Nervous System
advertisement

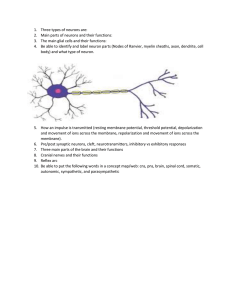
Anatomical Organization of the Nervous System • Central nervous system (CNS) – consists of the brain located within the skull and the spinal cord located within the vertebral foramen – integration and command center of the body • Peripheral nervous system (PNS) – consists of nerves (extensions of the CNS) that connect the CNS to all other locations in the body Nervous System • One of 2 controlling and communicating systems of the body (other is the endocrine system) • Transmit sensory information – send electrical impulses called action potentials (APs) to the CNS • from eyes, skin, blood vessels, ears, digestive tract, joints, muscles, lungs… • Integration – interpretation of sensory information by the CNS • type, location and magnitude of stimulus • Transmit motor information – send APs from the CNS to various effector organs throughout the body • provides a way to respond to stimuli Cells of the Nervous System • The two principal cell types of the nervous system are: – Neurons • hundreds of thousands of neurons extend axons and make synapses all over the body with other neurons, muscles and glands • communicate through action potentials • allows for short response times to changes in homeostasis – Neuroglia • guide developing neurons to make synapses • provide a supportive scaffolding for developed neurons Neuron Types of the Nervous System • Sensory (afferent) – associated with sensory receptors – send APs via the PNS toward the CNS • Interneurons – integrate information within the CNS – receive APs from sensory neurons and initiate APs in motor neurons • Motor (efferent) – send APs via the PNS away from the CNS • All 3 neuron types are used to respond to stimuli – reflex Basic Function of the Nervous System Membrane Potential • Although the total solute concentration in the ICF and ECF are equal, there is an uneven distribution of charged substances across the cell membrane of every cell in the body – creates an electrical potential (energy) between the ICF and ECF – measured as a voltage • in millivolts (mV) – causes the cell membrane to be polarized • a measurable charge difference between the ICF and ECF • The ICF is negatively charged compared to the ECF – a typical membrane potential is –70 mV • In an UNSTIMULATED (resting) cell this potential remains constant and is referred to as the resting membrane potential (RMP) Resting Membrane Potential Basis of the Resting Membrane Potential • Due to the permeability characteristics of the plasma membrane to charged (polar) substances – permeability is the ease in which one substance can move through another substance • Permeable charged substances – K+ – Na+ Basis of the Resting Membrane Potential • In a resting cell, Na+ and K+ are constantly pumped across the cell membrane by the Na+,K+-ATPase maintaining: – a high Na+ concentration in the ECF – a low Na+ concentration in the ICF – a high K+ concentration in the ICF – a low K+ concentration in the ECF Basis of the Resting Membrane Potential Diffusion of Na+ and K+ • There is a constant diffusion of Na+ into the cell by: • Na+ channels that are always open (leaky) • There is a constant diffusion of K+ out of the cell by: • open K+ channels that are always open (leaky) • The permeability of the cell membrane in a resting cell to potassium is approximately 40 times greater than the permeability to sodium – due to a much larger number of potassium leak channels compared to sodium leak channels • When a cell is at rest, the pumping of the Na+,K+ATPase, exactly equals the diffusion of Na+ and K+ – results in a steady state condition Contribution of Na+ to the RMP • If the cell membrane were permeable only to sodium then sodium would diffuse into the cell – as sodium diffuses into the cell it causes the inside of the cell to become positively charged (it only takes a few ions because each ion has a large charge) which begins to reduce additional sodium ion entry (due to repulsion) • Sodium diffusion stops when the inside of the cell has 58 more mV of charge compared to outside (membrane potential = +58 mV) – at this potential, the concentration gradient moving Na+ into the cell exactly balances the positive electric charge repelling Na+ out of the cell – Equilibrium potential for Na+ (ENa) Contribution of K+ to the RMP • If the cell membrane were permeable only to potassium then potassium would diffuse out of the cell – as potassium diffuses out of the cell it causes the inside of the cell to become negatively charged (it only takes a few ions because each ion has a large charge) which begins to reduce additional potassium ion exit (due to attraction) • Potassium diffusion stops when the inside of the cell has 90 less mV of charge compared to outside (membrane potential = -90 mV) – at this potential, the concentration gradient moving K+ out of the cell exactly balances the negative electric charge attracting K+ into the cell – Equilibrium potential for K+ (EK) RMP • Note that the RMP is neither equal to ENa or EK, but is somewhere between these 2 values • If the permeability of these 2 ions through the cell membrane were exactly the same, the