Shawn K. Hatch, ACSW, LMSW, CCS, CAADC
Marquette General Health System
Maximum east-west distance – 320 miles
Maximum north-south distance – 125 miles
1700 miles of continuous shoreline with the
Great Lakes
4,300 inland lakes and 12,000 miles of
streams
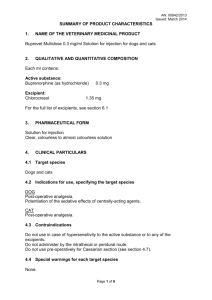
*U. S. Census Bureau: 2010 Population of UP Counties
2,156
36,628
6,780
8,860
67,077
16,427
7,028
9,601
11,817
8,485
26,168
24,029
37,069
11,113
38,520
Total population: 311,258
The UP holds 30% of the total land mass and
3% of the state population.
Three largest cities in the UP*
Marquette
Sault Ste. Marie
Escanaba
21,000 (Marquette County)
14,000 (Chippewa County)
12,000 (Delta County)
* 2010 U.S. Census
Morbidity and
Mortality
Healthy Behavior
Clinical Care
Social & Economic
Physical
Environment
The UP has a growing problem with opiate
and prescription drug abuse.
Alc. dep. or abuse in past year
Illicit drug dep or abuse in past year
Dep. on or abuse of any illicit drug
or alcohol in past year
National
Michigan
UP
7.53
2.82
9.07
7.79
2.88
9.41
8.05
3.07
10.00
Nonmedical use of pain relievers in past year among person aged 12 or older
National
Michigan
UP
5.00
5.63
5.29
MDCH, Mental Health & Substance Abuse Administration
Bureau of Substance Abuse & Addiction Services
State & Substate Estimates of Substance Use in Michigan
2006-2008 National Surveys on Drug Use and Health
Traditional outpatient and residential
treatment programs
Methadone . . . not available in the UP
Green Bay, WI – 175 miles
Muskegon, MI – 440 miles
Buprenorphine
4 physicians accepting new patients
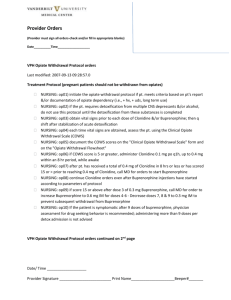
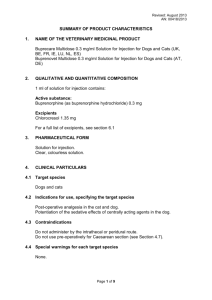
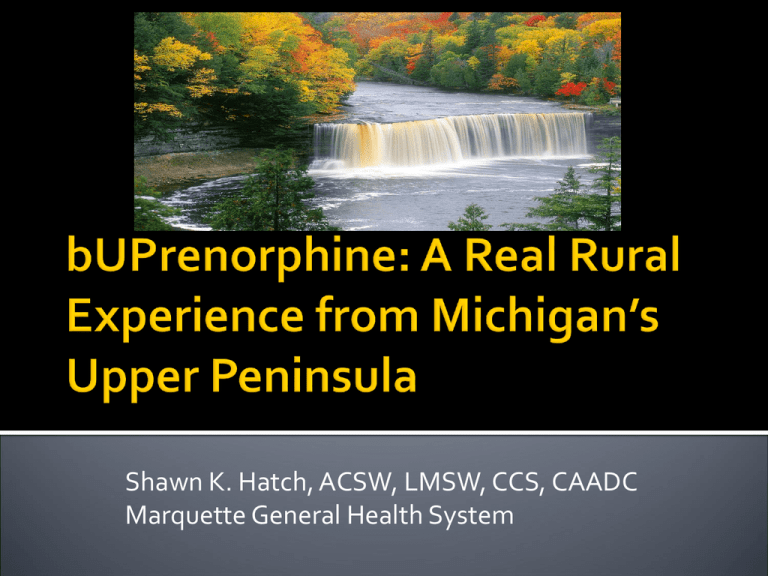
Medication approved for the OP treatment of
opiate dependence in 2000 (Drug Abuse
Treatment Act of 2000).
