Buprenorphine in Medication Assisted Treatment
advertisement

Buprenorphine in Medication
Assisted Treatment (MAT):
Problem or Solution?
Quintin Thomas Chipley, M.A., M.D., Ph.D.
and
Greg Jones, M.D., ABFM, ABAM, MRO
Prepared for CAPTASA 2016
DISCLOSURES
Neither presenter has any financial interest in any mode of
treatment as discussed in this presentation.
Quintin Chipley is employed at the University of Louisville as a
counselor to students at the Health Science Center. The U of L
is gracious to allow Chipley latitude to pursue professionallyrelevant endeavors outside of his work duties, but the
university should not be considered responsible for the
opinions and conclusions offered in this presentation.
Greg Jones is the medical director of the Kentucky Physicians
Health Program. Although that organization continues to be a
long-standing supporter of CAPTASA, and also supports Dr.
Jones’ relevant professional endeavors exterior to his
employment, the KPHF should not be considered responsible
for the opinions and conclusions offered in this presentation.
OVERVIEW
• HISTORY of BUPRENORPHINE and its use in
Medication Assisted Treatment1
• Problems observed in the research-and-policy
literature regarding Buprenorphine MAT
• Clinical anecdotes suggesting problems which
need future research
• Preliminary report on descriptive statistical data
gathered from The Healing Place, men’s and
women’s campuses, Louisville, Kentucky.
1
The material for the history of buprenorphine is taken from an excellent, well-balanced,
and carefully researched article: Nancy D. Campbell and Anne M. Lovell. “The History of the
Development of Buprenorphine As an Addiction Therapeutic.” Annals of the New York
Academy of Sciences. Issue: Addiction Reviews. 1248. 2012. 124-139. Referred to in the
following as Campbell and Lovell, 2012.
PART 1
HISTORY of BUPRENORPHINE
and Its Use in
Medication Assisted
Treatment
Buprenorphine:
A Tale of Markets, Labs, and Laws
Five Periods of Development, Pitch, and Legislation
1) 1966- 1978: Marketplace: Reckitts (a British household-chemicals manufacturer)
search for a non-addictive opiate analgesic which they hope can be nonprescription.
They discover buprenorphine in 1966 and start human trials.
Laboratory: In 1975, buprenorphine garners interest among U.S. researchers as a
possible addiction treatment before approved as analgesic use in U.K. in 1978.
2) 1978- 1982: Market: Poor sales as an injectable analgesic for acute pain.
Lab: U.S. researchers classify it as partial agonist/ antagonist within the larger groups
of antagonist opioids. These researchers want to find a “magic bullet” antagonist.
3) 1982 –1993: Market: sublingual for acute pain introduced, but Reckitts has been
losing interest due to weak sales; sells most marketing rights to other companies.
Lab: U.S. researchers want to make it an addiction treatment. French clinicians are
already using it off-label as a “harms reduction” addiction treatment.
4) 1993 - 2002: Market, Lab, and Law mingle: search for new indications (e.g. refractory depression (not labelled for this use yet, but pay attention to the
implications); treating opiate addiction; France officially allows use for addiction
treatment. Drug Abuse Treatment Act (DATA) of 2000 in U.S. allows outpatient office
treatment of addiction unlike specially licensed clinics required for methadone.
5) 2002 to the present: Market, Lab and Law merge: labelled use for treating “opiate
addiction” gains FDA approval in 2002, to fill the demand created by DATA 2000.
The first period:
1966-1978
• Buprenorphine, a semisynthetic opioid derived from
thebaine, is isolated in 1966 by the British company
Reckitt and Coleman, now named Reckitt Benckiser.
They had hoped to find an analgesic for acute pain that
would be as effective as morphine, but non-addictive
and eligible for over-the-counter sales.
• Buprenorphine entered human trials in 1971 and was
approved for market in the United Kingdom in 1978.
The British company began supplying buprenorphine
as a research drug to the U.S. A.R.C. in Lexington, KY. In
1975, strong interest in buprenorphine as a possible
drug with which to treat addiction began at that
location.
Second Period: 1978-1982
• The injectable form of buprenorphine failed to
secure consistent choice-of-use among physicians
because the suppression of acute pain was poor.
• Even at prescribed doses, the medication proved
to be addictive, though this clinically documented
fact contradicted conclusions drawn from a 1978
study (see next slide).
• A sublingual formulation was introduced in 1982.
Second Period: 1978-1982
(Continued)
• “In 1979, Jasinski classified the narcotic antagonists into three groups: (1)
compounds that produced agonistic effects that do not resemble
morphine (nalorphine and cyclazocine), (2) compounds that do not
produce agonistic effects (naloxone and naltrexone), and (3) antagonists
that produce agonistic effects that resemble those of morphine because
they are also partial agonists of morphine. By then, six category 1 narcotic
antagonists had been introduced as analgesics with low abuse potential.
According to Jasinski’s scheme, propiram and buprenorphine fit category
3. Interest shifted to these ‘partial agonists of the morphine type,’ which
did not constitute a homogenous class due to their intrinsically different
capacities for producing euphoria, sedation, and psychotomimetic
effects.” (Campbell and Lovell, 2012, p. 132; red-font emphasis added by presenter.)
