending upon the INR Heparin, until the effects of vitamin K1 have been reversed, and patient is responsive to warfarin Drug Interactions with Warfarin: Potentiation Level of Evidence †In Potentiation I Alcohol (if concomitant liver disease) amiodarone (anabolic steroids, cimetidine,† clofibrate, cotrimoxazole, erythromycin, fluconazole, isoniazid [600 mg daily] metronidazole), miconazole, omeprazole, phenylbutazone, piroxicam, propafenone, propranolol,† sulfinpyrazone (biphasic with later inhibition) II Acetaminophen , chloral hydrate , ciprofloxacin, dextropropoxyphene, disulfiram, itraconazole, quinidine, phenytoin (biphasic with later inhibition), tamoxifen, tetracycline, flu vaccine III Acetylsalicylic acid, disopyramide, fluorouracil, ifosfamide, ketoprofen, simvastatin, metozalone, moricizine, nalidixic acid, norfloxacin, ofloxacin, propoxyphene, sulindac, tolmetin, topical salicylates IV Cefamandole, cefazolin, gemfibrozil, heparin, indomethacin, sulfisoxazole a small number of volunteer subjects, an inhibitory drug interaction occurred. Drug Interactions with Warfarin: Inhibition Level of Evidence Inhibition I Barbiturates, carbamazepine, chlordiazepoxide, cholestyramine, griseofulvin, nafcillin, rifampin, sucralfate II Dicloxacillin III Azathioprine, cyclosporine, etretinate, trazodone How well does a University Hospital do in managing warfarin therapy? 26 “Inpatient Warfarin Medication Utilization Evaluation” Treatment decisions involving inappropriate assessment of response • 349 records reviewed and assessed by established criteria • 647/2030 (31.8%) warfarin treatment decisions were deemed inappropriate Total = 647 decisions 8% Initial dose too high (52 decisions) Initial dose too low (9 decisions) 1% 10% Different dose from home therapy (63 decisions) 1% 1% Continued home dose but should have been changed (6 decisions) 10% Continued home dose but should have been held (4 decisions) Held dose when therapy should have been restarted (66 decisions) 69% PK/PD not taken into account (447 decisions) Challenges With Conventional Laboratory Testing Challenges for patients’ compliance Patient issues Labor-intensive and higher costs Time for traveling to office or laboratory Ability to travel Need for venous access Scheduling visits Proper handling and delivery of sample Documentation at several time points Potential for communication delays Laboratory to contact provider with results Provider to contact patient with dosage adjustments Jacobson AK. In: Ansell JE, Oertel LB, Wittkowsky AK, eds. Managing Oral Anticoagulation Therapy. 2nd ed. St. Louis, Mo: Facts and Comparisons; 2003;45:1-6. Models of Chronic Anticoagulation Management Laboratory based Vs Patient self testing Routine Medical Care (Usual Care) AC managed by physician or office staff w/o any systematic program for education, follow-up, communication, and dose management. May use POC device or laboratory INR Anticoagulation Clinic (ACC) AC managed by dedicated personnel (MD, RN or pharmacist) with systematic policies in place to manage and dose patients. May use POC device or laboratory INR Patient Self-Testing (PST) Patient uses POC monitor to measure INR at home. Dose managed by UC or ACC Patient Self-Management (PSM) Patient uses POC monitor to measure INR at home and manages own AC dose Home Monitoring Willing to: Considerations for Patient Selection Able to: Learn and perform testing procedure Keep accurate written records Communicate results in timely fashion Participate in a training program to acquire skills/competencies to perform self-testing Generate an INR Understand implications of test result Maintain records Reliable to: Perform procedure with acceptable technique to obtain accurate results www. ASmartWayToTest.com Technology Advances: Offers a new paradigm for monitoring since 1987 Use of capillary whole blood Consistency of INR results Portability Allows fingerstick sampling Appropriate for self-testing Can be done anywhere Simplicity Patient can easily perform test 1. Leaning KE, Ansell JE. J Thromb Thrombolysis. 1996;3:377-383. 2. Ansell JE. In: Ansell JE, Oertel LB, Wittkowsky AK, eds. Managing Oral Anticoagulation Therapy. 2nd ed. St. Louis, Mo: Facts and Comparisons; 2003;44:1-6. Thromboembolism with PST or PSM vs Control Heneghan et al. Lancet 2006;367:404 Major Hemorrhage with PST & PSM vs Control Heneghan et al. Lancet 2006;367:404 Communication with patient doing home monitoring Oral Anticoagulation Patient Self-Testing: Consensus Guidelines for Practical Implementation. Managed Care 2008;17(#10, Suppl 9):1-9 Management of Warfarin During Invasive Procedures For sub-therapeutic or normal INR: Hold warfarin for 3–5 days preprocedure Low-dose heparin (5,000 IU SQ BID); hold warfarin 3–5 days preprocedure and begin LDH therapy 1–2 days pre-procedure Adjusted Dose Heparin (AdjDH): Same as LDH but higher doses of heparin (between 8,000–10,000 IU BID or TID) to achieve an aPTT in upper range of normal or slightly higher midway between doses Enoxaparin (Clexane) 1 mg/kg Full Dose