File

Lec.10, 11 Blood Physiology Done By Ehab Ahmed
Platelets formation (thrombopoiesis) :
Platelets are formed in the bone marrow from stem cell which will differentiate to megakaryocytes, from which platelets will be produced.
Negative feedback mechanism is the main role for RBCs production.
A Decrease in platelets will stimulate the release of thrombopoietin (glycoprotein hormone) from the liver and kidney. Which will stimulate the bone marrow to produce and release platelets to the circulation. While an increase in platelets will inhibit thrombopoietin and hens a decrease in platelets production
.
The normal range of platelets is 200000 400000/mm3. The lifespan of the circulating platelets is 7- 10 days .
The old platelets are destroyed by the spleen and the liver.
If the number of platelets is too low (thrombocytopenia), excessive bleeding will occur, while if its number is too high
(thrombocytosis), blood clot can occur which block blood vessels, and may cause stroke (CVA) or heart attack
.
CVA= cerebrovascular accident
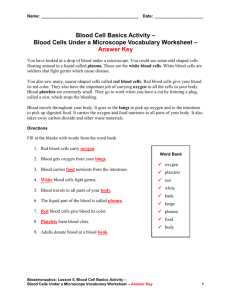
Primary hemostasis:
Bleeding will be stopped from pin-prick injury. It includes:
1. Vasoconstriction: it is due to:
Neural reflex, it is initiated by injury of the nerve fibers surrounding the blood vessels.
Thromboxane A2 and Serotonin; they are released from the platelets.
2. Platelets aggregation (plug): When a blood vessel is injured, the platelets will adhere to the exposed collagen fibers, and some of these platelets will rupture, releasing Thromboxane A2 which help in further platelets aggregation and adhesion.
Platelet aggregation will also need the presence of plasma clotting factor (factor VIII).
/ http://ninevehmedicine.weebly.com
ةيناثلا ةلحرملا ىونين بط بورك
Lec.10, 11 Blood Physiology Done By Ehab Ahmed
Secondary hemostasis (coagulation):
It is the mechanism by which the bleeding will be stopped from a large injured area of blood vessel. The large injured area will be converted into Small areas (by fibrin) which are easily blocked by platelets and RBCs.
The mechanism of blood coagulation (clot formation): involves three stages: a) Formation of prothrombin activator complex : The complex includes various plasma clotting (coagulation) factors, which is formed via the extrinsic or intrinsic pathway, as a response to vascular injury. b) Thrombin formation : The prothrombin activator complex will activate the prothrombin to form Thrombin, in the presence of calcium ions. Thrombin induces many actions:
(1) It has a positive feedback mechanism.
It activates some of the plasma clotting factors (V, VIII, and XI), causing increase in the formation of itself.
(2) It stimulates the platelets to release its content causing platelets aggregation.
(3) It activates fibrinogen to form fibrin. c) Fibrin formation : thrombin activates fibrinogen to form two peptides (A and B). These two peptides have the ability to polymerase together to form the fibrin molecules. Thrombin will also convert factor XIII to its active form, which will initiates bonds between the fibrin molecules (in the presence of Ca +2 ), which will become insoluble. Then this fibrin mesh will trap RBCs and platelets, resulting in clot (coagulation) formation, which will stop bleeding and also prevent bacteria from entering the body.
Fibrinolysis
Is the process by which the closed (coagulated) blood vessels will become open and permeable to the blood flow. The clot will be resorbed by plasma enzyme called plasmin, which has a fibrinolytic action.
/ http://ninevehmedicine.weebly.com
ةيناثلا ةلحرملا ىونين بط بورك
Lec.10, 11 Blood Physiology Done By Ehab Ahmed
Plasminogen which is a plasma protein synthesized in the liver will be activated and converted into plasmin by plasminogen activator enzyme synthesized and released from the endothelial cells.
Factors keep the Blood as a Fluid (prevent coagulation of blood) in Blood vessels:
1) Smooth endothelial surface . Which will prevents platelets aggregation.
2) The endothelial surface is negatively charged which repel the negatively charged platelets and proteins, preventing clot formation.
3) Heparin : is an anticoagulant plasma enzyme.
4) Plasmin : is a fibrinolytic plasma enzyme.
5) Antithrombin : it inhibits thrombin formation.
6) Protein C: is a major physiological anticoagulant. Impaired action of protein C may lead to a thrombotic tendency.
7) The continuous movement of blood . Therefore, stasis of blood will enhance thrombus formation, as in deep vein thrombosis.
Note : Vitamin K is essential for the formation of many plasma clotting factors by the liver. Therefore, it is given to patients with severe bleeding, or to patients with overdose of anticoagulant drugs as warfarin.
Fetal red blood cells
The affinity of fetal RBC (Hb) to o
2
is more than maternal RBC
/ http://ninevehmedicine.weebly.com
ةيناثلا ةلحرملا ىونين بط بورك
Lec.10, 11 Blood Physiology Done By Ehab Ahmed
Hemostasis
/ http://ninevehmedicine.weebly.com
ةيناثلا ةلحرملا ىونين بط بورك
Lec.10, 11 Blood Physiology Done By Ehab Ahmed
Hemophilia (for information)
وا ريصقت وا اطخ نم ناك امو الله نم وهف قيفوت نم ناك ام
..........ينم وهف ةمولعملا يف صقن
/ http://ninevehmedicine.weebly.com
ةيناثلا ةلحرملا ىونين بط بورك