Recognizing Different Sports Injuries
advertisement

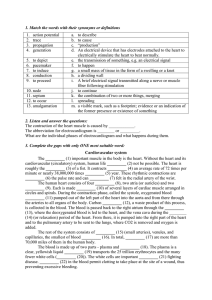
Musculoskeletal Assessment History • This is the information gathering and recording phase of the assessment. • The history should give a clear idea of what the problem is, how to treat the condition and how long it will take for recovery. • The history helps develop a rapport with the athlete, determine the type of person the athlete is and determines the athletes expectations and concerns about the injury. . History Questions • Questions should be orderly and progress from one to the other. • Keep questions simple and relevant. Listen carefully and clarify information. • Use questions that will encourage cooperation and confidence as well as keep the athlete calm and relaxed. • Remain professional at all times. Observations • This is the looking phase of the assessment. • Watch how the athlete moves. • Is the athlete limping? Having difficulty removing shirt or other clothing? • Have female athletes in sports bra and shorts and male athletes in shorts to enable you to look at entire person. What to look for Posture head position shoulder position back alignment pelvis position knee level ankle and foot position arches Athletes willingness to move body parts Facial expressions as athlete moves. Differences between left and right sides of the body. Deformity Asymmetry Muscle spasm Muscle development Muscle atrophy Limb size; shape; colour; temperature Scars Functional Tests This phase of the assessment determines the type of structure that is injured through active, passive and resisted testing. The tissues are divided into contractile and inert. Contractile tissues are; muscle belly, tendon and their attachment to the periosteum. Tension may be applied to these structures by stretching or by using resisted isometric contraction. Inert tissues are; ligament, capsule, fat pad, blood vessels, cartilage, meniscus, nerves, skin. These structures hove no inherent capacity to relax or contract. Tension may be applied to these structures by stretching during a passive movement. Active Movement Active movements tell the therapist: •The athlete=s willingness to move the joint; •The athlete=s active range of motion; •That the muscle can move the joint and body part; •The quality of movement in the range of available motion; •How the joint surfaces are working or the state of the joint. Active Movement How to test: • Ask athlete to move the joint through as much of the range as possible, noting where pain occurs in the range; • Measure or approximate the degrees of range of motion at the joint; • Compare the ranges to opposite limb where possible; • Test each movement at the joint. • Note any pain, location of pain, type of pain, sensations, sounds or abnormal movement during testing. Active Movement Results: • Range of motion may be normal, limited or excessive in any one, combination of or all range(s) of motion at he joint. • There may be pain throughout the range, at certain points in the range or at the end of range. There may not be pain in the range of motion. Passive Movements Passive movement tell the therapist: The state of the inert structures. Pain at the extremes of movement indicates; a painful structure is stretched or being squeezed. A painful arc indicates impingement. Limited range and painless indicates possible symptomless osteoarthritis. Full range and pain free indicates no inert structure involved. Passive Movements How to test: The therapist gently lifts the limb through the full possible range of motion available without forcing the joint. The athlete must be relaxed. Measure or approximate the degrees of motion and compare to opposite limb. Test each anatomical range of motion. Passive Movements Results: • The range of motion may be limited, normal or excessive. • Pain or muscle spasm may be present at any point in the range. • There may be pain, limitation or both in any or all ranges of motion. Resisted Isometric Contraction Resisted testing tells the therapist: The state of contractile structures and their nerve supply. The degree of strength on a scale of 0-5; Gone 0 no contraction felt. Trace 1 can feel muscle tighten but no movement produced. Poor 2 produces movement with gravity eliminated but can not function against gravity. Fair 3 can raise part against gravity. Good 4 can raise part against gravity with outside resistance. Normal 5 can overcome a greater amount of resistance than a good muscle. Resisted Isometric Contraction How to test: • Position athlete so the part being tested is in a neutral position. • Stabilize the body part being tested, make sure athlete is comfortable. • Ask athlete to meet your resistance as you apply pressure against the muscle group you want to test. • Use slow gradual increase in pressure until a maximal contraction is felt. • Hold the contraction for five seconds and gradually relax. • The limb should not move through any range of motion. Resisted Isometric Contraction Results: Strong and painless indicates no neurological deficit or lesion involving the muscle or tendon. Strong and painful indicates no neurological problem. There is a minor contractile tissue injury. Weak and painless indicates there may be some interruption of the nerve supply to the muscle or there may be a complete rupture of the muscle or tendon. Weak and painful indicates there may be a partial rupture of tendon or muscle. Special Tests This phase of the assessment is used to test specific structures that are suspected as injured after completing functional tests. Special tests are also used to rule out the uninjured structures. Eg. Tap test is used to rule out fracture and distal pulse check is used to rule out artery interruption. Palpations Palpations are used to: • Isolate the structures that are injured. • Discriminate differences in tissue tension. • Distinguish differences in tissue texture. • Detect abnormalities in shape structure and type of tissues. • Feel temperature variations. • Note abnormal sensations.