IV Acetaminophen Research Proposal - Beth Ellen Kalkman
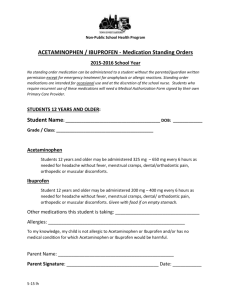
advertisement

Running head: CHAPTER 1 1 IV acetaminophen Research Proposal Chapter 1 Cathy Bozek, Karen Collins, Beth Kalkman, Lori Van Zoeren, and Joel Vedders Ferris State University Running head: CHAPTER 2 2 Research Proposal Introduction The side effects of opioids and their use in postoperative patients are well documented. These side effects include sedation, nausea, vomiting, respiratory depression, and constipation (Memis, Inal, Kavalci, Sezer, & Sut, 2010). Pain control in the elderly hip fracture population (defined as adults sixty-five years and older) often requires the use of opioids to assist in postoperative pain control. Administration of opioids can lead to the unwanted side effects previously listed. However, under-treatment of pain in this population can also have detrimental effects on the patient's recovery. “Cognitively intact patients with undertreated pain were nine times more likely to develop delirium than patients whose pain was adequately treated" (Morrison et al., 2003, p. 80). Patient outcomes can also be affected when pain is under-treated. These include increased length of hospital stay, missed or shortened therapy sessions, decreased likelihood of ambulating by the third postoperative day, and decreased ambulation scores six months after surgery (Morrison et al., 2003). The goal is to strike a balance between minimizing opioid side effects and maximizing patient outcomes. A multimodal approach to pain control has been shown to be effective in the reduction of opioid consumption (Morrison et al., 2003). This method often adds the use of non-opioid medications as an adjunct with the goal of reducing the amount of opioids needed for optimal pain control. A non-opioid that has been recently approved for use in the United States is intravenous (IV) acetaminophen. Several studies have been performed using IV acetaminophen showing favorable results in its effectiveness in reducing the amount of opioids used postoperatively. Limited data is available specifically related to its use in the elderly hip fracture population and comparison studies between IV and oral acetaminophen administration. On the basis of this limited data it is therefore necessary to CHAPTER 2 3 verify our hypothesis comparing the efficacy of IV acetaminophen versus oral administration in the elderly hip fracture population for optimal pain control and reduced consumption of opioids. As nurse educators utilizing evidence-based practice and research is essential in providing quality care. It is imperative that we understand the rationale for providing multimodal pain management for the elderly hip fracture population. Therefore research that furthers our understanding of pain management will enhance not only practice at the beside but broadens our knowledge of pain management as a whole. Abbreviated Literature Review IV acetaminophen was approved for use in the United States by the Food and Drug Administration (FDA) in 2010 (Smith, 2011). The initial use was limited to acute pain and fever in pediatric and adult populations (Marcario and Royal, 2010). Prior to FDA approval, a prospective randomized study performed in Sweden by Pettersson, Jakobsson, and Owall (2005) examined the opioid sparing effect of IV paracetamol (acetaminophen) administration compared to that of oral acetaminophen administration in coronary bypass patients. According to their findings, opioid sparing was somewhat improved in the IV administered group, but not significantly so, and adverse effects (nausea and vomiting) were similar in both study groups during the post-operative period. The same year, in a multi-center, double-blinded, placebocontrolled, repeated-dose, 3 parallel-group study, Yale researchers demonstrated the safety and efficacy of IV acetaminophen in comparison to propacetamol (a precursor to paracetamol available in Europe for over 20 years) for pain management in orthopedic patients (Sinatra et al., 2005). A double-blind randomized controlled trial presented in New Zealand in 2009 by Brett, Barnett, and Pearson (2012), verified a more rapid achievement of elevated plasma levels of CHAPTER 2 4 acetaminophen through intravenous administration when compared to the oral route in postoperative patients. The rapid onset of higher plasma levels, they hypothesized, insured quicker onset of a therapeutic range of acetaminophen and therefore, decreased the need for rescue analgesia during the early recovery period for IV recipients. Although statistically significant differences were not demonstrated between oral and IV routes, a trend towards a reduced need for rescue analgesia in the IV route was confirmed in knee arthroscopy patients (Brett, Barnett, & Pearson, 2012). Memis, Inal, Kavalci, Sezer, and Sut (2010) studied the efficacy of IV acetaminophen in reducing opioid use, decreasing opioid related adverse effects, and decreasing time to extubation for post-operative patients in the intensive care unit. In this Turkish study, initially presented as a poster presentation in 2009 at the European Society of Intensive Care Medicine Congress, IV acetaminophen was used as a complement to Demerol administration for the management of post-operative pain. Results of the study confirmed improved pain control, decreased Demerol usage, and reduced nausea, vomiting, and sedation through the combined therapy of IV acetaminophen and Demerol. A literature review was presented by Marcario and Royal (2010) providing a summary of studies conducted worldwide related to the analgesic effects of IV acetaminophen. The study included information related to propacetamol a precursor to the current, paracetamol formulation in comparison to placebo or active comparator. Their description of 16 studies completed in 9 countries, supports IV acetaminophen as an effective postoperative analgesic. As part of the New Drug Application (NDA), Sinatra, et. al (2011) validated the findings of their 2005 study providing more quantifiable data. This data included: CHAPTER 2 5 pain intensity differences over 24 hours using currently accepted imputation methods . . ., efficacy after the first 6 hours, effects of gender, race/ethnicity, age, weight, surgical site, American Society of Anesthesiologist (ASA) class, and serotonin antagonists; and a stepwise regression analysis of why adverse event of nausea and vomiting were numerically (although not statistically) higher in the IV acetaminophen group compared with placebo (p. 357). Findings of this study confirmed the researchers' earlier results verifying IV acetaminophen as a safe and effective analgesic agent. Most recently, Jahr, Breitmeyer, Pan, Royal, and Ang (2012) presented data from three randomized trials on the efficacy and safety of IV acetaminophen use in the elderly orthopedic post-surgical patients. Using subjects meeting inclusion criteria for their purposes, the researchers extracted information from existing studies on IV acetaminophen to discuss its use in light of the unique complications and co-morbidities of this population when experiencing hip or knee replacement. The author's findings promote IV acetaminophen as a desirable alternative to, or compliment of, opioid pain relief. Problem/Purpose Statement Many studies have been performed using IV acetaminophen in a multimodal approach to pain post-operatively. Until recently, however, little data was available about IV acetaminophen use in the elderly hip fracture population. Jahr et al. (2012) compared the efficacy and safety of IV acetaminophen in the elderly following orthopedic surgery. Nevertheless, there is limited information regarding the appropriate length of time IV acetaminophen should be used or the effectiveness of IV versus oral administration of acetaminophen in controlling pain. CHAPTER 2 6 As the aging population increases, the incidence of hip fracture will also increase. According to Chang, Center, Nguyen, and Eisman (2004), the incidence of hip fracture is predicted to be 2.6 million by 2025 and reach 4.6 million by 