The Osteopathic Evaluation and Treatment of Acute Basketball
advertisement

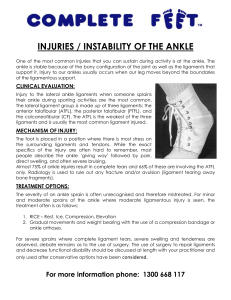
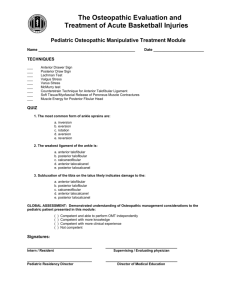
American College of Osteopathic Pediatricians Although basketball was not introduced during Dr AT Still’s tenure, OMT has a practical place in the evaluation, diagnosis and treatment of basketball injuries. The number of injuries seen in basketball has continued to rise over the years along with the number of participants. The most common injuries seen are strains and sprains of the ankle and knee followed by contusions. The ankle is the most commonly injured structure in basketball, followed by the knee. Ankle sprains are classified into grade I, II or III. X-rays should be attained according to the Ottawa ankle rules to rule out fractures. Most ankle injuries result from an inversion mechanism where the foot is plantar flexed and the sole of the foot is inverted medially. The foot is supported laterally by 3 ligaments and the peroneus muscle. The ligaments are relatively weak, and when the exerted force exceeds the strength of the supporting structures, tearing of the ligament fibers and muscle fibers occur. The anterior talofibular ligament is the weakest and most frequently injured structure. After an acute ankle sprain, the durability of the ligament can be assessed by the anterior drawer test. Subluxation of the tibia on the talus likely indicates damage to the anterior talofibular ligament. If excessive laxity of the ankle joint is noted, there is likely concomitant damage to one of the other ligaments as well; most likely the calcaneofibular ligament. Eversion injuries of the ankle are rare and when noted, associated avulsion fracture must be ruled out. There has been conflicting evidence regarding the overall incidence of injury between male and female athletes. However, there has been a significant disparity noted between the numbers of injuries to the anterior cruciate ligament seen in female basketball players when compared to male basketball players. This is thought to be multi-factorial, and includes neuromuscular, hormonal and structural differences between the sexes. All of the ligaments and both menisci in the knee can be assessed via different stress tests. The injured knee should always be compared to the contra lateral knee. If a soft end feel, or excess laxity of the joint is noted, there is likely damage to the ligaments. Radiographic examination is usually required after an acute knee injury. Initial radiographs can be obtained to rule out any avulsion fractures. Subsequent MRI imaging is usually required to diagnose ligamentous or meniscal damage. Due to the competitive nature of athletes, it is not surprising that here are a higher number of injuries that occur during competition relative to practice. Traditional therapy for sprained ankles/knees includes rest, ice, compression bandages, elevation and analgesics. The main focus of this therapy is to decrease the swelling and edema to help facilitate the return of full range of motion. There has been some evidence reported that OMT techniques can help reduce ankle edema, pain and increase the range of motion and ultimately lead to less time out of competition. Most knee ligament and meniscal injuries require surgical correction, but OMT can play an important role in the rehabilitation phase. How its performed 1: Patient is on their side with the affected leg up 2:Physician is seated beside the table 3: The tender point is located, typically anterior to the lateral malleolus 4: The ankle is everted until the tissues soften and the patient reports maximal relief at the tender point. 5: The position is held for 90 seconds and then the ankle is brought back to the neutral position and the tender point is reassessed. How 1: its performed Patient is in the supine position 2: The physician stands at the side of the involved leg 3: The physician inverts the foot to stretch the peroneus muscle and kneads the muscles to promote lymphatic flow 1: Patient is in the supine position 2: The physician stands on the side of the involved leg 3: The patients hips and knees are flexed to 90 degrees. 