PAY ATTENTION TO THE ASSUMPTION OF “intrinsically different.” Also, this is when Jasinski begins citing
his 1978 study to declare “it [buprenorphine] produced ‘very little physical dependence’ even with
chronic administration .” (Campbell and Lovell, 2012, p. 132.) There is a real problem (though we do NOT
consider it an intentional misrepresentation) with the way Jasinski interpreted the data reported in
Jasinski, D.R., Pevnick, J.S. and Griffith, J.D., “Human Pharmacology and Abuse Potential of the Analgesic
Buprenorphine: A Potential Agent for Treating Narcotic Addiction,” Archives of General Psychiatry, 35,
April 1978, 501-516. In that study, only three subjects completed the active treatment arm of the study,
and the primary measure of “physical dependence” was degree of dysphoria created when administered
naloxone as a reversal antagonist. Here is the problem: naloxone and buprenorphine are so similar in
avidity for mu-receptor sites that the full antagonist naloxone is a poor competitor against buprenorphine
compared to the way naloxone molecules can dislodge morphine or heroin from receptors and then
defend against their return to reoccupy the receptor.
Third Period:
1982- early 1990’s
• The injectable forms and the sublingual forms of
buprenorphine were available but not much-used for
analgesia. By the early 1990’s, French physicians began
using the sublingual forms off-label to reduce needlesharing among addicts with the goal of reducing HIV
infections.
• U.S. government researchers with the famous
“Narcotics Farm” in Lexington, KY had moved to
Maryland as the ARC after 1979 (and was renamed the
NIDA Intra Mural Research Program in the 1990’s.)
Donald Jasinski was one of these scientists.
Third Period:
1982- early 1990’s (CONTINUED)
In a 1983 meeting of the Committee on Problems of Drug
Dependence (CPDD), a group under the National
Academy of Sciences, meeting,
“Jasinski spoke to buprenorphine’s advantages over
naltrexone, noting that his subjects liked buprenorphine
better, and ‘felt comfortable on it. The induction of a
feeling state that they found salient following
buprenorphine was certainly there. . . Most of our
subjects told us that it was, in fact, the most reinforcing
drug that they had ever used’ (p. 95). Despite this
caution, buprenorphine was offered as a ‘safe and
effective mode of pharmacotherapy for heroin
addiction.’”
Campbell and Lovell 2012, p. 133. Font emphasis added by presenter.)
Third Period:
1982- early 1990’s (CONTINUED)
“But the shift from research to industrial drug development for addiction
treatment took off at the intersection of two trajectories: formal interest on
the part of NIDA and a change of orientation within Reckitts. In 1989, the U.S.
Congress mandated that a Medications Development Program be established
in NIDA. The following year, NIDA established the Medications Development
Division (MDD) to develop close working relationships between academia,
the pharmaceutical industry, and government agencies, including the FDA, so
as to develop and evaluate addiction treatment medications to the point that
they could go through the FDA approval process.[…. ]The time was propitious
for Reckitts, as well. Disappointed with its analgesia business, the company
had contracted out buprenorphine commercialization to numerous
companies worldwide and had abandoned ethical1 drug development in the
early 1980s.” (Campbell and Lovell, 2012, p. 134. Emphasis added)
1
“Ethical” is used here in a very specific sense of “for human use.” It does not mean “in accord
with guiding principles of acceptable behavior and judgement.” Reckitts had been mostly a
household-chemical (that is, Lysol, etc.) manufacturing company. Their disappointing foray into
analgesic medication had burned them financially, and they had returned to their origins. They
probably would have kept their products under the kitchen cabinet -- and out of the medicine
cabinet -- if NIDA had not aggressively courted them to reconsider their own product,
buprenorphine, for the new indication of opiate-addiction treatment.)
Fourth Period:
1993-2002
“In 1993,MDD also approached Reckitts about formalizing
their already existing mutual interest in developing
buprenorphine for addiction treatment. NIDA was
interested in buprenorphine by itself and in combination
with naloxone (to prevent diversion).1 Reckitts was NIDA’s
obvious choice for a Cooperative Research and
Development Agreement (CRADA), as another company
would have had to conduct safety and toxicology studies
from scratch for a new indication.” Campbell and Lovell 2012, p. 134.)
1Adding
naloxone to methadone as a diversion-deterrent had been proposed
many years before, though it had not been actively pursued because officials felt
that confining methadone to dedicated, clinic-only-distribution would blunt
diversion sufficiently. Their idea to add naloxone as diversion prevention was
theory-driven rather than experimentally well-demonstrated, either for
methadone or for buprenorphine. The theory presupposes that all brains basically
respond similarly. If you believe that brains prone to addiction work differently
than those not prone to addiction, the theory will not be convincing.
Fourth Period:
1993-2002 (CONTINUED)
In 1994, France and some countries in Asia approve
buprenorphine for labeled use in opiate addiction
treatment as an attempt to reduce HIV infections
from shared needles. The use is explicitly
understood as “harms reduction.”1 Reckitts begins
buying back it rights to the drug. The same years,
U.S. gave Reckitts the CRADA approval, and
included a 7 year “orphan drug” marketing
protection based entirely on economic risk. This is
the first medication granted “orphan” status on an
economic argument.
1It
is crucial to distinguish “harms reduction” and “recovery from
addiction. “ Choices that might be good for the first goal can very well
be bad for the second goal.