RMP would be exactly between the values of ENa and EK, or -16 mV. • However, the permeability of the cell membrane to potassium is approximately 40 times greater than that of sodium due to a much greater number of potassium leak channels. • This causes potassium to have a much greater influence on the RMP compared to sodium, which is why at -70 mV the RMP is closer to -90 mV than +58 mV. Changes in the Resting Membrane Potential • Many cells of the body use the electric potential across the cell membrane to function – the membrane potential changes from its resting value due to a change in the environment of the cell • the change in the membrane potential causes the cell to “respond” to the change in its environment • Changes in the membrane potential from resting values are due to the function of gated ion channels – these channels remain closed (while a cell is at rest) until a change in the environment of the cell (STIMULUS) causes them to open Types of Gated Ion Channels • Gated ion channels only allow the diffusion of 1 (sometimes 2) type of ion across the cell membrane – Ligand-gated channels • open when a specific chemical binds to the extracellular portion of the channel – Stretch-gated channels • open when the plasma membrane is stretched – Voltage-gated channels • open when the membrane potential deviates from resting and reaches a specific voltage Gated Channels • Channel types include some of the following examples – Voltage-gated Ca2+ channels – Stretch-gated Cl- channels – Voltage-gated K+ channels – Ligand-gated Na+ channels • The diffusion of any additional ions across the plasma membrane occurs at a much faster rate than the rate of pumping of the Na+,K+-ATPase – this causes the cell membrane potential to deviate from the resting value Operation of a Ligand-Gated Channel Example: ligand-gated Na+ channel • Closed when a chemical is NOT bound to the extracellular portion of the channel – Na+ cannot enter the cell • Opens when a specific chemical attaches to the extracellular portion of the channel – Na+ diffuses into the cell Operation of a Ligand-Gated Na+ channel Deviations in the Resting Membrane Potential • The opening of a gated ion channel will allow a specific ion to diffuse down its respective gradient across the cell membrane • The membrane potential will deviate from the resting value (-70mV) based on 2 criteria: – the charge of the diffusing ion • either positive (cation) or negative (anion) – the direction of the diffusion • either into or out of the cell Deviations in the Resting Membrane Potential • The ICF becomes less negative when: – a cation diffuses into the cell – an anion diffuses out of the cell • depolarization –reduces the polarity of the membrane as the membrane potential moves toward 0mV • The ICF becomes more negative when: – a cation diffuses out of the cell – an anion diffuses into the cell • hyperpolarization –increases the polarity of the membrane as the membrane potential moves further away from 0mV Deviations in the Resting Membrane Potential • When the gated ion channels close, the cell membrane potential returns to its resting value Gated Channels and the Membrane Potential • When gated channels open: – ions move across the cell membrane down its concentration gradient (HIGH → low) – the number of ions that move across the membrane is relatively small and thus DOES NOT CHANGE the concentration gradient of the ion • The membrane potential deviates because each ion has a large charge associated with it – the movement of only a “few” ions creates a large change in the distribution of electric charge across the cell membrane • After the gated channels have closed, the “few” ions that diffused are quickly moved up the gradient to return the membrane potential to resting Responses to Stimuli • Stimulation of various cells (receptors/sensors) in the body causes the opening of gated channels which changes in the resting membrane potential initiating an electrical impulse – ligand-gated channels are opened in taste buds by the food that is ingested – stretch-gated channels are opened in free nerve endings in the dermis of the skin when bitten by a mosquito – voltage-gated receptors are opened when your lab partner uses an electrical stimulating electrode on your arm Responses to Stimuli • The electrical impulse travels from the stimulated receptor cell to an effector cell (muscle and/or gland) • A change in the membrane potential of the effector cell causes a functional change in the cell allowing for an appropriate response – the salivary glands will secrete saliva into the mouth while the tongue and muscles controlling the jaw will contract, allowing you to chew and swallow or spit out the ingested food – the muscles controlling the arm and hand will contract, allow you swat the mosquito – the muscles of the hand will contract, causing the fingers and wrist to flex Neurons (Nerve Cells) • The transfer of these electrical impulses over large distances is accomplished by the cells of the nervous system called neurons – capable of: • generating/initiating an electrical impulse • sending electrical impulses very rapidly from one location in the body to another • changing the resting membrane potential of other cells within the body including: –other neurons –effector cells of the body • The nervous system is made up of millions of neurons that connect all parts of the body to one another Neuron Anatomy • Dendrites – branched appendages that receive stimuli – respond to a stimuli by opening gated channels • location of stretch or ligand-gated channels • change in the membrane potential of the neuron at the precise location of the stimulus on the cell • Body (soma) – location of organelles, but can also receive stimuli – respond to a stimuli by opening gated channels • location of stretch or ligand-gated channels • change in the membrane potential of the neuron at the precise location of the stimulus on the cell • Axon – long extension of the cell body, that can branch many times which sends the electrical impulse to other cells in the body • location of voltage-gated channels Neuron Initiation of an electrical impulse • The initiation of an electrical impulse occurs at either the dendrites or the body of a neuron – the opening of stretch or ligand-gated channels causes EITHER a depolarization or a hyperpolarization, depending on the charge and the direction of movement of the ion at the location of the opened gated channels • this type of membrane potential change is called a graded (local) potential –a brief, localized change in the membrane potential Graded Potentials • The grade or magnitude of depolarization or hyperpolarization is directly related to the size of the stimulus – determines the number of gated channels that is opened • determines the number of ions that cross the plasma membrane Graded Potentials of Stretch-gated Channels • A small pressure applied to the skin: – causes a small amount of stretch of the cell membrane of the pressure sensing cells of the skin • causes few stretch-gated channels to open –allows few ions to cross the cell membrane • causes a small change of the membrane potential from the resting value • A large pressure applied to the skin: – causes a large amount of stretch of the cell membrane of the pressure sensing cells of the skin – causes more stretch-gated channels to open –allows more ions to cross the cell membrane • causes a larger change of the membrane potential from the resting value Graded Potentials • Decrease in magnitude with distance from the site of stimulation – as ions move into/out of the cell through opened gated channels, they diffuse away from the opened gated channel • as the ions diffuse away from the opened gated channel the concentration of the ion decreases –as the ion concentration decreases, so does it’s influence on the membrane potential • the further away from the stimulus, the closer the membrane potential is to the resting value Function of Graded Potentials • The purpose of graded potentials in the dendrites or soma is to cause (or prevent) the opening of voltagegated ion channels in the axon of the neuron – open when the membrane potential in the axon has been depolarized to a minimum value – the opening of voltage-gated channels in the axon will create a membrane potential change in the axon called an action potential • the action potential will “travel” down the length of the axon and all of its branches to the axon terminus Action Potentials (APs) • A very rapid sequence of membrane potential changes due to the opening and closing of voltagegated Na+ and voltage-gated K+ channels • There are 3 sequential phases to an AP in a neuron: – Depolarization • a reduction in the polarity of the membrane potential – Repolarization • a return of the membrane potential towards the resting value – Hyperpolarization • the membrane potential reaches values more negative than the resting value • All APs in a neuron have the same magnitude regardless of the size of the stimulus (not graded) Action Potential Threshold and Action Potentials • The initiation of an AP occurs at the beginning of the axon called the initial segment and requires that the membrane potential at the axon be depolarized to threshold – the minimum amount of depolarization required to initiate an action potential • typically -55mV • causes the opening of voltage-gated Na+ channels Threshold and Action Potentials • Threshold can be reached by a depolarizing graded potential in the dendrites or soma of a neuron – small (weak) stimuli DO NOT initiate an AP because the magnitude of the graded potential at the axon is TOO SMALL to depolarize the membrane at the axon to threshold • subthreshold stimuli – large (strong) stimuli DO initiate an AP • threshold stimuli • All-or-none phenomenon – action potentials either completely, or not at all Ionic Basis of Action Potential (Resting State) • Na+ and K+ channels are closed Ionic Basis of Action Potential (Depolarization) If a strong enough stimulus is presented to the cell, the membrane potential depolarizes to threshold (-55mV) causing: – Na+ channels to open • Na+ enters the cell (diffusion) –membrane potential continues to depolarize to +30mV • K+ channels slowly begin to open Ionic Basis of Action Potential (Repolarization) Membrane potential reaches peak depolarization of +30mV causing: • Na+ channels to close • K+ channels to open – K+ exits the cell (diffusion) • the membrane potential returns toward resting values (repolarization) Ionic Basis of Action Potential (Hyperpolarization and Return to Resting) • K+ channels remain open • This causes more than enough K+ to leave the cell resulting in hyperpolarization of the membrane potential • Eventually, the K+ channels close, allowing the membrane potential to return to resting Refractory Periods Absolute Refractory Period • The absolute refractory period: – is the time during an action potential that another action potential CANNOT be initiated • no matter how strongly the dendrites/soma are stimulated – ensures that each action potential created is separated from one another so that the body can interpret stimuli accurately – is time required for the voltage-gated Na+ channels to be “reset” • required for the channels to open again Relative Refractory Period • The relative refractory period: – is the time after the absolute refractory period until the membrane potential returns to the resting value • During this time another action potential CAN be initiated – requires a stronger than normal stimulus at the dendrites • during this time some of the voltage-gated Na+ channels have been “reset” while others have not Propagation of an Action Potential • Once an action potential has been initiated at the beginning of the axon, it must “travel” (propagate) along the length of the axon to the axon terminus • The influx of Na+ into the cell during depolarization causes the membrane potential in “front” of the opened Na+ channels to depolarize to threshold • Reaching threshold opens up the Na+ channels in “front” of the site of the action potential causing an action potential to be created in this new location • As the next group of Na+ channels begins to open, the ones “behind” them are closing • The impulse continues to propagate away from its point of origin to the axon terminus • “the domino effect” Propagation of an Action Potential Propagation Velocity of an Action Potential • The propagation velocity is the speed at which the action potential propagates along the length of the axon • Conduction velocity depends on: – axon diameter (thickness) • the larger the diameter, the greater the conduction velocity – presence of a myelin sheath • dramatically increases impulse speed –to speeds up to 300 mph • more effective than increasing axon diameter • The human body uses both methods to maximize propagation velocity Myelin Sheath • White, fatty (lipid), segmented covering around most long axons • Increases propagation velocity of APs by electrically insulating the axon • Formed by Schwann cells – wraps around the axon many times with its plasma membrane – encloses the axon with many concentric layers of lipid bilayers Myelin Sheath Myelin Sheath Formation Nodes of Ranvier • The nodes of Ranvier are: – gaps between the Schwann cells • naked axon segments – the ONLY locations of voltage-gated Na+ and K+ channels • in large densities • ONLY locations where an AP can be generated along the length of the axon Saltatory Conduction • Ions pass through a myelinated axon only at the nodes of Ranvier creating an action potential – due to the large density of voltage-gated Na+ channels creates a large electrical field surrounding the node • causes the cell membrane to reach to threshold at a large distance away (the next node) –creates and AP at the next node • The action potential jumps from node to node – much faster conduction rate compared to unmyelinated axons (of the same diameter) Nodes of Ranvier and Saltatory Conduction Saltatory Conduction Axon Termini and Synapses • When the AP reaches the axon termini the impulse must be transmitted to the next cell in the path to the effector • A synapse is the junction between 2 cells where the impulse is transmitted from one cell to another : – Presynaptic cell (before synapse) – Postsynaptic cell (after synapse) – found between: • 2 neurons • a neuron and an effector cell (muscle or gland) – 2 general types include: – chemical – electrical Axon Termini and Synapses Chemical Synapses • Composed of 3 parts: – axonal terminal of the presynaptic neuron • contains synaptic vesicles –filled with a neurotransmitter (chemical/ligand) – receptor region on the postsynaptic cell which contains ligand-gated channels – fluid-filled space between the cells (synaptic cleft) • separates the presynaptic and postsynaptic cells Chemical Synapse Synaptic Cleft: Information Transfer • An action potential that arrives at the axon terminus of the presynaptic cell causes the opening of voltagegated Ca2+ channels – causes Ca2+ to diffuse into the cytoplasm of the presynaptic cell • triggers the exocytosis of neurotransmitters into the synaptic cleft • The neurotransmitters diffuse across the cleft and open the ligand-gated channels on the postsynaptic cell – causes ions to cross the cell membrane and result in a graded potential • postsynaptic potential –depolarization or hyperpolarization Synaptic Cleft: Information Transfer Postsynaptic Potentials The 2 types of postsynaptic potentials are: • EPSP (excitatory postsynaptic