2050. In 2006 the Center for Disease Control (CDC) reported that of the 900,000 discharges from short stay hospitals, 566,000 were the result of fractures in those age 65 or older (Jahr, Breitmeyer, Pan, Royal, & Ang, 2012). Hip fractures are one of the most costly fractures that nurses see in practice (Chang, et al., 2004). Failure to provide adequate pain control, while minimizing side effects related to opioid use, will result in increased healthcare costs related to lengthened hospital stays. It is therefore essential that this population receives optimal and efficient care. This is particularly important to nursing practice as awareness and education is needed related to all the potential complications that elderly hip fracture patients face, especially pain. A potential solution to providing adequate pain relief in this population may lie in a multimodal approach using IV acetaminophen in conjunction with opioids. The knowledge gap that exists with regard to the use of IV acetaminophen in the hip fracture population, as well as gaps in efficacy over time comparing IV and oral administration demonstrates the need to pursue this information. Considering the expected explosion in elderly hip fractures over the coming years, this information will be very useful as we strive for optimal outcomes for this population. Therefore based on this preliminary examination of IV acetaminophen and the needs of elderly hip fracture patients, this group hypothesized: Elderly hip fracture patients (ages 65 and older) who receive IV acetaminophen for 48 hours postoperatively use less rescue opioids than those who receive scheduled oral acetaminophen for 48 hours following surgery. This purpose statement may yield vital information to fill gaps in current available research. CHAPTER 2 7 Theoretical Framework The relationship between theory and research is reciprocal (Polit & Beck, 2012). Nursing theories provide structure and offer a systematic approach to research (Cody, 2013). A theoretical framework can be utilized by both quantitative and qualitative research. In the assessment of any proposed research, basic questions need to be asked of the study’s chosen framework. These questions include: Is the theory clear, too simple or too complex, grounded in reality, appropriate, and important (Polit & Beck, 2012). Additional questions to be asked are, has the theory been utilized with prior research, and is the theory credible (Polit & Beck, 2012). A theory gains credibility through evidence which lends support to a theory’s previously accepted tenet (or conversely, weakened by evidence to the contrary). It is important to ensure a “fit” between the theory chosen and the research. As the research problem states, in the growing elderly population there is an increased incidence of hip fractures requiring surgical repair (Chang, Center, Nguyen, and Eisman, 2004). Maintaining adequate postoperative pain control for these patients can be difficult. The elderly often have other co morbidities and are affected differently than younger adults with the use of opioids. Appropriate postoperative pain management is essential to the positive outcome of the elderly surgical patient. The authors have chosen to conduct research to determine if IV acetaminophen is more effective than oral acetaminophen in the elderly postsurgical hip fracture patient, specifically to reduce the side effects caused by opioid use. Several theories regarding pain exist. Many theoretical frameworks were considered to guide this research proposal. Lenz and Pugh’s (1997) theory of unpleasant symptoms was one theory considered. This theory explains the catalytic behavior between two or more symptoms occurring at the same time, thus making the patient’s perception of each symptom more intense. CHAPTER 2 8 Another theory considered was Auvil-Novak’s (1997) middle-range theory of chronotherapeutic intervention for postsurgical pain. This theory explores the concept of circadian rhythm pain. Since the authors are trying to support the use of IV acetaminophen in striking a balance between analgesia and side effects, Good’s theory Pain: A balance between analgesia and side effects theory was chosen. This theory contains three propositions which are multimodal intervention, attentive care, and patient participation. Good’s (2009) theory makes five assumptions which include: providers will interact with nursing to manage acute pain opioid analgesic are indicated medication is given for side effects as needed patients have set goals, have the ability to learn, and can communicate symptoms Nurses have knowledge of pain management. Assessment of the Model Theoretical clarity: Good’s theory clearly defines outcomes and propositional statements. Theoretical and operational definitions are listed. Basic assumptions are consistent with one another. Theoretical complexity: This theory is comprised of three outcomes; 1) Balance between analgesia and side effects, 2) Pain, and 3) Side effects. Proposition one encompasses potent pain medication (opioid) use, and a pharmacologic adjunctive (IV acetaminophen), and non-pharmacologic interventions (nursing therapies-i.e. early ambulation, coughing, and deep breathing). Proposition two discusses the regular assessment of pain and side effects (giving regular scheduled doses of IV acetaminophen for 48 hours postoperatively), identification of pain relief (numeric scale), and reassessment and/or further nursing interventions. Proposition CHAPTER 2 9 three is concerned with patient education and goal setting that is mutually agreed upon by the patient and the healthcare team. Theoretical grounding: When discussing theoretical grounding, Polit and Beck (2012) ask the question “are the concepts identifiable in reality” (p.138). Good’s (2009) Pain theory is easily identified in studies. Two studies were offered in the research. Appropriateness of the theory: The theory is fairly narrow so researchers can utilize minimal randomization control trials (RCTs) in the adult population suffering from postoperative hip surgery pain. Importance: The goal of this theory was to provide a more holistic approach to pain management. Utilization of multimodal entities allows for decreased opioid use. General issues: A limitation of this theory is that it does not express the treatment of pain in the elderly population. Nursing models and theories represent ideal, logical, unique perspectives or “maps” of the person and health (Cody, p. 339). The following three questions will help the nurse identify the most appropriate model. Does the theory or model address the client’s problems and health concerns? Are the nursing interventions suggested by the model consistent with the client’s expectations for nursing care? Are the goals of nursing actions, based on the model or theory, congruent with the client’s desired health outcomes (Cody, p. 345)? A concept map is attached as an appendix. This map is a visual representation of the proposed research within this theoretical framework. It is the assumption of this group that IV CHAPTER 2 10 acetaminophen use in the elderly post operative hip fracture patients will elicit decreased opioid use and side effects compared to oral acetaminophen use. Research Questions Research questions seek to address a research problem, and also the strength and direction of the variables as they relate to each other (Polit & Beck, 2012). When considering a research question for a proposed project it is important to think in terms of variables. Determining the exact variables of focus will clarify the researchable questions (Polit & Beck, 2012). Utilizing evidenced-based practice and research ensures nurses provide optimal care to this patient population. With the projected rise in the elderly hip fracture population it is imperative that nurses will be actively involved in research which will improve patient outcomes. The use of IV acetaminophen as an analgesic, with fewer side effects than other analgesics, provides the safest option for pain management (Vadivelu, Mitra, and Narayan, 2010). This study is well suited to