2 - National Child Traumatic Stress Network
NCTSN/NCPTSD
Psychological First Aid (PFA)
Overview presented by
Eric Vernberg, Ph.D.
University of Kansas and the
NCTSN Terrorism and Disaster Center
1
PSYCHOLOGICAL FIRST AID
Field Operations Guide
Sponsors:
• National Child Traumatic Stress Network
• National Center for PTSD
Principal Authors (alphabetical order)
Melissa Brymer, Anne Jacobs, Chris Layne, Robert Pynoos, Joseph
Ruzek, Alan Steinberg, Eric Vernberg, and Patricia Watson
Special consultants (alphabetical order)
Steve Berkowitz, Dora Black, Carrie Epstein, Julian Ford, Laura Gibson,
Robin Gurwitch, Jack Herrmann, Jessica Hamblen, Russell Jones,
Robert Macy, William Saltzman, Janine Shelby, Merritt Schreiber, Betty
Pfefferbaum, Rose Pfefferbaum, Margaret Samuels, Cynthia Whitham,
Bonita Wirth, and Bruce Young.
2
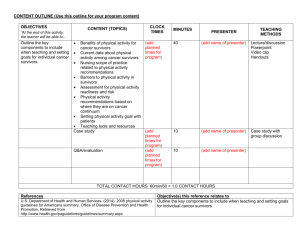
Basics of Psychological First Aid
• What: establish safety and security, connect to restorative resources, reduce stress-related reactions, and foster adaptive short- and long-term coping
• For: individuals experiencing acute stress reactions or who appear to be at risk for significant impairment in functioning
• By: mental health professionals and others who provide crisis assistance after catastrophic events
• When: Immediate and early phase post-event, in as little as 30 minutes and extended as needed
• Where: in a broad range of emergency settings, in either single or multiple sessions, adapted for use in group settings
3
• Principles and techniques of PFA meet four basic standards:
– (1) consistent with research evidence on risk and resilience following trauma
– (2) applicable and practical in field settings
– (3) appropriate to developmental level across the lifespan
– (4) culturally informed
PFA
4
• Evidence-Informed
• Modular format
• Information-gathering
• Concrete examples
• Developmental Framework
• Attention to Cultural Factors
• Handouts
Strengths of PFA
5
Basic Requirements for
Early Intervention Providers
• Capacity to connect with wide range of individuals
• Tolerance for symptomatic behavior and strong expression of affect
• Capacity for rapid assessment of survivors
• Ability to provide care tailored to timing of intervention, context, culture
• Recognition and response to emotional numbing processes
• Knowledge of self capacities
• Ability to provide clear, concrete information
• Ability to shift from conventional clinical practice
• Capacity for self-care
6
Expect normal recovery
Assume survivors are competent
Recognize survivor strengths
Promote resilience
Some Basics
7
PFA Core Actions
• Contact and engagement
• Safety and comfort
• Stabilization (if needed)
• Information gathering: current needs and concerns
• Practical assistance
• Connection with social supports
• Information on distress reactions and coping
• Linkage with collaborative services
8
Contact and Engagement
1: Establish a connection with affected persons in a nonintrusive, compassionate manner.
• Introduce self and describe role
• Ask for permission to talk
• Explain objective
• Ask about immediate needs
• Be informed about cultural norms related to personal contact
9
Safety and Comfort (1)
2:
Enhance immediate and ongoing safety, and provide physical and emotional comfort.
• Ensure immediate physical safety
• Provide information about disaster response activities/services
• Offer physical comforts
• Offer social comforts
• Attend to children who are separated from their parents/caregivers
• Protect from additional trauma and potential trauma reminders
10
Safety and Comfort (2)
• Help survivors who have a missing family member
• Help survivors when a family member or close friend has died
• Attend to grief and spiritual issues
• Provide information about casket and funeral issues
• Attend to issues related to traumatic grief
• Support survivors who receive death notification
• Support survivors involved In body identification
• Help caregivers confirm body identification to a child or adolescent
11
Stabilization (1)
3: Calm and orient emotionally-overwhelmed/distraught survivors.