Fourth Period:
1993-2002 (CONTINUED)
Until this time, buprenorphine was only a Schedule 5 drug (i.e. lowest
perceived danger). An interesting “contest” (i.e. – fight) between two
U.S. government agencies emerged. The DEA wanted it to put it on
Schedule 2, which would have effectively precluded any simple outpatient use. NIDA, however, was helping Reckitt Benckhiser lobby
Congress to allow physicians with extra-training to treat addicts at
regular outpatient office visits. The Drug Addiction Treatment Act of
2000 (DATA of 2000) allowed such trained physicians to apply for a DEA
exemption (that is the “x” on a DEA license number), buprenorphine
was placed on Schedule 3 around 2001, and in 2002 the FDA approved
the indication for opiate addiction treatment. The American Society of
Addiction Medicine (ASAM) began voicing strong approval of
buprenorphine for addiction-treatment beginning in 1998. ASAM was
entirely supportive of DATA of 2000, two years before buprenorphine
could be legally used by any physician outside the few approved
experimental-trial locations.
Fifth Period:
2002 - Present
Although buprenorphine has moved back into the market as an analgesic
(now for chronic pain) the strongest market, however, is for MAT. There has
been an explicit shift from a) use as a short-term (a few weeks) “step-down”
detox agent for physiological opiate dependence to b) use as a long-term (18
to 24 months; perhaps lifetime) for a mixed population of with addiction who
are mostly polysubstance-abusing addicts. An FDA advisory committee
recommended on January 12, 2016 that an implanted buprenorphine device
(6 month longevity per implant) be approved fully by the FDA for the purpose
of MAT 1. This form awaits final FDA approval. Veterinarians use the injectable
formulation for animal analgesia.
The literature -- both primary journal articles and policy statements for bestpractices – on MAT with buprenorphine tends to be unclear as to whether the
goal for MAT is eventual abstinence-based living for the individual patient or if
it is “harms reduction” for the population as a whole.
1Szabo,
Liz. “Panel recommends FDA approve implant to treat opiate addiction.“ USA Today. January 12, 2016.
http://www.usatoday.com/story/news/2016/01/12/implant-aims-help-addicts-stop-using-heroin-prescription-painkillers/78677618/
Accessed January 13, 2016.
Fifth Period:
2002 – Present - Continued
• Special training for prescribing physicians was created as an eight-hour
course.
• The DATA 2000 federal law restricted states from passing legislation that
forbade office practice on the basis of the opiate nature of the drug.
• The restricted case-load in any one physician’s practice was originally set
at 10 patients, was almost immediately increased to 30 patients in the first
year with 100 patients allowed after demonstrating a year’s experience.
Prescribers are now petitioning for the removal of all patient-load caps on
practice enrollment.
• Patients are usually seen once a month
• Payment for buprenorphine MAT was originally about $700 per month,
usually fee-for-service in cash. The cost now tends to be about $250 per
month. Some states have modified laws to require that prescribing
physicians accept insurance, and this requirement seems to pass muster
with the DATA 2000 federal law.
• Medicaid pays for much of the drug cost.
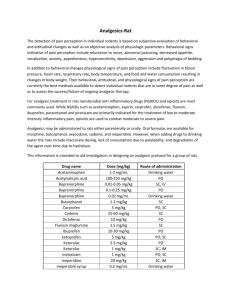
TOP 5 KY MEDICAID DRUG COST 2013:
Suboxone is 2nd at 17 million dollars
Script
Count
Member
Count
Quanty
Dispensed
Days
Supplied
Ranking by
Ranking by Member
Script Count Count
Ranking by
Total Spend
Drug Name
Total Spend
ABILIFY
$ 24,906,824.45
38737
6305
1163656.25
861954
1
85
139
SUBOXONE
$ 17,038,816.62
68863
6264
2317728
457642
2
46
140
METHYLPHENIDATE ER
$ 14,538,070.11
104687
17038
3376217
2236036
3
23
62
ADVAIR DISKUS
$ 13,124,576.01
50231
12661 3008171.635
991852
4
67
82
VYVANSE
$ 12,513,247.64
74453
11598
1380065
5
39
90
2213005
Part 2
Problems Observed In
the Research-and-Policy Literature
Regarding Buprenorphine MAT
Philosophies and Mental Health Science
Pure science, supposedly, is driven only by quantifiable data that is
interpreted as true information. The lens of interpretation, however, is
ground by philosophies, and philosophical theory harbors bias. We can
neither safely abandon the strengths of science nor ignore its weaknesses.
1) In the post-WW II years, researchers had immense trust in the ability of
science to correct human ailments with pharmaceutical agents. Advances in
medications to help treat everything from bacterial infections to depression
and psychotic disorders contributed to the optimism. But this burgeoning
optimism also led to the period of the 1960’s when dangers were minimized
or missed; a time, for example, when amphetamines and benzodiazepines
were freely distributed not only with little concern for addiction but even
with bold assertions that addiction was not possible.
2) In the post-WW II years, and especially by the 1960’s, psychology and
psychiatry in the U.S. were dominated by strict behaviorism’s learning
principles as discovered by B.F. Skinner. This psychology model has, as a
foundational premise, the notion that brains of similar intelligence will be
uniformly responsive to punishers and rewards in learning and unlearning
behaviors. It was not until Social Learning Theory (Albert Bandura in the early
1960’s) and Cognitive-Behavioral Theory (Aaron Beck in the later 1960’s and
early 1970’s) did a significant role for affect (i.e. – emotion) in learning arise.