produce quantitative data. Quantitative research questions produce information that can be measured. There are three levels of research questions that must be considered. A level one statement is used when you have limited research on a issue or topic. A level 2 purpose statement addresses what you will observe, but are unable to predict what you will find (Wood & Ross-Kerr, 2011). A level III purpose statement is written as a hypothesis or also known as a predictive hypothesis where you assume a relationship between your variables (Wood & Ross-Kerr, 2011). Due to what is currently known regarding IV acetaminophen Level III research questions several possibilities were generated. The research question that our group chose to examine in more detail is as follows: CHAPTER 2 11 Do elderly hip fracture patients who receive 1 gm IV acetaminophen every 6 hours for 48 hours post operatively require less rescue opioids and experience less opioid induced side effects than those who receive 1 gm of oral acetaminophen every 6 hours for 48 hours. For this proposed research project we will be manipulating the independent variable which is the route of acetaminophen (IV or oral) administration to determine the effect on the dependent variable of opioid consumption. If the hypothesis is supported by this research proposal, and acetaminophen does reduce the use of opioids, this will also decrease the incidence of opioid induced side effects. Ultimately this will result in improved care that is supported through evidenced-based research. Conclusion In summary, the authors hope this research proposal provides substantial evidence to support a research project to establish the superior efficacy of IV acetaminophen when compared to oral acetaminophen. Furthermore, a positive correlation between the use of regularly scheduled IV acetaminophen in the elderly, post-surgical hip fracture patient and the reduction of opioid use will be demonstrated. By reducing opioid use, unpleasant postoperative side effects will be diminished. Hip fracture can be a debilitating condition for the elderly patient due to pain and immobilization. Complications from hip fractures can include delirium, functional loss, and increased length of hospital stay. It is imperative that nurses partake in research which will improve patient outcomes. In Chapter 2, further developments will occur regarding Marion Good’s Pain: A balance between analgesia and side effects theory. Included will be criticisms and rationale for the selection of this theory. In addition, a more comprehensive literature review of the major CHAPTER 2 concepts supporting the use of IV acetaminophen in the elderly post-surgical hip fracture population will be included. 12 CHAPTER 2 13 References Auvil-Novak, S. E. (1997). A middle-range theory of chronotherapeutic intervention for postsurgical pain. Nursing Research, 46(2), 66-71. doi: 10.1097/00006199-19970300000002 Brett, C. N., Barnett, S. G., & Pearson, J. (2012). Postoperative plasma paracetamol levels following oral or intravenous paracetamol administration: A double-blind randomised controlled trial. Anaesthesia Intensive Care, 40(1), 166-171. Chang, K. P., Center, J. R., Nguyen, T. V., & Eisman, J. A. (2004). Incidence of hip and other osteoporotic fractures in elderly men and women: Dubbo Osteoporosis Epidemiology Study. Journal of Bone & Mineral Research, 19, 532-536. doi: 10.1359/JBMR.040109 Cody, W. K. (5th ed.) (2013). Philosophical and Theoretical perspectives for Advanced Practice Nursing. Charlotte, NC: Jones & Bartlett Learning. Good, M. (2009). Pain: A balance between analgesia and side effects. In S. J. Peterson, & T. S. Bredow (Eds.), Middle Range Theories: Application to Nursing Research (2 ed., Ch. 3). Philadelphia, PA: Lippincott Williams & Wilkins. Jahr, J. S., Breitmeyer, J. B., Pan, C., Royal, M. A., & Ang, R. Y. (2012). Safety and efficacy of intravenous acetaminophen in the elderly after major orthopedic surgery: subset data analysis from 3, randomized, placebo-controlled trials. American Journal of Therapeutics, 19(2), 66-75. doi: 10.1097/MJT.0b013e3182456810 Macario, A., & Royal, M. A. (2010). A literature review of randomized clinical trials of intravenous acetaminophen (paracetamol) for acute postoperative pain. Pain Practice, 11(3), 290-296. doi: 10.1111/j.1533-2500.2010.00426.x CHAPTER 2 14 Memis, D., Inal, M. T., Kavalci, G., Sezer, A., & Sut, N. (2010). Intravenous paracetamol reduced the use of opioids, extubation time, and opioid-related adverse effects after major surgery in intensive care unit. Journal of Critical Care, 25, 458-462. doi: 10.1016/j.jcrc.2009.12.012 Morrison, R. S., Magaziner, J., Gilbert, M., Koval, K. J., McLaughlin, M. A., Orosz, G., ... Siu, A. L. (2003). Relationship between pain and opioid analgesics on the development of delirium following hip fracture. Journal of Gerontology Series A: Biological Sciences and Medical Sciences, 58(1), M76-M81. doi: 10.1093/Gerona/58.1.M76 Morrison, R. S., Magaziner, J., McLaughlin, M. A., Orosz, G., Silberzweig, S. B., Koval, K. J., & Siu, A. L. (2003). The impact of post-operative pain on outcomes following hip fracture. Pain,103(3), 303-311. doi: 10.1016/S0304-3959(02)00458-X Lenz, E. R., Pugh, L. C., Milligan, R. A., Gift, A., & Suppe, F. (1997). The middle-range theory of unpleasant symptoms: An update. Advances in Nursing Science, 19(3), 14-27. Pettersson, P. H., Jakobsson, J., & Owall, A. (2005, June). Intravenous acetaminophen reduced the use of opioids compared with oral administration after coronary artery bypass grafting. Journal of Cardiothoracic and Vascular Anesthesia, 19(3), 306-309. doi: 10.1053/j.jvca.2005.03.006 Polit, D. F., & Tatano Beck, C. (2012). Nursing research: Generating and assessing evidence for nursing practice (9th ed.). Philadelphia, PA: Lippincott, Williams & Wilkins. Sinatra, R. S., Jahr, J. S., Reynolds, L. W., Viscusi, E. R., Groudine, S. B., & PayenChampenois, C. (2005). Efficacy and safety of single and repeated administration of 1 gram intravenous acetaminophen injection (paracetamol) for pain management after major orthopedic surgery. Anesthesiology, 102(4), 822-831. CHAPTER 2 15 doi: 10.1097/00000542-200504000-00019 Sinatra, R. S., Jahr, J. S., Reynolds, L., Groudine, S. B., Royal, M., Breitmeyer, J. B., & Viscusi, E. R. (2011). Intravenous acetaminophen for pain after major orthopedic surgery: An expanded analysis. Pain Practice, 12(5), 357-365. doi: 10.1111/j.15332500.2011.00514.x Smith, H. S. (2011). Perioperative intravenous acetaminophen and nsaids. Pain Medicine, 12, 961-981. doi: 10.1111/j.1526-4637.2011.01141.x Vadivelu, N., Mitra, S., & Narayan, D. (2010). Recent advances in postoperative pain management. The Yale Journal of Biology and Medicine, 83(1), 11. Wood, M. J., & Ross-Kerr, J. C. (2011). Basic steps in planning nursing research (7th ed.). Sudbury, MA: Jones and Bartlett Publishers. CHAPTER 2 16 Appendix CHAPTER 2 17 IV Acetaminophen Research Proposal Chapter 2 Cathy Bozek, Karen Collins, Beth Kalkman, Lori Van Zoeren, and Joel Vedders Ferris State University Running head: CHAPTER 3 18 IV Acetaminophen Research Proposal Chapter 2 The purpose of this chapter is to further explore the major concepts of our proposal and provide support for the theoretical framework in which it is constructed. Information related to IV acetaminophen, the unique characteristics of the elderly, and the experience and needs of elderly patients undergoing surgery will all be discussed. Furthermore, we will discuss considerations related to opioid use in the elderly population. We will examine several studies that have applied our chosen theory, Good and Moore's (1996) pain: a balance between analgesia and side effects (BASE) as their foundational structure. The theory's flexibility and adaptability in a variety of research demonstrates its use being an excellent choice for our study's theoretical framework. Theoretical Foundations The chosen framework for this proposal is Good and Moore's (1996) theory pain: BASE. As suggested by the theory's title, Good and Moore sought to provide optimal pain relief