• Stabilize emotionally overwhelmed survivors
• Talking points for emotionally overwhelmed survivors
• Role of medications in stabilization
12
Stabilization (2):
Signs a Survivor is Disoriented or Overwhelmed
• Looking glassy eyed and vacant
• Unresponsive to verbal questions or commands
• Disoriented
• Exhibiting strong emotional and physical responses
(uncontrollable crying, hyperventilating, rocking or regressive behavior, shaking, trembling)
• Exhibiting frantic searching behavior
• Feeling incapacitated by worry
• Engaging in risky activities
13
Stabilization (3)
If extremely agitated or losing touch with the surroundings:
• Ask them to listen to and look at you
• Speak softly and calmly
• Orient to surroundings
• Talk about aspect of the situation that is under their control, hopeful, or positive
14
Information Gathering: Current Needs and
Concerns (1)
4: Identify immediate needs and concerns, and gather additional information as appropriate to the situation.
• Form and maintain an alliance with the survivor
• Remain sensitive to survivor needs and perceptions
• Identify individuals in need of immediate referral
• Identify components of PFA that may be especially helpful
• Integrate survivor education with informal assessment
• Identify need for additional services or referral
15
Information Gathering: Content Areas (2)
• Nature and severity of experiences
• Death of a loved one
• Concerns about the immediate post-disaster circumstances and ongoing threat
• Separation from or concerns about the safety of loved ones
• Physical illness and need for medications
• Losses incurred as a result of the disaster
• Feelings of guilt or shame
• Thoughts about causing harm to self or others
• Developmental Impact
• Lack of adequate supportive social network
• Prior alcohol or drug use or psychiatric problems
• Prior exposure to trauma and loss
16
Practical Assistance
5: Offer practical assistance and information to address survivors ’ immediate needs and concerns.
• Identify the most immediate need(s)
• Clarify the need
• Discuss an action response
• Act to address the need
17
Connection with Social Supports
6: Connect survivors as soon as possible to social support providers, including family members, friends, and community helping resources.
• Enhance access to primary support persons (family and significant others)
• Encourage use of immediately-available support persons
• Discuss support-seeking
• Special considerations for children and adolescents
• Model supportive behavior
18
Information on Coping (1)
7: Provide the individual with information that may help them cope with the event and its aftermath, including information about:
• Provide basic information about common psychological reactions to traumatic experiences and losses
• Talk with children and body and emotional reactions
• Provide basic information on ways of coping
• Teach simple relaxation techniques
19
Information on Coping (2)
• Assist with developmental issues
• Assist with anger management Address highly negative emotions
• Address highly negative emotions (e.g., guilt, shame)
• Help with sleep problems
• Address alcohol and substance use
20
Linkage with Collaborative Services
8: Links survivors with needed services, and inform them about services that may be needed in the future.
• Provide direct links to additional needed services
• Promote continuity in helping relationships
21
Next Steps: Training
Develop strategic plan for dissemination and training
• NCTSN Terrorism and Disaster Network Committee
• Partnerships and adaptations
– Medical Reserve Corps (MRC)
– Spiritual care providers
– Health care settings
– Schools
– Community Emergency Response Teams (CERT)
• Standardized training packages
– Videos
– Skills training
– Integration with drills
– Online training version
22
Next Steps: Evaluation
Assessing effectiveness of PFA
• Does PFA facilitate decision-making
• Does PFA reduce immediate distress
• Does PFA help survivors avoid additional risk or risk-taking behavior?
• Does PFA help survivors connect to important services more quickly
Assessing impact of PFA training on providers
• Confidence, attitudes, knowledge
• Behavior in post-disaster settings
• Analog studies (e.g., behavior in training exercises)
23