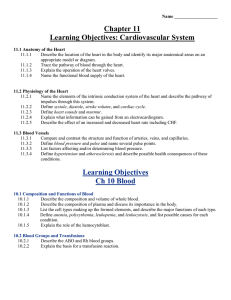
VITAL SIGNS

VITAL SIGNS
Vital Signs
Various factors that provide information about the basic body conditions of the patient.
4 Main VS
Temperature
Pulse
Respirations
Blood Pressure
Other Vital Signs
Pain
Scale - 0 to 10
Pts are asked to rate their level of pain on the 0 –
10 scale
Skin color
Size of the pupil & reaction to light
Level of consciousness
Patients response to stimuli
Pulse oximetry reading
Pulse
The pressure of the blood felt against the wall of an artery as the heart contracts and relaxes
Rate - # of beats per minute
Rhythm – refers to regularity
Volume – refers to strength
Pulse
Usually taken on the radial or carotid artery
Pulse is taken on an artery
Temporal – sides of the forehead
Carotid – sides of the neck
Brachial – inner aspect of forearm at the antecubital space
Radial – inner aspect of the wrist, above thumb
Femoral – inner aspect of the upper thigh
Popliteal – behind the knee
Dorsalis pedis – top of the foot arch
Pulse
Bradycardia – pulse <60 bpm
Tachycardia – pulse >100 bpm
(except in children)
Rhythm refers to the regularity of the pulse
(the spacing of the beats)
Regular
Irregular - arrhythmia
Usually caused by a defect in the electrical conduction pattern
Pulse
Volume – strength or intensity
Strong
Weak
Thready
Bounding
Factors that alter pulse rate
Increase pulse: exercise, stimulant drugs, excitement, fever, shock, nervous tension (stress)
Decrease pulse: sleep, depressant drugs, heart disease, coma, physical training
Respirations
The process of taking in O expelling CO
2 respiratory tract
2 and from the lungs and
1 breath consists of 1 inspiration and 1 expiration (exhalation)
Normal range:12–20 breaths/minute in adults
Respiration
Character – depth & quality
Deep
Shallow
Labored
Difficult
stertorous (abnormal sounds like snoring)
Moist
Regularity
Regular
Irregular
Respirations
Dyspnea – difficult or labored breathing
Apnea – absence of respirations
Tachypnea – RR >20 bpm
Bradypnea – RR <12 bpm
Orthopnea – severe dyspnea in which breathing is very difficult in any position other than sitting erect or standing
Respirations
Cheyne-Stokes Respirations – periods of dyspnea followed by periods of apnea; frequently noted in the dying pt
Rales – bubbling or noisy sounds caused by fluids or mucus in the air passages
Wheezing – dyspnea with high pitched whistling or sighing sounds during expiration; caused by narrowing bronchioles and/or obstruction or mucus accumulation in the bronchi
http://familymedicine.osu.edu/products/physicalexam/exam/
Respirations
Cyanosis – a dusky, bluish discoloration of the skin, lips, and/or nail beds as a result of ↓ O
2 bloodstream and ↑ CO
2 in the
RR should be counted in a way that the pt is unaware of the procedure
RR is partially voluntary controlled
Apical Pulse
Taken with a stethoscope at the apex of the heart
Use diaphragm (flat, flexible disk)
Actual heartbeat is heard & counted
Pulse Deficit – take the apical then the radial pulse, then subtract the radial from the apical = difference is the pulse deficit
Occurs with pts with heart conditions
Heart is weak & does not pump enough blood to produce a pulse
Temperature
A measurement of the balance between heat lost and heat produced
Heat is lost thru perspiration, respiration, & excretion (urine & feces)
Heat is produced by the metabolism of food; and by muscle and gland activity
Temperature
Homeostasis – constant state of fluid balance
The rates of chemical reactions in the body are regulated by body temp.
If body temp is too high or too low the body’s fluid balance is affected
Temperature
Measured:
Oral
Rectal
Axillary
Aural (ear)
O
R
Ax
T
aka tympanic; in auditory canal
A low or high reading can indicate disease
Temperature
Normal range 96.6 to 100.6 F depending on route used
Individuals have different body temps
Depends on the body’s processes
Time of day
Lower in am, after resting
Higher in pm or after activity or food intake
Parts of the body vary
O-98.6 R-99.6 Ax-97.6
Temperature
Factors that lead to ↑ body temp
Illness, infection, exercise, excitement, environmental temp
Factors that lead to ↓ body temp
Starvation/fasting, sleep, ↓ muscle activity, sleeping, mouth breathing, environmental temp, certain diseases
Temperature
Hypothermia – body temp <95 o F rectally
Death usually occurs if temp <93 o F rectally
Hyperthermia – body temp >104 o F rectally
Prolonged exposure will cause brain damage or serious infection
>106 o F will lead to convulsions, brain damage, or death
Temperature
Fever – elevated body temp >101 o F rectally
Pyrexia
Febrile – fever is present
Afebrile - no fever is present, WNL (within normal limits)
Clinical Thermometer
Glass with mercury or alcohol w/red dye
If breaks, mercury can evaporate & create toxic vapor, attacking CNS
Never vacuum or sweep to clean – use a mercury spill kit
Red – rectal
Blue – oral or axillary
Temperature
Factors that can alter temp in mouth
Eating, drinking (hot or cold), smoking
Wait at least 15 min before taking temp
Clean thermometers in disinfectant solution
Blood Pressure
BP – measurement of the pressure that the blood exerts on the walls of the arteries during the various stages of heart activity (contraction and relaxation)
BP is read in mm of Hg (mercury)
Sphygmomanometer is the medical name
Blood Pressure
Systolic BP
Pressure occurs in the walls of the arteries when the left ventricle of the heart is contracting and pushing blood into the arteries
Normal range 100 to 120 mm Hg
Blood Pressure
Diastolic BP
The constant pressure in the walls of the arteries when the left ventricle of the heart is at rest, or between contractions.
Blood has moved forward into the capillaries and veins, so the volume of blood in the arteries has decreased.
Normal range 60 – 80 mm Hg
http://familymedicine.osu.edu/products/ physicalexam/exam/
Blood Pressure
Pulse Pressure
The difference between Systolic BP and
Diastolic BP
Important indicator of the health and tone of the arterial walls
Normal range 30 – 50 mm Hg
120/80 120 – 80 = 40 pulse pressure
Blood Pressure
Hypertension (HTN) – High BP; 140/90 or higher
Causes: stress, anxiety, obesity, high
Na intake, aging, kidney disease, thyroid deficiency, vascular conditions
(arteriosclerosis)
HTN not treated will lead to kidney failure, stroke, heart disease
Blood Pressure
Prehypertension- BP in the range of
120/80 - 139/89
Don’t have “high blood pressure” but at risk for developing HTN if lifestyle changes do not occur.
Blood Pressure
Hypotension – low BP; less than 90/60
May occur with heart failure, dehydration, depression, severe burns, hemorrhage, and shock
Orthostatic or Postural Hypotension
Sudden drop in both SBP & DBP when a person changes positions
Caused by the inability of blood vessels to compensate quickly to positional change
SS ; lightheaded, dizziness, blurred vision
Blood Pressure
Factors that ↑ BP
Excitement, anxiety, nervous tension
Stimulant drugs
Exercise & eating
Smoking
Factors that ↓ BP
Rest or sleep
Depressant drugs
Shock
Excessive loss of blood
Fasting (starvation)
PRACTICE BLOOD PRESSURE
As a class practice reading the computerized blood pressures
http://familymedicine.osu.edu/products/ph ysicalexam/exam/
After each reach reading discuss if BP is in normal range or not