while minimizing the negative side effects of pain management modalities. Understanding the background to the theory will assist in establishing its credibility for use. The Agency for Health Care Policy and Research (AHCPR) published recommendations in 1992 that guide adequate pain management in postoperative patients (Good, 1998). The recommendations stress the importance of educating patients on how to communicate levels of pain and how to assess if pain is not adequately relieved after receiving medication. While these guidelines became the gold standard for clinical practice in postoperative pain management at that time, Good and Moore found that these guidelines were not in a form to be tested (Good, 1998). The guidelines needed a theory to assist in "concepts and propositions at an intermediate CHAPTER 3 19 level of abstraction" (Good, 1998, p. 120). Their theory was then formulated from the AHCPR guidelines. Good and Moore's resultant theory, pain: BASE stresses the importance of patient teaching with an emphasis on the nurse’s responsibility, as well as the patients themselves, to assess and reassess pain. Pharmacologic treatments, along with the effectiveness and side effects of the treatments, are also evaluated. Good and Moore (1996) discuss the importance of nurses having access to descriptive theories which guide practice related to pain management. Propositions of this theory were discussed in Chapter 1 which predicts outcomes related to postoperative pain management. The two main concepts that Good (1998) discussed were: (a) the balance between analgesia and side effects, and (b) decreased pain and side effects (p. 122). Concepts that are more specific can then be researched by delving into the elements of pain versus the effects of sequelae such as nausea and vomiting. Good (1998) stressed the importance of a multimodal delivery of care to decrease pain. Involved in this method of care are: (a) a comparison of medications and how the medications are delivered; (b) the use of a pharmacological adjuvant in comparison to not using an adjuvant; and (c) the use of non-pharmacologic adjuvants, such as cold therapy, music, imagery, and massage. These measures all assist the researcher in developing a proposal that answers the hypothesis in question. Several articles utilize BASE, and the relationship between their theory and our proposed research will be demonstrated. Study One Good and Moore’s theory of pain alleviation is the underlying framework for a study done by Benson, McMillan, and Ong (2012). Their study focused on how potent pain medication (bupivacaine spinal with intrathecal morphine), along with other opioids and non- CHAPTER 3 20 pharmacologic adjuvants (i.e. warming blankets), can promote a balance between analgesia and side effects. The aim of this prospective, randomized controlled study was to determine the efficacy of a patient-controlled, forced-air warming gown in optimizing a patient’s perioperative body temperature and in decreasing postoperative pain after a total knee arthroplasty (TKA). Limitations of the study were listed as: (a) lack of standardization of administration of anesthetic, (b) the study was not a blinded study, (c) temperature variations were not monitored in the operating rooms, (d) a specific gown temperature was not tested, and (e) the temperature of the warming cupboard was not monitored and may have resulted in variable blanket temperatures. Findings of the study demonstrated that opioid consumption was decreased in those patients who were warmed with a warming gown (Benson, McMillian, & Ong, 2012). Study Two A retrospective study of two hundred fifty-seven charts, conducted by Otten and Dunn (2011), used BASE to promote a multimodal system for postoperative pain control following TKA. The prescriptive theory BASE was utilized as foundation of this study because: (a) the population of interest is alert adults, (b) pain is usually severe after TKA, (c) multimodal therapeutics are needed, and (d) side effects of pain medication administration are troublesome (Otten & Dunn, 2011). Patients who received “all 3 anesthetic modalities (intrathecal morphine sulfate, single-shot femoral nerve block, and wound catheter) had better pain control postoperative TKA” (Otten & Dunn, 2011, p. 373) and requested less rescue opioids. Study Three A third study utilizing Good and Moore’s theory is a “descriptive profile of pain in 80 women during the first two days after gynecologic surgery” (Good et al., 2000, p. 96). Pain was scored before and during ambulation on both day one and day two after surgery. Sleep was also CHAPTER 3 21 addressed, as pain can often be a cause of nighttime sleep disturbances (Good et al., 2000). The recovery of gastrointestinal function was also addressed. It was found that post-surgical nurses should help patients set realistic goals for pain control after gynecologic surgery, provide adequate analgesic medications, assess and reassess the patients for pain, and provide nonpharmacological adjuvants (relaxation or soft music tapes). All of these, in conjunction with one another, produce less postoperative complications (Good et al., 2000). A reported limitation of this study was the fact that sleep medications were not accounted for. In addition, the instrument used to address the patient’s sleep had “no known reliability or validity” (Good et al., 2000, p. 102). Study Four Blanchard and Murnaghan (2010) used BASE to lend support to their single case study of a nursing student's experience of working with a multimodal approach to pain management in a patient with acute chest pain in the emergency room. They stress the correlation of BASE to the Prince Edward Island conceptual model. A collaborative, systematic approach to pain is evident with assessment and reassessment. The article clearly illustrates the use of multimodal interventions with: (a) patient teaching and goal setting, (b) attentive care with assessment of pain and interventions, and (c) pharmacological and non-pharmacologic treatments (Blanchard & Murnaghan, 2010). Study Five Voshall, Dunn, and Shelestak (2012) conducted a study “to examine nursing faculty’s knowledge of pain management” (p. 2). BASE was the theoretical framework for this descriptive correlational study as well as King’s theory of goal attainment. Both theories emphasize patient teaching with mutual goal setting, regular assessment of pain, possible CHAPTER 3 22 pharmacologic modalities, evaluation of side effects if medication is used, and the assessment of interventions (Voshall et al., 2012). Voshall et al. (2012) addressed the relationship of nursing faculty’s age, educational level, pain management preparation and length of time as a practicing nurse. Additionally, the length of time as an instructor, length of time teaching pain management in the classroom, and additional continuing education in pain management were studied. Results of the study indicated that nursing curriculum “may need to be strengthened in the topic of pain management” (Voshall et al., 2012, p. 10). Based on these five articles, we are in support of the use of Good and Moore’s theory, BASE. Multimodal approaches to pain management should be in place for the safety of our patients, thus decreasing potentially debilitating side effects. BASE addresses multimodal therapy (IV acetaminophen and opioid use), attentive care (regularly scheduled doses of IV acetaminophen, and assessment and reassessment of pain and side effects), and patient participation (with patient teaching regarding medication and pain management). Literature Review of Major Concepts Elderly Population Considerations The elderly population is rapidly growing within the United States (U.S.). This is attributed to not only the aging baby boomers, but also to advances in health care and illness prevention that are making it possible for humans to live longer. By 2030, there is expected to be 71.5 million people over the age of 65 within our country (Bruckenthal, 2010). The elderly will constitute 20% of the nation's entire population (Kim & Geitsfeld, 