Philosophies and Mental Health
Science- Continued
3) Campbell and Lovell, 2012, clearly describe a decadeslong tradition of very strong hopes among the U.S.
“Narcotics Farm” researchers that some opiate
antagonist would be the “Holy Grail” of addiction
treatment. This hope seems to be the only reasonable
explanation of Jasinski’s choice to classify buprenorphine
under the heading, “antagonist,” despite the clearly
established knowledge that the medication showed
morphine-like agonist action. We are not attributing
intentional misrepresentation as his motive, but we do
suspect that clear science was obscured by the
laboratory’s philosophical agenda that purported good
intentions.
Some Background on Discoveries
• Watson and Crick first described the mechanism of
inheritance, Deoxyribonucleic acid, or DNA, in 1953.
• Donald Goodwin published in a series of four articles1
in the early 1970’s the definitive proof from the
“natural laboratory” in Denmark using adoption
records that alcohol addiction is more strongly
predicted by manifestations in the biological than by
manifestations in the adoptive environment.
• The “Decade of the Brain” of the 1990’s used the newly
improved non-invasive, neuro-imaging techniques to
demonstrate distinct differences in living-brain function
for addicts versus non-addicts.2
1Summarized in
Goodwin, Donald. Is Alcoholism Hereditary? New York : Oxford University Press, 1976. Print.
a more recent article that will provide in the reference list a good guide to this advance in imaging to addiction, see
Goldstein, Rita Z and Nora D. Volkow. “Dysfunction of the Prefrontal Cortex in Addiction: Neuroimaging Findings and Clinical
Implications.” Nature. 12. November 2011. 652- 669. Print.
2For
Implications for the Buprenorphine
MAT Researchers
The major researchers for developing addiction-treatment
applications of buprenorphine were all educated at the
graduate study level before these advances had made much
of an impact on their notions about neuropharmacology of
addiction. A rough summary of the implications might be:
1) They tended to think, “All brains are basically the same,
and all brains train in the same way,”
2) They did not have the advantage of understanding the
impress of genetic load,
3) They had not absorbed the implications of the role that
affect (i.e. - emotion) plays in learning, and
4) They were of the generation of medical scientists who
were entranced by a wide array of proposed
pharmacological solutions.
BLUNT PROBLEM: Opiate Receptors “Burned”?
There is a notion that opiate addicts “burn out” their mu
receptors for the remainder of their life (i.e. – they will
always be deficient in ability for endogenous opioids and
encephalin substances to sooth the brain). This notion
has no credible foundation in any study we have found.
We are open to reviewing such if we can be pointed to
the sources. There are studies that show, for example,
that extensive methamphetamine-use permanently
truncates neuronal axons beyond repair,1 but the mureceptor “burnout” hypothesis does not seem to have
similar hard-data based on micrographs of post-mortem
neurons or based on fluorescent antibody studies.
1Gold
MS, Kobeissy FH, Wang KK, Merlo LJ, Bruijnzeel AW, Krasnova IN, Cadet JL. “Methamphetamine- and trauma-induced brain
injuries: comparative cellular and molecular neurobiological substrates.” Biological Psychiatry. 2009 Jul 15;66(2):118-27. PMID:
19345341
Blunt Problem: No Euphoria?
The buprenorphine literature continues to state that the drug causes little euphoria
because of the “ceiling effect” that occurs when the antagonist action trumps the
agonist action. The ceiling effect for buprenorphine alone (i.e. – when no sedativehypnotic drug like a benzodiazepine or alcohol is also present) is true for respiratory
suppression (brain-stem/ mid brain area). But this effect is not generalizable to all
parts of the brain; nor to polysubstance abusers.
THE PROBLEM is TWO FOLD:
• First, even the researchers know that naïve subjects can, and do, get high on
buprenorphine. It is true that an active heroin or Rx opiate addict will not get
much euphoria from buprenorphine, but a detoxed-addict or a first-time user will
and does get high. BUPRENORPHINE IS A DRUG OF REWARD.
• Second, IT IS A DRUG OF REWARD primarily because of the dopamine system, not
the nociceptive system. The major mu-receptor activity in the brain associated
with pain-control does not cause a “high.” Reduction of pain and induction of
euphoria are different phenomena. Opiate-receptors on interneurons in the
ventral tegmental area normally keep dopamine neurons from firing easily, but
when an opiate agonists settle on them, those interneurons stop inhibiting
dopamine release and a dopamine surge occurs. For 85% of the population, this
action may not be such a big concern because those people have a relatively
robust dopamine-reward system. They are “normals.” For persons who are
however predisposed to addiction genetically and, very possibly, epigenetically,
this action is serious. Introducing the predisposed addict’s pleasure-reward system
to any opiate agonist will likely trigger the phenomenon of craving.
Blunt Problem – Comparison Studies?