Set physician qualifications for prescribing.
FDA approved Suboxone/Subutex in 2002.
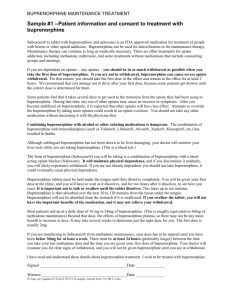
Partial Opioid Agonist
Ceiling effect
Withdrawal & Craving
Suboxone
8 mg buprenorphine/2 mg naloxone
Subutex
8 mg buprenorphine
▪ Primarily for pregnancy
Multiple reports of addicts snorting or using
IV.
Amount of naloxone may not be enough for
some individuals.
This is an abusable drug – like most, can be
used for good or evil.
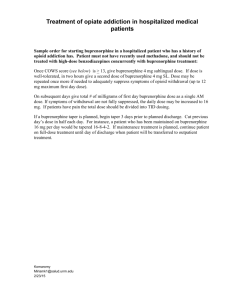
Prescribers must go through special training
and are issued a separate DEA number.
Prescribers are limited to 30 patients for the
first year.
Can apply for a waiver and treat up to 100 after
the first year.
Many prescribers want this population out of
their office . . . .
Prescribers still have limited knowledge of
addiction.
Yes
It isn’t the “drug of choice” but it is (significantly)
better than nothing
▪ The “high” experience
▪ Expectancy
▪ Relief from sick to not sick
Great to have on hand in case addict can’t score
▪ Selling/trading for full agonist
Methadone is currently the “standard of care”
for the pregnant opiate addict.
ACOG: Buprenorphine Versus Methadone
Treatment for Opiate Addiction in Pregnancy: An
Evaluation of Neonatal Outcomes, 2010
Lower NAS scores for the Subutex babies
▪ 10.69 versus 12.5
Shorter LOS
▪ 8.4 versus 15.7
Less than 50% of Subutex babies requiring treatment
versus 73% of methadone babies
2006
2007
2008
2009
2010
14
23
17
23
45
Yes . . . . and no
Making the leap
June of 2007 – MGHS accepts first patient
Brief phone screen
Quickly overwhelmed
Swamped with phone calls
High “hassle factor”
▪ Reports of “lost” or “stolen” meds
▪ Requests for early refills
▪ Refill requests . . . from jail
High volume of drop-outs and non-compliance
April of 2008 – Discontinued admissions
10 months and 29 patients
No denying how desperately this service was
needed.
At this point, only one other physician
prescribing in the UP.
We had a handful of patients who were doing
well for the first time in their lives.
This posed an interesting and challenging
question: How do we expand this
classification of patients?
Prescribing physician left our organization
Dr. John Lehtinen agrees to prescribe.
Road trip
How do we manage a limited resource?
How do we make this service available to the
best treatment candidates?
How do we manage the “hassle factor” and
prevent burning out our staff and physician?
How do we maintain our integrity and
credibility with local agencies, treatment
providers, law enforcement, and most
importantly, our patients?
Slowing down the process and looking for the
best matches for the medication.
Rationale for the application:
Completing and mailing the application would
require effort.
The application would allow us a better
opportunity to screen applicants and potentially
fill the limited treatment slots with those in the
best position to benefit from buprenorphine.
Items from criteria in TIP 40: Clinical
Guidelines for the Use of Buprenorphine in
the Treatment of Opioid Dependence:
History of treatment completion/compliance
Not currently abusing benzos, sedative-hypnotics,
or barbiturates
Not currently abusing alcohol
Supportive living environment
Supports for recovery
Dependence is limited to opiates
Employed
No medical contraindications
Indicated agreement to abide by rules and
expectations.