potentials) – depolarizing graded potentials – causes the membrane potential move towards threshold which increases the chances that an AP will be initiated in an axon • IPSP (inhibitory postsynaptic potentials) – hyperpolarizing graded potentials • causes the membrane potential move away from threshold which reduces the chances that an AP will be initiated in an axon Excitatory and Inhibitory Postsynaptic Potentials EPSPs and IPSPs Summate • A single EPSP CANNOT initiate an action potential – EPSPs must summate (add) to bring the membrane potential to threshold at the axon • Temporal summation – postsynaptic potentials are generated at a single location at a high frequency • Spatial summation – postsynaptic potentials are generated at different locations at the same time • IPSPs can also summate with EPSPs – cancel each other out Temporal Summation Temporal Summation Spatial Summation Myelination of Neurons of the Nervous System • Some neurons in the CNS are myelinated, while most are unmyelinated • All of the neurons in the PNS are myelinated • Areas of the CNS that are made of myelinated neurons are called white matter – represent the locations of long sensory and motor neurons • Areas of the CNS that are made of unmyelinated neurons are called gray matter – represent the locations of short interneurons which make many synapses for integration to process sensory information and initiate motor information Spinal Cord • The spinal cord is attached to the brain and extends to the lumbar region of the vertebral column • Functions include: – integration of basic stimuli presented to the body below the neck through simple reflexes • withdrawal reflex in response to pain – sending sensory and motor information to and from the brain Spinal Cord Anatomy • Dorsal (posterior) horns (left and right) – sensory information enter the cord on the dorsal aspect where they synapse with interneurons or motor neurons – extend into dorsal roots and ganglia (group of cell bodies outside the CNS) • Ventral (anterior) horns (left and right) – motor information exits the cord on the ventral aspect where they control effectors (muscle or glands) – extend into motor roots • Dorsal and ventral roots merge together to form spinal nerves Spinal Cord Anatomy Brain Cerebral Cortex • 4 lobes – frontal, parietal, temporal and occipital – location of interneurons for perception of all senses – site of memory, emotion, learning – site of initiation of voluntary skeletal muscle contraction The Cerebellum • Protrudes under the occipital lobes of the cerebrum • Makes up 11% of the brain’s mass • Modifies the motor information leaving the motor cortex – provides precise timing and appropriate patterns of skeletal muscle contraction to maintain balance and coordination • Cerebellar activity occurs subconsciously Brain Stem • Comprised of the pons and the medulla oblongata • Clusters of neurons (brain centers) in regions of the pons and medulla control the basic life functions: – heart rate • controlled by the cardioacceleratory and cardioinhibitory centers in the medulla – blood pressure • controlled by the cardioacceleratory, cardioinhibitory, and vasomotor centers in the medulla – breathing rate • controlled by the inspiratory and expiratory centers in the medulla and pons, respectively • Control of effectors occurs through the Autonomic Nervous System Peripheral Nervous System • The PNS consists of nerves (bundles of axons) – send APs to and away from the CNS – 12 pairs (left and right) of cranial are connected to the brain and 31 pairs (left and right) of nerves are connected to the spinal cord • Sensory (afferent) – all axons carry impulses from sensory receptors via the PNS to the CNS • Motor (efferent) – all axons carry impulses via the PNS from CNS • Mixed – a mixture of sensory and motor neurons that carry impulses via the PNS to and from CNS – most common type of nerve in the body Nerves • Nerve – cordlike organ of the PNS consisting of axons enclosed by connective tissue • Connective tissue coverings include: – Endoneurium • loose connective tissue that surrounds each individual axon – Perineurium • coarse connective tissue that bundles axons into fascicles – Epineurium • tough fibrous connective tissue around a nerve Structure of a Nerve Reflexes • A rapid, predictable motor response to a stimulus • Reflexes can be: – simple • involve peripheral nerves and the spinal cord –rapid – learned (acquired) • involve peripheral nerves and require thought –slower • Following a stimulus, the sensory and motor information of a reflex follows a pathway called a reflex arc – in many spinal reflexes, the effector is nearby the location of the stimulus Reflex Arc • There are five components of a reflex arc – Receptor • detect stimulus – Sensory neuron • transmits the afferent impulse to the CNS – Integration (control) center • region within the CNS where synapses (processing of sensory info) occur – Motor neuron • sends efferent information to an effector – Effector • muscle fiber or gland that responds to the efferent impulse • the activity of the effector depends upon the magnitude of the stimulus Sensory Receptors • Structures specialized to respond to