Articles that report on buprenorphine MAT tend only to compare it to other types of
MAT (clonidine, for example). The studies have not compared long-term use of
frequently-administered buprenorphine as MAT to long-term participation in
Abstinence-Based, peer-supported, frequently-attended programs such as 12 Step
Recovery. In fact, the presence of such “highly motivated subjects” as found in 12
Step Recovery would exclude them from a comparison-study because the MAT
comparison group would not be expected to show such motivation. The one study
which tried to compare buprenorphine-MAT to psychosocial therapies (i.e. variations of “talk therapy”) has been withdrawn from the field and the original
authors now concur that the study lacked sufficient data from which to draw any
conclusions.1 The studies most often measure success simply as “retention in
treatment” (i.e. – subjects show up for a longer period of time for some treatment).
The articles frequently generalize conclusions to populations not yet tested.
Examples:,1) results from MAT for Prescription opiate addicts is generalized to apply to
heroin addicts. 2) Results from studies about detoxification are generalized to longterm or life-time maintenance. 3) Results from opiate-only addicts are generalized to
polypharmacy addicts.
Mayet S, M Farrell, M Ferri, L Amato, M Davoli, “Psychosocial treatment for opiate abuse and dependence (Review).”The
Cochrane Library. 2004: 4. Reprint. 2010.
1
Blunt Problem – Harms Reduction vs.
Personal Recovery?
The confusion of the two different goals -- harms reduction and personal
recovery – in the research literature has bled into public policy pressures and
mandates.1 Harms reduction has as its main goal protection public interests
from addicts’ behaviors. Personal recovery has traditionally focused on an
individual finding a way to be abstinent from mind-altering drugs. The two
domains overlap, but they are not identical. As buprenorphine MAT advocates
amplify claims that this approach is evidence-based, three problems emerge.
1) There is no evidence comparing Buprenorphine MAT to Abstinence-Based
Recovery. Both approaches have believers, but neither side has controlledstudy evidence. NEITHER SIDE. 2) The Harms Reduction approach to social ills
has been quickly transformed into an Drug-substitution-Based Personal
Recovery, but this transformation has not paid attention to a real issue of
HARMS PROMOTION among a very vulnerable section of the population. This
vulnerable segment comprises the 8 to 15 % of the humans who are
predisposed to any-and-all addictions. These people are very likely 1) to have
predictive family histories and they are very likely 2) to exhibit polysubstance
abuse profiles. They do not usually get better on buprenorphine and they
often abuse buprenorphine (see study results below). They sometimes
transition from buprenorphine to heroin.2 - CONTINUED NEXT SLIDE
Blunt Problem – Harms Reduction vs.
Personal Recovery? - Continued
This vulnerable population -- many who have failed buprenorphine MAT in
the past – can find centers where, with sufficient motivation on their part and
with sufficient shielding from exposure to all drugs of reward on the part of
the center administrations, they can learn a design for living which allows
them to pursue abstinence-based personal recovery. Recent Public Policy
decisions and case-law findings increasingly attempt, however, to force such
abstinence-based-recovery centers to include in their case-loads participants
who choose buprenorphine MAT. If this trend gains power and force, it will
severely compromise the recovery-milieu of abstinence for those who choose
to pursue abstinence. A “clean” environment and a shared communal
experience is crucial for participants who are motivated to remain clearly
abstinent of all mind-altering substances.
1Vestal,
Christine. “In Drug Epidemic, Resistance to Medication Costs Lives.” Stateline: Pew Charitable Trust. January 11, 2016.
http://www.pewtrusts.org/en/research-and-analysis/blogs/stateline/2016/01/11/in-drug-epidemic-resistance-to-medication-costs-lives
Accessed January 13, 2016.
2Weiss,
Roger D., Jennifer Sharpe Potter, Margaret L. Griffin, Scott E. Provost, Garrett M. Fitzmaurice, Katherine A. McDermott, Emily N. Srisarajivakul,
Dorian R. Dodd, Jessica A. Dreifuss, , R. Kathryn McHugh, Kathleen M. Carro. “Long-term outcomes from the National Drug Abuse Treatment Clinical Trials
Network Prescription Opioid Addiction Treatment Study.” Drug and Alcohol Dependence 150 (2015). 112–119.
{PRESENTERS’ COMMENT: THIS STUDY IS PUBLISHED BY A TEAM WHERE THE LEAD RESEARCHER DISCLOSES FINANCIAL TIES TO RECKITT BENCKISER. EVEN
THOSE WHO STRONGLY SUPPORT THE WIDE USE OF BUPRENORPOHINE AS M.A.T. HAVE ACKNOWLEDGED THAT PRESCRIPTION OPIATE ADDICTS WITH NO
PREVIOUS HEROIN USE HISTORY HAVE ADVANCED TO HEROIN AFTER EXTENDED TREATMENT WITH BUPRENORPHINE.]
Blunt Problem – Is Ancillary
Counseling Support is Erratically
Advised and/ or Monitored?
Practice guidelines suggest that buprenorphine prescribers encourage
patients to engage in some form of non-medication psycho-social
therapy or peer-support. The buprenorphine MAT advocate industry
that has set those guidelines, however, 1) has not, determined by
random-assignment, controlled measurement studies which ancillary
therapy modality to encourage, 2) the prescribers have generally not
been held accountable for their patients’ failure to continue with such
ancillary treatment, and 3) the outcome-goal (e.g. - Eventual
buprenorphine MAT cessation with continued opiate abstinence?
Lifetime continuation of buprenorphine MAT with lifetime abstinence
from all other opiates? Eventual buprenorphine MAT cessation with
subsequent abstinence from alcohol and all drugs-of-reward?) are not
defined. (See study results below)
Blunt Problem – Is There Agreement on
Advice Given for Duration of
Buprenorphine MAT?
