training_the_next_generation_of_clinician_scientists-
advertisement

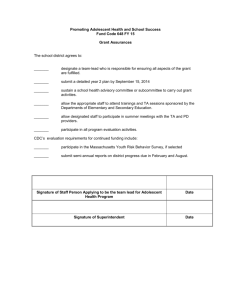
Improving Adolescent/Young Adult Health – Training the Next Generation of Clinician Scientists in Transdisciplinary Research S. Jean Emans, MD Professor of Pediatrics, HMS Director, Office of Faculty Development Chief, Division of Adolescent Medicine, Vice Chair for Clinical Affairs, Dept of Medicine Children’s Hospital Boston PI, Boston LEAH The Trajectory of Physician Scientists in Adolescent Medicine – a case example Nov 2008 – meeting hosted by WT Grant Foundation (Granger, Emans, Haggerty) Participants LEAH – S. Jean Emans, MD, Bryn Austin, ScD, Charles Irwin, MD, Richard Kreipe, MD, Donald Orr, MD MCH/HRSA - Laura Kavanagh, MPP; Trina Anglin MD, PhD NIH – Aria Crump, ScD, Robert Freeman, PhD, Lynne Haverkos, MD, Susan Newcomer PhD, Belinda Sims, PhD, David Stoff, PhD Foundations - Robert Granger, EdD, Lauren Hammer Breslow, Sally Klingenstein Martell, George Thibault, MD, John Van Gorder Other - Robert Haggerty, MD, Dale Garell, MD, Elizabeth Goodman, MD, Iris Litt, MD, Mark Schuster, MD, PhD, James Stockman, III, MD Adolescent/Young Adult Health Improving the health of youth requires high quality research by investigators across the disciplines of medicine, mental health, public health, nursing, education, sociology, epidemiology, and biostatistics Expert clinician educators, scholars, and investigators (MCH leaders) are needed to train health professionals in care delivery and quality improvement and create new knowledge and policy, including models of care. The Ideal Contribution of Adolescent Health Scientists Clinician scientists can ideally combine practical experiences in the delivery of mental and physical health services, a focus on the developmental trajectory of adolescents, and knowledge of the education and public health systems in formulating research questions Physician scientists, trained in transdisciplinary research, need to be able to bridge from the one-on-one patient encounter to collaborations with the investigators across disciplines The Challenge of Training Physician Scientists Adolescent Medicine fellowships are 3 yrs in pediatrics, 2 yrs in internal med, family practice 26 ACGME programs – Clinical and research training: curriculum with stats, research design, ethics, teaching, and for pediatrics a scholarship project under a Scholarship Oversight Committee – May include advanced degree MPH, MSc – May also receive credit for 2 years in RWJ program plus clinical experience Current Crisis in Number of New Adolescent Medicine (AM) Physician Scientists 20-28 physicians graduate each year from AM Fellowships; most clinician educators An informal survey of 6/7 MCH funded Leadership Education in Adolescent Health (LEAH) Programs for the trajectory of graduates past 5 years: 10/56 (18%) were spending more than 50% of time in research. A crisis for future research Facilitators: research environment (MCH support), mentoring, funding extending beyond fellowship, NIH Loan Repayment The Trajectory of the AM Physician Scientist Critical periods to spark interest and build competencies Additional research training and mentorship along the pathway Structured research time and feedback from national experts and peers; models from RWJCSP and WT Grant Scholars Funding – NIH, LRP, Foundations, Institutions Departmental research environment Pathway to Becoming an Independent Adolescent Medicine Physician Scientist NIH loan repayment can make research career viable. Typical Time in Training: 4 years 4+ years 3 years 3 years 1-3 years 3-5 years Additional research training, degrees, thesis. Clinical Training Undergraduate education Medical school Residency Fellowship Research Training Postdoc or first faculty position Mentored career development award Critical periods: Opportunities to spark interest, build competence in adolescent health research Projects in clinical and translational research, adolescent health Volunteer work in adolescent services Research opportunities Block research time Structured research mentorship, coursework, degree programs; T71 or T32, or RWJ Clinical Scholars departmental research environment Departmental coverage for 1-3 years for candidate to become viable for mentored career development awards; mentorship by investigators with external research funding Independent research scientist NIH and other federal funding, private foundation funding, or similar substantial career level award Challenges Short duration and variability of content and quality of research training; often little prior research experience Support for stipends – MCH T71 LEAH primary mechanism (broader goals); T32 funding unusual Lack of protected time in first two years of faculty position; mentoring may be inadequate; research environment may not have funded investigators Challenges New faculty may not be competitive for K’s, foundation young investigator programs Few unique funding mechanisms for those in adolescent medicine, unlike GI, cardiology, etc which often have society or foundation programs 85-90% of AM fellows are women - gender disparities in grant funding and academic outcomes Debt often high which may lead MDs to choose safer clinical trajectories What are some next steps? Develop ideal trajectories for medicine and other disciplines to create leaders who are clinician educators or investigators Propose the elements of the transformative transdisciplinary education that successful AM clinician scientists need for 2020 to be competitive for extramural funding (e.g. course work in other disciplines, collaborative projects, mentoring, critical feedback from senior investigators nationally). Recommendations for Adolescent Medicine Physician Scientists Transform medical student/residency education adding research content (courses, projects, MPH, PhD/MD, posters), summer stipends (eg SPR), mentorship, scholarships to meetings Broaden the research training of fellows with a research trajectory (course work, mentorship, environment); collaborate with programs such as RWJ CSP and Health Services Research Programs to develop a pipeline for some fellows to enter research intensive programs Recommendations Redesign the transition from fellow to faculty for those in transdisciplinary research: support, research environment, mentoring Partner with NIH, HRSA/MCH, CDC, foundations funders to create summer institutes on grantsmanship, enhance networking and research support (LRP, Ks, cross institute T32s, etc), target areas from NRC/IOM report on health services research (including models of care and “ehealth”). Recommendations Develop research forums and opportunities for mentoring, collaboration, and critical feedback from senior faculty, sponsored by MCH, NIH, CDC, or foundations, using model of WT Grant and RWJCSP. Educate IRBs about adolescent health issues and integrate into CTSAs. Address gender/minority trainee/faculty development to enhance academic success. Thanks To the WT Grant Foundation, Bob Granger, Bob Haggerty, and all the participants for defining new pathways to train the next generation of physician scientists. To the participants today and the IOM for continuing this important dialogue. Improving adolescent/young adult health in the U.S. and beyond will require the committed action of clinician educators and investigators across all the disciplines serving adolescents, and importantly adolescents and their families.