Heparin (FDH): full doses of heparin, IV continuous infusion, to achieve a therapeutic aPTT (~1.5–2x control); implement as for LDH Enoxaparin (Clexane 1 mg / kg B. D.) Restart heparin or warfarin post-op when considered safe to do so Warfarin Dosing in Elderly Patients Mean Warfarin Daily Dose (mg) Patient Age <50 50–59 60–69 70–79 >80 Gurwitz, et al, 1992 (n=530 patients total study) 6.4 5.1 4.2 3.6 ND James, et al, 1992 (n=2,305 patients total study) 6.1 5.3 4.3 3.9 3.5 Increasing age has been associated with an increased response to the effects of warfarin Gurwitz JH, et al. Ann Int Med 1992; 116(11): 901-904. James AH, et al. J Clin Path 1992; 45: 704-706. Warfarin: Dosing & Monitoring Start low Educate patient Initiate 5 mg daily* Stabilize Titrate to appropriate INR Monitor INR frequently (daily then weekly) Adjust as necessary Monitor INR regularly (every 1–4 weeks) and adjust * Elderly, frail, liver disease, malnourished: 2 mg/day Special Considerations in the Elderly: Bleeding Older age associated with increased sensitivity at usual doses Comorbidity Increased drug interactions ? Increased bleeding risk independent of the above Barriers to Warfarin Use Reasons why physicians don’t use coumadin: Risk of hemorrhage: 2.0 Risk of embolus too low: 3.4 Patient Refusal: 3.6 Inconvenience of monitoring: 5.2 Impairs quality of life: 5.2 Belief that aspirin is superior: 5.2 Cost: 5.6 Doubt effectiveness: 6.8 McCrory, et al. Arch Int Med, 1995 Management Recommendations Heparin: For patients starting IV UFH, the initial bolus and the initial rate of the continuous infusion be weight adjusted Bolus 80 units/kg followed by 18 units/kg per h for VTE; Bolus 70 units/kg followed by 15 units/kg per h for cardiac or stroke patients) Use of a fixed dose (bolus 5,000 units followed by 1,000 units/h) rather than alternative regimens (Grade 2C). For outpatients with VTE treated with SC UFH, weight-adjusted dosing (first dose 333 units/kg, then 250 units/kg) without monitoring rather than fixed or weight-adjusted dosing with monitoring (Grade 2C) suggested. For patients receiving therapeutic LMWH who have severe renal insufficiency (calculated creatinine clearance < 30 mL/min), we suggest a reduction of the dose rather than using standard doses (Grade 2C). For OPD start therapy with warfarin 10 mg daily for 1-2 days followed by dosing based on INR measurements Recommend against the routine use of pharmacogenetic testing for guiding doses of VKA (Grade 1B). In acute VTE, start VKA therapy on day 1 or 2 of LMWH or low-dose unfractionated heparin (UFH) therapy (Grade 2C). For patients taking VKA therapy with consistently stable INRs, we suggest an INR testing frequency of up to 12 weeks rather than every 4 weeks (Grade 2B). For patients with previously stable therapeutic INRs a single out-of-range INR of ≤ 0.5 below or above therapeutic, continuing the current dose and testing INR within 1 to 2 weeks (Grade 2C). a single subtherapeutic INR value, not to routinely administering bridging heparin (Grade 2C). For patients taking VKAs, we suggest against routine use of vitamin K supplementation (Grade 2C). For patients treated with VKAs who are motivated and can demonstrate competency in self-management strategies, including the self-testing equipment, we suggest patient self-management rather than outpatient INR monitoring (Grade 2B). For dosing decisions, we suggest using validated decision support tools (paper nomograms or computerized dosing programs) rather than no decision support (Grade 2C). For patients taking VKAs, avoid concomitant treatment with nonsteroidal antiinflammatory drugs, and certain antibiotics (Grade 2C). For patients taking VKAs, we suggest avoiding concomitant treatment with antiplatelet agents except patients with mechanical valves, patients with acute coronary syndrome, or patients with recent coronary stents or bypass surgery (Grade 2C). A therapeutic INR range of 2.0 to 3.0 (target INR of 2.5) rather than a lower (INR < 2) or higher (INR 3.0-5.0) range (Grade 1B) is recommended. For patients with APS with previous thromboembolism, warfarin therapy titrated to a moderate-intensity INR range (INR 2.0-3.0) rather than INR 3.0-4.5 (Grade 2B) recommended. Discontinuation of VKA, should be abrupt rather than tapering of the dose (Grade 2C). Conclusions . . . • • • • • • Anticoagulants (oral and parenteral) top the list for adverse events. Management of warfarin therapy is often poor, even in the best of circumstances. The transition from inpatient to outpatient anticoagulation requires labor intensive systems and processes for successful implementation. Anticoagulation management models include Routine or Usual Care, Anticoagulation Clinics, and PST/PSM (home monitoring) Point-of-care provides an alternative to laboratory testing that is easy, portable, and accurate and allows for testing either by physician or patient Home monitoring requires systems in place to implement and manage results. IDTFs can perform much of the implementation and follow up tracking of results