Practice varies from a 7 day, detox administration to a recommendation of
life-time maintenance. Consider Reckitts response to journalist:1
“Has RBP written a protocol for titration off of the medication SUBOXONE®
Film or SUBUTEX® (buprenorphine HCl) Sublingual Tablet? If not, why?”
"No. Reckitt Benckiser Pharmaceuticals Inc. believes there is no “one-sizefits-all” approach to opioid dependence treatment, and the company is not
aware of an established guideline or protocol for titration. The decision to
discontinue therapy with SUBOXONE® Film after a period of maintenance
should be made as part of a comprehensive treatment plan. Patients seeking
to discontinue treatment for opioid dependence should be advised to work
closely with their healthcare provider on a tapering schedule and should be
apprised of the potential to relapse to illicit drug use associated with
discontinuation of opioid agonist/partial agonist medication-assisted
treatment.“
1Roberts,
Dawn. “So You Thought You Could Get Off Suboxone?” The Fix: Addiction and Recovery,
Straight Up. September 04, 2014. https://www.thefix.com/content/hard-to-kick-suboxone?page=all .
Accessed January 13, 2016. Red font emphasis added by presenters.
Blunt Problem – Diversion Has
Increased
“2014 NFLIS Finds Nearly Three Times More Buprenorphine Than Methadone Reports
The National Forensic Laboratory Information System (NFLIS) collects drug test results
from law enforcement-encountered drug items submitted to and analyzed by state
and local forensic laboratories across the country. NFLIS data can provide valuable
information about trends in the drugs seized by U.S. law enforcement. In 2014, the
number of NFLIS reports for buprenorphine reached a high of 15,209, almost three
times the number of methadone reports (5,559). Buprenorphine reports increased
from 90 in 2003 (one year after buprenorphine was approved to treat opioid
dependence) to 15,209 in 2014. In contrast, methadone reached a peak of 10,016
reports in 2009, and has since decreased each year. In 2014, the Northeast had the
highest rate of buprenorphine reports (9.79 per 100,000 persons aged 15 or older),
while the West had the lowest rate (2.09 per 100,000 persons). More information
about buprenorphine can be found in the CESAR FAX Buprenorphine Series, available
online at http://go.umd.edu/cesarfaxbuprenorphine .“
CESAR FAX Volume 24, Issue 13, found at:
http://www.cesar.umd.edu/cesar/cesarfax.asp
Blunt Problem – Diversion Has
Increased
KENTUCKY MEDICAL EXAMINATION OFFICER’S
REPORT - 2014
Kentucky Resident Drug Overdose
Deaths by Drugs Involved (High
volume drugs)
300
250
200
150
100
50
0
ALPRAZOLAM
ETHANOL
HYDROCODONE
2011
2012
OXYCODONE
2013
2014
HEROIN
FENTANYL
Kentucky Resident Drug Overdose
Deaths by Drugs Involved (Lower
volume drugs)
60
50
40
30
20
10
0
BUPRENORPHINE
GABAPENTIN
2011
METHAMPHETAMINE
2012
2013
2014
THC
% Change Shown on KY MEO Toxicology Reports from 2013 to 2014
Fentanyl
Hydrocodone
Gabapentin
Buprenorphine
Heroin
Methamphetamine
Ethanol
Alprazolam
0.0%
100.0%
200.0%
300.0%
400.0%
500.0%
600.0%
Part 3
Clinical Anecdotes
Suggesting Problems
Which Need Future Research
Anecdotes CAN Lead to Data
Although the “plural of anecdote is not data,” a
deaf ear to anecdotes is most certainly a form of
“contempt prior to investigation.” Testable
hypotheses in medicine and mental health are
derived by careful attention to the signs and
symptoms of patients in the clinical settings, and
both treatment professionals and the patients in
addiction-recovery settings have been reporting
important things that deserve investigation.
“Is Dose Selection Supported?”
Criteria for choosing an induction-dose criteria
have never been well established by
randomized, controlled trials. This problem has
led to some patients, especially patients with
recent physiological addiction to prescription
opiates but with current remission from acute
withdrawal, to experience the induction dose as
the strongest “high” ever experienced in their
drug-use career. Avoiding iatrogenic euphoria
would seem to be an important goal.
“Is There An Increased Risk of
Depression?”
Some treatment center professionals have noted that
their participants who have been placed on
buprenorphine MAT seem to be more likely to exhibit
treatment-resistant major depression when compared to
the depressive episodes exhibited by recovering
participants not on this same MAT. The question of
possible iatrogenic depression requires investigation,
especially since an increasing trend has emerged to
suggest multiple-year to life-long adherence to MAT.
See also, Scherrer, Jeffrey F. Joanne Salas, Laurel A. Copeland, Eileen M. Stock, Brian K. Ahmedani, Mark D. Sullivan, Thomas Burroughs, F.
David Schneider, Kathleen K. Bucholz, and Patrick J. Lustman. “Prescription Opioid Duration, Dose, and Increased Risk of Depression in 3 Large
Patient Populations.” Ann Fam Med January/February 2016 14:54-62; doi:10.1370/afm.1885.