2008). Although the American Nurses Association (ANA) has published specific standards of practice for gerontological nursing, schools of nursing may not adequately prepare student nurses to provide CHAPTER 3 23 care in the specialty area of geriatrics (Corbett, 2011). As this aging and vulnerable segment of the population grows, it is imperative that nurses gain a better understanding regarding the unique characteristics related to aging and the pain management needs of this group. Physiological changes of aging. Normal aging involves the slow deterioration of multiple body systems (Chodko-Zajko et al., 2009). The resultant physiological changes include: decreased muscle mass with accompanying reduced strength and flexibility, decreased cardiovascular function with reduced blood volumes and increased blood pressure at rest, an initial increase in weight with slow decline after age 70, and a decline in bone density (ChodkoZajko et al., 2009). Together, these factors can contribute to an increased risk of fall and injury. “Regular exercise can minimize the physiological effects of an otherwise sedentary lifestyle and increase active life expectancy by limiting the development and progression of chronic disease and disabling conditions" (Chodko-Zajko et al., 2009, p. 1510). Since only 50-60% of patients return home to their independent life after sustaining a hip fracture (Koren-Hakim et al., 2012), the ultimate goal for nursing should be returning the elderly patient to physical activity as soon as possible following an injury such as a fractured hip. Pain experience. Some causes of pain in the elderly are irreversible (Bruckenthal, 2010). McCleane (2010) echoes this sentiment stating "we are not at the position where we could realistically claim that pain is an entirely treatable symptom or that pharmacological modalities available for such treatment are devoid of significant side effects" (p. 183). In the elderly person there can be a loss of serotonin and norepinephrine receptors that assist in the suppression of pain (McCleane, 2010). Also, neurological changes in the aging body include loss of myelination in the fibers of the peripheral nervous system. These neuropathies may cause significant chronic pain. The existence of chronic pain in some elderly patients has led to CHAPTER 3 24 misdiagnosis and mistreatment related to the source of pain (Brown, Kirkpatrick, Swanson, & McKenzie, 2011; McCleane, 2010). Care providers may wrongly attribute a person's pain to one of the common chronic conditions of aging instead of looking for an acute source. It is important to safeguard one's self against stereotyping elderly patients experiencing pain. McCleane (2010) reports the results of a number of studies have shown elderly persons to have an increased threshold for pain. Meaning, elderly patients report the experience of pain at more extreme measures than younger people; that is, it takes more pain to feel pain. However, elderly people are less tolerant of experiencing pain. Whereas a younger individual may be exposed to pain and accept it with a sense that it is temporary, elderly individuals may fear that the pain, once experienced, will not cease (McCleane, 2010). The elderly person's tolerance for pain or ability to cope with pain may be directly associated to his or her psychological, biological, and social health (Bruckenthal, 2010). According to Kim and Geistfeld (2008), "social isolation commonly occurs among older adults as a consequence of poor health, retirement, and the loss of a spouse and friends" (p. 3). Reciprocally, the experience of pain may further cause social isolation (Brown, Kirkpatrick, Swanson, & McKenzie, 2011). Postoperative pain management in the elderly is often complicated by the frequent incidence of poly-pharmacy in the population (Bruckenthal, 2010). Many elderly persons are taking a number of medications for chronic conditions. The risk of side effects and interactions between medications make appropriate prescribing difficult. "Both inappropriate prescribing and medication underuse are common in the elderly, as is the under treatment of pain in this patient population" (Bruckenthal, 2010, p. S23). Therefore, it is important to partner with the elderly patient to determine strategies to successfully manage his or her pain. CHAPTER 3 25 Surgical Considerations in the Elderly/Opioid side-effects According to the Centers for Disease Control and Prevention (CDC, 2012) in 2007, 281,000 hospital admissions were related to hip fracture patients who were 65 years and older. Hip fractures within the geriatric population may result in a major disability with an overall reduced quality of life. Our goal is to positively impact the key outcomes of surgery for this population and aid in returning the individual to the highest level of self-care and quality of life. Ambulation. Post-surgical early ambulation within the elderly hip fracture population is a necessity to achieve long-term and short-term goals. According to a review of clinical practice guidelines for the management of proximal femoral fractures, early assisted ambulation accelerated functional recovery and is connected with an increase in direct discharges home (Mak, Cameron, & March, 2010). With optimal pain relief, early ambulation can be achieved (Olsson, Karlsson, & Ekman, 2007). Early ambulation is necessary to prevent pulmonary complications, thromboembolism, and pressure ulcers, which are all a frequent complication after surgical hip repair (Roth, Kammerlander, Luger, & Blauth, 2010). Nutrition. Nutritional status is another issue to consider when caring for an elderly hip fracture patient. According to Koren-Hakim et al. (2012), up to 58% of patients with a hip fracture have been found to be malnourished. This can be caused by a number of issues; first, nutritional deficits can result from aging and poor cognitive status (Koren-Hakim et al., 2012). Additionally, preoperative fasting, surgical delays, pain, nausea, and vomiting can contribute to malnutrition for the elderly while in the hospital (Koren-Hakim et al., 2012). A retrospective study was performed which included 215 elderly hip fracture patients who were surgically repaired between the years 2007-2009. Ninety-five patients were well-nourished, ninety-five were at risk for malnutrition, and twenty-five were malnourished (Koren-Hakim et al., CHAPTER 3 26 2012). Fewer hospital readmissions occurred in the well-nourished group (36%) compared to the high risk and malnourished groups (64%) (Koren-Hakim et al., 2012). Mortality rates were also lower at thirty-six months within the well-nourished group (22%) compared to the at-risk group (40%), and the malnourished group (50%) (Koren-Hakim et al., 2012). The results of this study show the importance of elevating nutritional status in the elderly hip fracture population and the positive effects it can have on the outcomes. Mak, Cameron, and March (2010) promote utilization of protein and energy supplements in this population to support an adequate nutritional status. Postoperative cognitive dysfunction. Elderly patients who have undergone surgery often suffer from postoperative cognitive dysfunction (POCD) (Halaszynski, 2009). Halaszynski (2009) reports a potential cause of POCD is a decrease in the stress response during opioid consumption, which can then lead to postoperative delirium. Sleep impairment can also result in decreased postoperative function levels, fatigue, and POCD (Halaszynski, 2009). Postoperative delirium increases length of hospital stays and is associated with poor long-term outcomes (Marik, 2010). Opioid Use in the Elderly Due to the changing physiology associated with aging, the elderly experience negative side effects of opioids related to absorption and metabolism of the drugs themselves. The possible side effects range from nausea, constipation, urinary retention, central nervous system adverse effects, pruritus, respiratory depression, and opioid-induced hyperalgesia (Chau, Walker, Pai, & Cho, 2008). A reduction in muscle mass and an increase in body fat can increase the amount of