stimuli: – nerve endings (dendrites of neurons) – sense organs • nerve endings combined with other tissue types to enhance detection of a stimuli –example: taste buds • Mechanoreceptors – respond to touch, pressure, stretch and itch • Thermoreceptors – respond to changes in temperature • Photoreceptors – respond to light • Chemoreceptors – respond to chemicals • Nociceptors – respond to pain Neural Integration of the CNS • Qualitative information (salty, pain or temperature) depends upon which neurons are propagating APs • Quantitative (strength) information depend on: – the number of neurons that are firing APs – the frequency of APs fired per neuron Functional Organization of the Nervous System Sensory Division of the Peripheral NS Sensory division • made of afferent neurons – somatic • sensory neurons send APs from skin, skeletal muscles, and joints – visceral • sensory neurons send APs from organs within the abdominal and thoracic cavaties Motor Division of the Peripheral NS Motor division • made of efferent neurons control the action of effectors – somatic • motor neurons send APs to voluntary skeletal muscle – visceral • motor neurons send APs to involuntary cardiac muscle, smooth muscle and glands –a.k.a. the Autonomic Nervous System (ANS) –2 antagonistic (opposing) divisions • Sympathetic • Parasympathetic –the two divisions control the same effectors (with few exceptions) but create opposite responses in the effectors Motor Pathways of the Somatic Nervous Division vs. Autonomic Nervous Division Autonomic Nervous System • Visceral motor neurons of the Peripheral NS control the activity of involuntary effectors such as cardiac muscle, smooth muscle and glandular secretion affecting: – heart rate – breathing rate – sweating – digestion – blood pressure • Action potentials in these motor neurons are initiated in the medulla oblongata and the pons – these motor neurons exit the brain by: • descending tracts of the spinal cord –exit spinal cord via spinal nerves • cranial nerves Function of the Sympathetic Division • The sympathetic division is called the “fight or flight” system – activated when the body needs to expend energy • Involves E activities • exercise, excitement, emergency, and embarrassment • Promotes necessary changes during these activities – increases heart rate, blood pressure, respiration rate, blood flow to skeletal muscles, glucose metabolism – decreases the activity of and blood flow to the digestive system organs • Its activity is illustrated by a person who is threatened Function of the Parasympathetic Division • The parasympathetic nervous system is called the “rest and digest” system – activated when the body needs to conserve energy • Involves the D activities – digestion, defecation, and diuresis (urination) • Promotes necessary changes during these activities – decreases heart rate, blood pressure, respiration rate, blood flow to skeletal muscles, glucose metabolism – increases the activity of and blood flow to the digestive system organs • Its activity is illustrated in a person who relaxes after eating a meal Efferent Pathways of the ANS • Efferent pathways of the ANS consist of a two-neuron chain between the brain or spinal cord and the effector – synapses between the neurons occur at ganglions – The cell body and dendrites of the preganglionic neuron is located in the CNS and the axon extends along a nerve to the ganglion – The cell body and dendrites of the postganglionic neuron is located in the ganglion and the axon extends to an effector organ Organization of the Sympathetic Division Organization of the Parasympathetic Division Motor Pathways of the Somatic Nervous Division vs. Autonomic Nervous Division • All somatic motor neurons exocytose ACh – ACh binds to nicotinic acetylcholine receptors on the skeletal muscle fiber leading to its contraction • All preganglionic motor neurons exocytose ACh – ACh binds to nicotinic acetylcholine receptors on the postganglionic neuron creating an AP • All parasympathetic postganglionic motor neurons exocytose ACh – ACh binds to muscarinic acetylcholine receptors on the effector tissue/organ causing a response • All sympathetic postganglionic motor neurons exocytose norepinephrine NE – NE binds to adrenergic receptors on the effector tissue/organ causing a response Efferent Sympathetic vs. Parasympathetic Effects of Neurotransmitters of the ANS • The way the 2 divisions of the ANS can create opposite responses in the effectors that they control is by the release of different neurotransmitters onto the cells of the effectors • The cells of each organ controlled by the ANS have membrane receptors to BOTH ACh and NE – organs are dually controlled • The response of the organ is determined by the identity of the neurotransmitter released – the binding of ACh to its receptor will cause the effector to respond in one way – the binding of NE to its receptor will cause the effector to respond in the opposite way • The effect of ACh and NE is effector specific – NE increases heart rate, ACh decreases heart rate – NE decreases the secretion of saliva, ACh increases the secretion of saliva Dual Control by the Sympathetic and Parasympathetic Systems