“CONCLUSIONS Opioid-related new onset of depression is associated with longer duration of use but not dose. Patients and practitioners
should be aware that opioid analgesic use of longer than 30 days imposes risk of new-onset depression. Opioid analgesic use, not just pain,
should be considered a potential source when patients report depressed mood.”
With each incremental increase (one month, two months, and three months duration), the risk on new-onset depression increased. This study
did NOT include any patients on buprenorphine (whether for pain treatment or for addiction treatment), but buprenorphine is an opioid
which originated as analgesic, has maintained that analgesic indication, has expand formulations for that analgesic application. This question
deserves to be answered so that patients who are considering the offer of many months or lifetime treatment can have a true informed
consent.
“Is Cessation of Buprenorphine More
Difficult Than Other Opiate Cessations?”
Anecdotes1 for participants in buprenorphine
MAT who decide to taper-off and then to quit
the extended maintenance report that the
withdrawal and cessation is more difficult than
even other MAT agents such as methadone. If
this is established by controlled research, proper
Informed Consent would need to be modified to
warn patients of this probability.
Roberts, Dawn. “So You Thought You Could Get Off Suboxone?” The Fix: Addiction and Recovery,
Straight Up. September 04, 2014. https://www.thefix.com/content/hard-to-kicksuboxone?page=all . Accessed January 13, 2016.
“When Should the Patient Plan to Stop
Buprenorphine MAT?”
As noted above, the research literature itself
does not give clear statements to this question.
Patient anecdotes suggest that prescriber
practices vary widely and wildly. Some patients
cannot even recall having been told by the
prescribers ANY target cessation goal.
“Possible Overdose Morbidity/Mortality
When Mixed with Sedative-Hypnotics?”
As shown in Section 3 above, states are including
buprenorphine (and the metabolite
norbuprenorphine) in toxicology screens and
reports. What is lacking so far is an analysis which
sorts out the overdose deaths which show when
buprenorphine is only present with any sedativehypnotic (e.g. – alcohol, benzodiazepines,
barbiturate)[ that is, when other well-known
mortality-associated opiates are absent.
“Extra Challenge Managing Overdose
in the ER?”
Emergency Department physicians already report that treating an
acute buprenorphine overdose by administering the reversal
(antagonist) agent naltrexone is difficult. Acute opiate overdose
treatment is initiated on history (if known) and clinical symptoms
(pupil size, respiration rates, etc.) and begins before lab results are
returned. Even then, common lab panels have not included
buprenorphine. In the first hour or two after naltrexone
administration, the patient’s signs improve, but these revert to the
poor levels of first presentation because buprenorphine molecules will
successfully compete against naltrexone to return to receptor-sites
before the liver detoxifies the plasma-levels of circulating drug.
Emergency Departments are busy places, and a suddenly (and
unexpectedly) “crash” of a previously stabilized patient is harrowing for
all concerned.
“What Social/Financial Burdens Are
Created by Diversion?”
Many participants in legally prescribed buprenorphine MAT report that
they procure their one-month supply from a pharmacy, they sell to
street-buyers a large portion (perhaps three-fourths) of the supply in
order to get money to purchase on the street opiates of preference
(diverted pain pills or heroin), hold back a portion (perhaps one-fourth
of the supply) for personal back-up use to stave of “drug sickness” in
the case that they cannot get a opiate of choice due to “dry spells” in
supply or lack of money.
This becomes a social financial burden because the purchase-price for
the legitimate prescription is often funded by others – sometimes
family members, but very often by Medicaid dollars.
When this occurs, Medication Assisted Treatment has become
Medication Facilitated Addiction, and the required capital for this form
of diversion is actually a diversion of dedicated health-care dollars. The
financial impact on public health care deserves study.
PART 4
Preliminary Report
on Descriptive1 Statistical Data
Gathered from The Healing Place,
Men’s and Women’s campuses,
Louisville, Kentucky.
1These
data are descriptive and not predictive according to standard use of those two terms
in inferential statistics. The subjects are drawn from a single cohort of a naturally-occurring
social setting. There is no random assignment to varied and controlled treatment
conditions. Having stated this fact clearly, we unapologetically hold the opinion that the
careful attention to these kinds of descriptions can help addiction-treatment professionals
and policy-developers understand more accurately the experience of these sorts of
subjects in this type of condition.
PARTICIPANT GENDER
120 Male
112 Female
TOTAL 232
PARTICIPANTS’ DRUGS OF
PREFERENCE
Subjects named three drugs in decreasing preference. The
drugs were coded in the classes of Heroin, Prescription
opiates, Alcohol, Benzodiazepines, Stimulants, Cannabis, and
Hallucinogens. Responses were searched to count the number
of times when either Heroin or Prescription Opiates occurred,
showing:
ZERO= 31% 1 time= 46% 2 times= 20% 3 times= 3%
(Background and Interpretation: Of the 232 subjects, about one-fourth were
almost exclusively alcohol users, or alcohol-and-non-opiate drug users. This
group did not have much opiate history or interest. Of the other subjects,
opiate-abuse was strong, but “opiate-only” users were extremely rare
(essentially only 3%). The opiate-addicts, therefore, in this setting are also
polysubstance abusing/ addicted.)