4: The physicians cephalad hand stabilizes the patient’s knee and holds the posterior fibular head between his thumb and index finger. 5: The physicians other hand everts and dorsiflexes the foot and internally rotates the lower leg 6: The patient then attempts to return his ankle/knee to the neutral position while the physician maintains isotonic resistance for 3-5 seconds. 7: The patient relaxes for 3-5 seconds and then the process is repeated until no new barriers are encontered and normal range of motion is restored. OMT evaluation consisting of observation, range of motion testing, and specific tests relative to each joint can adequately diagnose and assess the need for further intervention. The data suggests that OMT techniques focusing on relieving the swelling and increasing the range of motion of the joints in addition to the traditional therapy of rest, ice, compression wraps, and elevation leads to a faster recovery. Eisenhart et all performed a study that evaluated the efficacy of osteopathic manipulative treatment for patients with grade 1 and 2 acute ankle sprains. They used soft tissue, muscle energy, counterstrain, fascial and lymphatic drainage techniques. They found that after 1 session within the emergency department, patients had a statistically significant improvement in edema and pain and a trend toward increased range of motion when compared to the control group. At the 1 week follow-up appointment, both groups had an improvement in edema and pain, but there was a statistically significant improvement in the range of motion in the group that received OMT when compared to the control group. These specific modalities of soft tissue, muscle energy and HVLA are a worthwhile adjuvant treatment option that can help relieve tissue swelling and enhance the range of motion. If these techniques are done properly and in a timely manner, the data suggests that it can ultimately lead to less time lost from participation. In conclusion, the data suggests that the OMT module is easily performed within the time frame of an office visit or basketball game. Organ/System EENT Parasympathetic Sympathetic Ant. Chapman's Post. Chapman's T1-T4 T1-4, 2nd ICS Suboccipital Heart Cr Nerves (III, VII, IX, X) Vagus (CN X) T1-T4 T3 sp process Respiratory Vagus (CN X) T2-T7 T1-4 on L, T2-3 3rd & 4th ICS Esophagus Vagus (CN X) T2-T8 --- T3-5 sp process --- Foregut Vagus (CN X) T5-T9 (Greater Splanchnic) --- --- Stomach Vagus (CN X) T5-T9 (Greater Splanchnic) Liver Vagus (CN X) Gallbladder T6-7 on L T5-T9 (Greater Splanchnic) 5th-6th ICS on L Rib 5 on R Vagus (CN X) T5-T9 (Greater Splanchnic) Rib 6 on R T6 Spleen Vagus (CN X) T5-T9 (Greater Splanchnic) Rib 7 on L T7 Pancreas Vagus (CN X) Rib 7 on R T7 Midgut Vagus (CN X) T5-T9 (Greater Splanchnic), T9T12 (Lesser Splanchnic) Thoracic Splanchnics (Lesser) Small Intestine Vagus (CN X) T9-T11 (Lesser Splanchnic) Ribs 9-11 T8-10 Tip of 12th Rib T11-12 on R Appendix Hindgut Ascending Colon Transverse Colon T12 Pelvic Splanchnics (S24) Vagus (CN X) Vagus (CN X) Lumbar (Least) Splanchnics T9-T11 (Lesser Splanchnic) T5-6 --- --- --- --T10-11 T9-T11 (Lesser Splanchnic) R Femur @ hip Near Knees L Femur @ hip T12-L2 Descending Colon Pelvic Splanchnic (S2-4) Least Splanchnic Colon & Rectum Pelvic Splanchnics (S24) T8-L2 --- --- --- Question1: A, B, C, D, E. Question2: A, B, C, D, E. Question3: A, B, C, D, E. The most common form of ankle sprains are: a. inversion b. eversion c. rotation d. aversion e. reversion The weakest ligament of the ankle is: a. anterior talofibular b. posterior talofibular c. calcaneofibular d. anterior talocalcanel e. posterior talocalcanel Subluxation of the tibia on the talus likely indicates damage to the: a. anterior talofibular b. posterior talofibular c. calcaneofibular d. anterior talocalcanel e. posterior talocalcanel I, _________________________, successfully completed the Pediatric OMT Module on __ __ 20__ Signatures: Pediatric Resident ____________________ Pediatric Residency Director____________ ( Please print and give to program director.)