drugs available in the system for a longer period of time that can increase the opioid’s side effects (Huang & Mallet, 2012). Reduced hepatic function due to aging can reduce the CHAPTER 3 27 hepatic clearance of the drug by 30-40% (Huang & Mallet, 2012). A decline in renal function must also be considered as metabolites that are not excreted completely can accumulate (Huang & Mallet, 2012). The use of opioids also increases the risk of falls. According to Huang and Mallet (2012), the use of codeine puts the patient at a 127% greater risk of falls. Opioids also increase the risk of drug-to-drug interactions that create an increased risk of falls. A goal of healthcare providers should include limiting side effects of opiates while still properly controlling pain for their patients (Chau, Walker, Pai, & Cho, 2008). Utilizing other pain therapies (i.e. IV acetaminophen) along with decreasing the use of opioids will yield superior outcomes for the elderly. IV Acetaminophen Given the rising costs of health care in the U.S., hospitals are seeking new ways to minimize pain in postoperative populations in order to reduce length of stays. The use of multimodal medication therapies is on the rise. White (2005) studied the use of multimodal medication therapies and the changing role that IV acetaminophen and other non-opioid analgesics can provide. White (2005) wrote that IV acetaminophen is probably the safest and most cost effective of all the non-opioid options on the market at the time of publication. In addition, IV acetaminophen decreased morphine use in postoperative patients by 22 % to 46 % in patients who had major orthopedic surgery (White, 2005). History of IV acetaminophen. IV paracetamol, also referred to as IV acetaminophen for the purposes of this paper, has been available in Europe since 2001 (Jones, 2011). However, it was not approved for use in the U.S. until November of 2010 (Smith, 2011). Prior to its approval in the U.S., IV acetaminophen was available for use in sixty other countries, involved CHAPTER 3 28 in sixty-nine clinical trials, and more than 400 million doses were administered (Barkin, 2011). IV acetaminophen was established as a safe and effective drug that could be used as part of a multimodal treatment regimen for postoperative pain. IV acetaminophen has been available in another form known as propacetamol. Propacetamol was never approved for use in the U.S. and although previously used in Europe, it is currently being phased out in favor of paracetamol (Pergolizzi, Raffa, Tallarida, Taylor, & Labhsetwar, 2011). Propacetamol is a prodrug of IV acetaminophen and is a diethylglycidyl ester of acetaminophen; once it is administered intravenously it is converted to acetaminophen within seven minutes (McNicol et al., 2011). A meta-analysis was performed by McNicol et al. (2011) which reviewed thirty-six studies to compare the effectiveness and safety of IV acetaminophen verses propacetamol. A total of 712 patients received IV acetaminophen, 1431 were treated with propacetamol, and 1048 received a placebo (McNicol et al., 2011). Combined data from nine studies which compared each form of drug to a placebo showed a 50% reduction in pain over six hours in 26% of those who received propacetamol, and 27% in those receiving IV acetaminophen (McNicol et al., 2011). These results translated in to a 30% reduction in opioid use (McNicol et al., 2011). Thirteen of the studies also reported no statistical difference in nineteen different adverse events reported when compared to placebo (McNicol et al., 2011). One significant difference reported between IV acetaminophen and propacetamol was injection site pain during administration (McNicol et al., 2011). Of those who received propacetamol, 23% reported pain at the injection site compared to just 2% in those receiving IV acetaminophen (McNicol et al., 2011). An additional advantage of IV acetaminophen over propacetamol is that propacetamol needs to be reconstituted prior to administration, while IV acetaminophen is ready to use in its CHAPTER 3 29 current solution state (McNicol et al., 2011). Contact dermatitis has also been reported by health care workers who handle propacetamol during its reconstitution (McNicol et al., 2011). The meta-analysis conducted by McNicol et al. (2011), concluded that IV acetaminophen and propacetamol yielded similar results related to safety and effectiveness in controlling pain. IV acetaminophen held an advantage because it did not need reconstitution and had a low incidence of pain upon infusion (McNicol et al., 2011). This may also be one reason propacetamol is not available in the U.S. Advantages of IV acetaminophen. IV acetaminophen is advantageous for the postoperative or orthopedic patient due to its relatively low side effects rate. In the elderly, this is important, as opioids may be associated with respiratory depression, hypotension, dizziness, confusion, and delirium (Lachiewicz, 2013). Lachiewicz (2013) suggests that multimodal pain protocols should be considered for all perioperative orthopedic patients. IV acetaminophen has a rapid onset; “the median time to reach maximum plasma concentration (Tmax) . . . is 15 minutes” (Lachiewicz, 2013, p. 16). The Tmax for oral acetaminophen is 45 to 75 minutes, and the Tmax of rectal administration is 3 to 4 hours (Lachiewicz, 2013). The half life of IV acetaminophen is 3.2 hours (Lachiewicz, 2013). Gaps in the Literature Our comprehensive literature review yielded information related to the major concepts of our proposed study. However, remaining gaps were identified. Although it is clear that improved pain management facilitates early ambulation, no literature was located related to IV acetaminophen's use in improving functional outcomes. These include: early ambulation, decreasing the well-known side effects of opioids, increasing compliance with physical therapy, and promoting early discharge home for the elderly patient. Furthermore, there was no evidence CHAPTER 3 30 of research utilizing BASE in our chosen population of the elderly postoperative hip fracture patient. Two articles reflected on TKA, one article on chest pain, one article on gynecologic surgical pain, and one on nursing faculty’s knowledge of pain. Conclusion As health care costs continue to rise in the U.S., hospitals are seeking ways to control postoperative pain, and thus shorten the length of stay. Multimodal therapy has been proven to be effective in this endeavor. The use of IV acetaminophen in the elderly postoperative hip fracture population has been shown to significantly decrease postoperative pain, along with the adverse side effects of opioid use, as the elderly metabolize opioids in a different manner than do their younger counterparts. However, the use of IV acetaminophen and its effect on functional outcomes has not been documented. Chapter Three will focus on the design and methodology for our research proposal. We will discuss the research design, how to choose the population sample and collect data, as well as a focus on the validity and reliability of this research. Additionally, we will consider ethical considerations and discuss limitations of the project. CHAPTER 3 31 References Benson, E. E., McMillian, D. E., & Ong, B. (2012). The effects of active warming on patient temperature and pain after total knee arthroplasty. American Journal of Nursing, 112(5), 26-33. doi:10.1097/01.NAJ.0000414315.41460.bf Blanchard, J. F., & Murnaghan, D. A. (2010). Nursing patients with acute chest pain: Practice guided by the Prince Edward Island conceptual model for nursing. Nurse Education in Practice, 10(1), 48-51. doi:10.1016/j.nepr.2009.03.010 Brown, S. T., Kirkpatrick, M. K., Swanson, M. S., & McKenzie, L. (2011). Pain experience of the elderly. Pain Management Nursing, 12(4), 190-196. doi:10.1016/j.pmn.2010.05.004 Bruckenthal, P. (2010). Integrating nonpharmacologic and alternative strategies into a comprehensive management approach for older adults with pain. Pain Management Nursing, 11(2), S23-S31. doi:10.1016/j.pmn.2010.03.004 Center for Disease Control and