PARTICIPANT Self-Diagnosis
(N = 223, not 232 because
9 protocols failed to ask)
ADDICT:
48,
ALCOHOLIC:
66,
ADDICT AND ALCOHOLIC: 109,
NEITHER:
0,
or 22%
or 29%
or 49%
or 0%
History of buprenorphine use
(N = 232)
Had used buprenorphine
Had not used buprenorphine
146, or 63%
86, or 37%
Of Those Who Had Used
Buprenorphine (n = 146),
Those Who Used It ONLY WITH Prescription:
5, or 3.5%
Those Who Used It ONLY WITHOUT Prescription:
101, or 69%
Those Who Used It WITH AND WITHOUT Prescription:
40, or 27.5%
146 had used buprenorphine
(both circles combined)
101 only used
without Rx
(light blue
“C-shaped”
portion of
large circle)
146 had used
buprenorphine
(both circles
combined)
101
No
40
RX
=
141
Rx=45
45 had access by
Rx. (small circle).
Of them, 40 used
sometimes with
an Rx and
sometimes
without an Rx
5 (dark blue portion
of the small
circle). 5 of them
only used with an
Rx (light blue
“fingernail” of
small circle).
Intentional Euphoria-Seeking by
Use of Buprenorphine
Those who did so who only used without prescription
(n= 101):
77, or 76%
Those who did so who used both with and without
prescription (n= 40):
34 or 85.2%
Those Reporting Prescription-OnlyAccess to Buprenorphine (n=5) Who
Reported Taking Other Drugs or
Alcohol with Their Rx Buprenorphine
to Get a High
4, or 80%
Those Who Reported They Had Used
Buprenorphine to Get Through Rough
Days Until They Could Get Their
Preferred Drug of Choice
(“Bridge Use”)
Those who only used without prescription (n = 101):
79, or 78%
Those who used with and without prescription (n = 40):
34, or 85%
Ancillary Treatment-Advice from
Buprenorphine Prescribers to Those
Who Had Obtained by Prescription
(n=46)
Advised to attend AA/NA meetings:
29, or 63%
Advised to attend group or individual therapy:
28, or 61%
Suggested Duration and Reported
Duration of Buprenorphine MAT
In the first wave of subjects entered in the study (n =175)
the 34 subjects who had received prescription
buprenorphine MAT responded to this question as
follows: some do not recall having been told a time
frame for duration of treatment (n=16). There was one
report of a stated lifetime duration (i.e. - n=1). The 17
remaining subjects were told a range of 7 days or (n=1),
one month (n=2), 2 months (n=5), 3 months (n=2), 6
months (n=3), 9 months (n=1),12 months (n=2), 18
months (n= 2), and 24 months (n= 1).
In the second wave of enrollment, we asked subjects to
state how long they had stayed on buprenorphine. Seven
(7) subjects responded: “Does not remember” (n=1), 48
months (n=1), 24 months (n=1), 12 months (n= 2), 8
months (n=2).
Of Those Who Had Used
Buprenorphine (n = 146), Subjects
Who Report1 an Overdose When
Combining Buprenorphine with Other
Drugs or Alcohol
5, or 3.4%
1Note
well: whatever these experiences were for these few
subjects, they are the users who survived to report.
Diversion of Prescribed
Buprenorphine
In a third revision of the interview protocol,
subjects who reported ever having had received
buprenorphine by legal prescription (n = 11)
were asked if they had ever sold, traded, or
given away part of their prescription. Nine (n=
9), or 82%, answered “yes.” (One subject stated
bluntly that he only obtained prescribed
buprenorphine in order to sell it to others.)
SUMMARY POINTS
Is buprenorphine ever useful in addiction
treatment? Yes,
but only for
a) a very narrow range of patients
b) who are ONLY opiate-addicted
c) who do not show a significant family-history of
addiction
d) and only when used for a brief course of tapered
detoxification.
SUMMARY POINTS - Continued
Is buprenorphine an abused drug-of-reward? Yes.
Is buprenorphine often diverted? Yes.
Is buprenorphine addictive? Yes.
Is the withdrawal from buprenorphine easier to tolerate
than the withdrawal from methadone? No,
not if reports gathered in clinical interviews
are to be trusted.
Does a “ceiling-effect” protection against overdose-death
secondary to respiratory depression exist? Yes,
when ONLY buprenorphine is present. But safety
in this regard is not clearly established when
mixed with sedative-hypnotics. Nor is danger
in such cases established. Proceed with caution.
SUMMARY POINTS - Continued
Does the “ceiling effect” on respiration also
generalize to the prevention of euphoria? NO!
1) No research literature ever proves this assertion,
2) early research literature reports euphoria,
3) over 75-80% of the subjects from our addictionrecovery population report euphoria,
4) they report heightened euphoria by varying doses,
5) and they report mixing it with other substances to
enhance euphoria.
Are induction and maintenance dose choice well
established by research? No.
The Future for this Descriptive Study
The survey items which have yielded the pilot –
study information are now embedded in the
protocol used by the Center for Drug and Alcohol
Research, University of Kentucky, T.K. Logan, Ph.D.,
lead researcher. This center is tasked to collect data
continuously and regularly on participants at all
Healing Place locations in Kentucky (private, nonprofit) and at all Recovery Kentucky centers (a
division of the Commonwealth of Kentucky’s
Housing Authority). With this work, we hope to take
seriously the following famous statement:
"Facts do not cease to exist
because they are ignored."
-Aldous Huxley (1928)