Already being treated with Suboxone and
successful
Active in substance abuse treatment
Treatment goal of abstinence
Has resources to pay for treatment and
medication
Not in collections with us
“Clean” MAPS
Application is complete
Buprenorphine screening questionnaire
MGHS Personal Data form
Releases of Information to the PCP and
current substance abuse professionals, as
applicable
Treatment contract*
Patient and family information about
buprenorphine
Summary of substance use
Program Requirements:
Attendance at all scheduled appointments
Attendance at a substance abuse program
ROI’s to all physicians and counselors/therapists
Abstinence from alcohol and drugs
Patient Responsibilities:
Store medication properly
Take as prescribed
Pill counts
Drug testing
Notify office if medication lost or stolen
Notify of relapse
Payment for services
Application is sent to caller.
Returned applications are “scored”
Review by Committee
Higher scoring applicants are contacted to
schedule appointment with physician and for
induction; assuming no medical
contraindications.
The score sheet – no magic number or total
score for automatic admission
Receive letter with specific treatment
recommendations and an invitation to meet
with addiction physician in consideration of
other treatment options.
Receive instructions regarding how to access
services for his/her circumstances, i.e., location,
treatment history, funding source, etc.
Encouraged to contact us for second review if
treatment recommendations are followed
through.
Prescribing Physician
Director of Clinical Services
Clinical Supervisor
Clinician
Provides forum to review program policy,
discuss clinical challenges, and advocate for
candidates.
Takes “heat” away from prescribing
physician.
Between August of 2009 and March of 2011
more than 350 applications were distributed.
Marquette 46%
Delta
19%
Dickinson 12%
Baraga
5%
Houghton 4%
Menominee 4%
Schoolcraft 3%
Iron
2%
Chippewa 1%
Ontonagon 1%
Gogebic
Luce
Mackinac
Alger
Wisconsin
Lower Pen.
n=2
n=1
n=1
n=2
n=2
n=1
50/50 split between males/females
Average distribution rate has been 18 per
month
Nearly half (170) of the 350 applications were
completed and returned to the Review
Committee
28% of those who have returned applications
have been admitted for buprenorphine
treatment.
Average age 29.8
Age:
17
18-30
31-40
41-50
51-65
Race
1%
61%
28%
8%
1%
91% Caucasian
9% Native American
Sex
Male
Female
46%
54%
June 2007 – April 2008 (10 months)
29 patients admitted
22 of original 29 were discharged
20 of the 22 were discharged by October of
2009, however, nearly half were gone within
the first 4 months of treatment
13 dropped out
7 discharged “at staff request”
2 completed
August 2009 – March 2011 (19 months)
48 patients admitted
7 discharges
5 dropped out
2 discharged “at staff request”
Retention rate went from 24% to 85%
Significant reduction in the “hassle factor”
Able to more than double admissions without
additional staff resources
Currently have 76 patients enrolled in the
program.
Pregnancy
The only exception to the application process
The application process would delay treatment
Acknowledgement that our focus has shifted to
treat the pregnant addict and provide the best
possible start for the baby.
▪ Limited window to engage the patient in treatment and
recovery.
Non-compliance with counseling
Late entry into pre-natal care and treatment
Shame
Use of other drugs/continued drug use
Poor support system
Poverty
Distance from physician (from all over UP)
“Hostage” until birth
Case coordination between OB/NICU and
prescribing physician
Pregnancy to access program.
High volume of pregnant addicts seeking
treatment with buprenorphine
43 since December of 2010; 40 pregnant at
admission
The return of the “hassle factor”
Incentive to comply
▪ About 25% compliance but improving.
Better outcomes from NICU
Shorter LOS and less severe withdrawal
How significant problem of opiate addiction
is in the UP
Buprenorphine isn’t for everyone
The application process is an effective way to
manage a valuable and limited treatment
resource
Support group didn’t fly.
How long should someone be on
buprenorphine? A controversial and
individualized question.
Counseling need to start before the
buprenorphine and the longer the better
We need to continually “take our own
inventory” regarding attitudes, beliefs,
biases, regarding buprenorphine treatment
and patients.
We still have much to learn . . . .
More challenging and stimulating opportunities
lie ahead . . . .
Shawn K. Hatch, ACSW, LMSW, CCS, CAADC
Director of Clinical Services, Behavioral Health
Marquette General Health System
Shawn.Hatch@mghs.org
(906) 225-3214