Prevention. (2012). Costs of falls among older adults. Retrieved from http://www.cdc.gov/HomeandRecreationalSafety/Falls/fallcost.html Chau, D., Walker, V., Pai, L., & Cho, L. (2008). Opiates and elderly: Use and side effects. Clinical Interventions in Aging, 3(2), 273-278. Retrieved from http://www.ncbi.nlm.nih.gov.libproxy.library.wmich.edu/pmc/articles/ PMC2546472/pdf/cia-0302-273.pdf Chodko-Zajko, W., Proctor, D. N., Flatarone-Singh, N. A., Minson, C. T., Nigg, C. R., Salem, G. J., & Skinner, J. S. (2009). Exercise and physical activity for older adults. Medicine & Science in Sports Medicine, 41, 1510-1529. doi:10.1249/MSS.0b013e3181a0c95c CHAPTER 3 32 Corbett, K. (2011). Gerontological nursing: Scope and standards of practice. Nebraska Nurse, 44(4), 8. Retrieved from http://nursingald.com/uploads/publication/ pdf/185/NE12_11.pdf Good, M. (1998). A middle range theory of acute pain management: Use in research. Nursing Outlook, 46(3), 120-124. doi:10.1016/S0029-6554(98)90038-0 Good, M., & Moore, S. M. (1996). Clinical practice guidelines as a new source of middle range theory: Focus on pain. Nursing Outlook, 44(2), 74-79. doi:10.1016/S00296554(96)80053-4 Good, M., Stanton-Hicks, M., Grass, J. A., Anderson, G. C., Makii, M., & Geras, J. (2000). Pain after gynecologic surgery. Pain Management Nursing, 1(3), 96-104. doi:10.1053/jpmn.2000.9857 Halaszynski, T.M. (2009). Pain management in the elderly and cognitively impaired patient: The role of regional anesthesia and analgesia. Current Opinion in Anaesthesiology, 22, 594599. doi:10.1097/ACO.0b013e32833020dc Huang, A., & Mallet, L. (2013). Prescribing opioids in older people. Maturitas, 74(2), 123-129. doi:10.1016/j.maturitas.2012.11.002 fulltextPDF/13CF9E760CA756E9C85/6?accountid=10825 Jones, V. M. (2011). Acetaminophen injection: A review of clinical information. Journal of Pain & Palliative Care Pharmacotherapy, 25, 340-349. doi:10.3109/15360288.2011.606293 Kim, E., & Geitsfeld, L. (2008). What makes older adults vulnerable to exploitation or abuse? The Forum for Family and Consumer Issues, 13(1). Retrieved from http://ncsu.edu/ffci/publications/2008/v13n1-2008-spring/index-v13n1-apr2008.php CHAPTER 3 33 Koren-Hakim, T., Weiss, A., Hershkovitz, A., Otzrateni, I., Grosman, B., Frishman, S., . . . Beloosesky, Y. (2012). The relationship between nutritional status of hip fracture operated elderly patients and their functioning, comorbidity and outcome. Clinical Nutrition, 31(6), 917-921. doi:10.1016/j.clnu.2012.03.010 Lachiewicz, P. F. (2013). The role of intravenous acetaminophen in multimodal pain protocols for perioperative orthopedic patients. Orthopedics, 36(2), 15-19. doi:10.3928/01477447-20130122-52 Mak, J., Cameron, I., & March, L. (2010). Evidence-based guidelines for the management of hip fractures in older persons: an update. Medical Journal of Australia, 192 (1), 37-41. Retrieved from http://illiad.ferris.edu/illiad/illiad.dll?Action=10& Form=75&Value=104744. Marik, P. E. (2010). Management of the critically ill geriatric patient. In J. M. O’Donnell, & F. E. Nacul (Eds.), Surgical Intensive Care Medicine (pp. 649-658). doi:10.1007/978-0-387-77893-8_55 McCleane, G. (2010). Pain management in older people. Reviews in Clinical Gerontology, 20 (3), 183-192. doi:10.1017/S0959259810000146 McNicol, E. D., Tzortzopoulou, A., Cepeda, M. S., Francia, M. B., Farhat, T., & Schumann, R. (2011). Single-dose intravenous paracetamol or propacetamol for prevention or treatment of postoperative pain: a systematic review and meta-analysis. British Journal of Anaesthesia, 106(6), 764-775. doi:10.1093/bja/aer107 Olsson, L., Karlsson, J., & Ekman, I. (2007). Effects of nursing interventions within an integrated care pathway for patients with hip fracture. Journal of Advanced Nursing, 58(2), 116-125. doi:10.1111/j.1365-2648.2007.04209.x CHAPTER 3 34 Otten, C., & Dunn, K. (2011). Multimodal analgesia for postoperative total knee arthroplasty. Orthopaedic Nursing, 30(6), 373-380. doi:10.1097/NOR.0b013e318237108a Pergolizzi, J. V., Raffa, R. B., Tallarida, R., Taylor, R., & Labhsetwar, S. A. (2011). Continuous multimechanistic postoperative analgesia: A rationale for transitioning from intravenous acetaminophen and opioids to oral formulations. Pain Practice, 12(2), 137-159. doi:10.1111/j.1533-2500.2011.00476.x. Roth, T., Kammerlander, C., Gosch, M., Luger, T. J., & Blauth, M. (2010). Outcome in geriatric fracture patients and how it can be improved. Osteoporosis International, 21, 615-619. doi:10.1007/s00198-010-1401-4 Smith, H. (2011) Perioperative intravenous acetaminophen and NSAIDS. Pain Medicine, 12, 961-981. doi:10.1111/j.1526-4637.2011.01141.x Voshall, B., Dunn, K. S., & Shelestak, D. (2012). Knowledge and attitudes of pain management among nursing faculty. Pain Management Nursing (Available online 21 March 2012), 1-10. http://doi:10.1016/j.pmn.2012.02.001 White, P. F. (2005). The changing role of non-opioid analgesic techniques in the management of postoperative pain. Anesthesia & Analgesia, 101, S5-S22. doi:10.1213/01.ANE.0000177099.28914.A7 CHAPTER 3 35 IV Acetaminophen Research Proposal Chapter 3 Cathy Bozek, Karen Collins, Beth Kalkman, Lori Van Zoeren, and Joel Vedders Ferris State University CHAPTER 1 36 IV Acetaminophen Research Proposal Chapter 3 For more than ten weeks, the research team consisting of Bozek, Collins, Kalkman, VanZoeren, and Vedders has compiled data to rationalize the need for a research study to validate our proposed hypothesis that the use of IV acetaminophen in the elderly post-operative hip fracture patient is expected to decrease the consumption of opioids. Chapter 1of the proposal focused on the introduction to our research project. An abbreviated literature review was performed based upon our stated hypothesis; the research question was identified; and, a theoretical framework was chosen and discussed. In Chapter 2, a comprehensive literature review provided a detailed explanation of the key concepts related to the proposed study. Gaps in the research were revealed related to the elderly hip fracture population and optimal standards to treat pain. In addition, there were limited studies comparing IV versus oral acetaminophen using a multimodal approach. This confirmed the use of Good and Moore's (1996) theoretical framework pain: a balance between analgesia and side effects (BASE) as an appropriate choice to test the hypothesis. It is believed that a multi-modal approach to pain control will have an effect on outcome measures for these patients including decreased untoward side effects, decreased length of hospital stay, earlier ambulation, and optimal post-operative functioning. In Chapter 3, the focus will be on the design and methodology of the proposed study. The specific research design, sampling plan and method of data collection will be addressed. Additionally, reliability and validity of the chosen instruments will be discussed. As in any research study, we will present the limitations and ethical concerns of this proposal. It will be imperative to choose the proper design and methods to carry out accurate data collection that is untainted with excessive rigor. By the end of this final chapter, the reader should have a clear CHAPTER 3 37 understanding of the entire research proposal and the planned methods for conducting the research. Research Design The study we are proposing is one of experimentation; more specifically, we are planning a type of quantitative research design known as a three-armed, double-blind, placebo controlled randomized controlled trial (RCT). In a RCT, participants are randomly assigned to two or more groups; one group receives standard treatment and the other group (or groups) receives the experimental intervention (Stanley, 2007). There are three defining characteristics of a RCT: manipulation, control, and randomization (Polit & Beck, 2012). We will be determining the effect of manipulating the route of acetaminophen administration on opioid consumption in the chosen population for 48 hours post-operatively. In addition, we will be providing a counterfactual (or control group) which helps to validate the relationship between the independent and dependent variables by removing the independent variable from one group in the sample (Polit & Beck, 2012). By including a non-intervention group, we can better determine that the observed results are attributable to the independent variable (Polit & Beck, 2012). Furthermore, we will randomly assign subjects from the study sample to one of three groups: IV administration of acetaminophen, oral administration of acetaminophen, or no acetaminophen administration. Randomization helps to remove the potential for researcher bias (Stanley, 2007; Wood & Ross-Kerr, 2011). To double-blind this study, where caregiver and patient are unaware of the treatment assignment (Polit & Beck, 2012), it will be necessary for all participants to receive IV and oral "medication" simultaneously every six hours. For two of the groups, one route will contain acetaminophen whereas the other will contain a placebo. In the control group, neither route will CHAPTER 3 38 contain acetaminophen. Providing the intervention in this manner will protect against the Hawthorne effect, an elevated response due to participation in a research study (Polit & Beck, 2012). All other care provision will be identical between groups. An area of consideration in an RCT is the principle of clinical equipoise (Stanley, 2007). Under this ethical principle, a researcher cannot intentionally submit research participants to interventions which are knowingly sub-standard (Stanley, 2007). Therefore, all groups within a study must receive treatment that is, at the minimum, provided at the current accepted standard of care. Because the literature supports opioids in standard pain management following orthopedic surgery (Vadivelu, Mitra, & Narayan, 2010), opioids will be available and utilized within our study. The question our research seeks to answer is whether intravenous acetaminophen will decrease the use of opioids in the target population. Setting and Sample Setting The setting for our proposed research study is a dedicated orthopedic care unit specializing in fracture repair located at a Level 1 regional trauma center in West Michigan. It is estimated that this facility repairs more than 400 intertrochanteric (IT) fractures every year providing a sufficiently large population from which to recruit our study sample. Furthermore, this trauma center is known for its on-going participation in research and its provision of stateof-the-art care. Performing our proposed research in this single-site setting will lend credibility to our proposed research, ease sample recruitment, result in consistent quality service to study participants, and also provide a supportive environment for novice researchers. CHAPTER 3 39 Sample As stated in the research hypothesis, our population of interest is the elderly (age 65 and older) hip fracture patient. Polit and Beck (2012) emphasize that a target population is best represented by a sampling which accurately reflects the common features of the desired group. Chapter 2 of our proposal clearly describes the unique characteristics of the elderly. Inclusion of these characteristics will be intentional during the recruitment process thereby strengthening the study's external validity (Wood & Ross-Kerr, 2011). Conversely, in order to strengthen the internal validity of our study, some variability within the sample must be controlled (Polit & Beck, 2012). For example, there are a variety of orthopedic repair techniques which differ in degree of invasiveness based on the presentation of the hip fracture. To decrease the potential risk of study results being attributed to variations in methods of repair, only those patients undergoing an open reduction internal fixation (ORIF) for an IT fracture will be eligible for study inclusion. After careful consideration by the research team the following eligibility criteria have been determined: Inclusion criteria: 1. Age: 65 years and older. 2. Gender: Male or female. 3. Race: No limitation. 4. Cognition: Alert and oriented as determined by a satisfactory score on the MiniMental State Exam (MMSE) (see Appendix A). 5. Social: Family support identified. 6. Nutritional status: Adequate. CHAPTER 3 40 7. Medication: No allergies to acetaminophen or opioids. No identified potential drugdrug interactions between acetaminophen or opioids and patient's current medication list. 8. Injury: Isolated IT fracture. 9. Literacy: English speaking and/or reading, or ability to give informed consent through use of interpretive services. Exclusion criteria: 1. The inverse to any of the above criteria. 2. Current treatment with opioids for conditions such as chronic pain. 3. Existence of severe liver disease. 4. Inability to swallow. Regulatory criteria: 1. The study must have signed approval by the appropriate governing body at the proposed research site. If Institutional Review Board (IRB) approval is deemed necessary, this will be achieved and documented. 2. A signed informed consent must be documented and kept available for each study participant. 3. Ethical concerns must be addressed and have satisfactory resolution prior to conducting the study (Wood & Ross-Kerr, 2011). Intact cognition will be determined through the administration of the MMSE by individuals trained in the administration and scoring of this test. This 10-15 minute test includes examination of memory, orientation, attention, recall and abstract thinking (Feliciano, Baker, Anderson, LeBlanc, & Orchanian, 2011). The MMSE has been extensively researched and CHAPTER 3 41 validated with "interrater correlations of r=.82 and test-retest reliability ranging from r=.89 to r=.98 and sensitivity and specificity rates of 71% and 95.6% in hospitalized patients" (Feliciano et al., 2011, p.2). Due to the administration time of this test being considerably less than that of another commonly used test, the Cognitive Assessment of Minnesota (CAM) which takes 35-45 minutes to administer (Feliciano et al., 2011, p.2), the choice was made to use the MMSE. Because we have identified a specific setting for this study and we have a target population of the elderly hip fracture patient, consecutive sampling will be used to obtain the necessary subjects. A power analysis will be performed by a research statistician to determine the necessary sample size. Per Polit and Beck's (2012) definition of consecutive sampling, all individuals who present to the trauma center during sample recruitment and meet the eligibility criteria for the study will be approached for study inclusion. All information related to the study will be discussed with the individual in order to obtain informed consent. Once consent is gained, the patient will be enrolled in the study and randomized into a particular treatment group. Methods In order to have a study that is free of bias, blinding must occur. Blinding eliminates three types of bias. The first type is expectation bias; if the patient is unaware of which drug is being administered the outcome cannot be influenced by the patient's expectation of its efficacy (Polit & Beck, 2012, p.212). Secondly, performance bias is eliminated; if the care provider is unaware of which agent is being administered, it will eliminate differences in care provided to different groups (Polit & Beck, 2012). For example, if the nurse was aware the patient was receiving placebo only, he or she may implement other methods of pain control such as ice to the surgical site, or spend more time teaching relaxation techniques. The third type of bias, detection bias, will be controlled by utilizing the Numeric Rating Scale (NRS) to measure pain which CHAPTER 3 42 allows no room for recording variations in outcome variables. This method provides transparency which allows for multiple researchers to deliver the same method of assessment and acquire the same results (Burns & Groves, 2007). Study Variables Post-operative order sets will be developed for the purpose of the study through a collaborative effort by the orthopedic surgeons, nursing staff, and researchers. The orders will include routine post-operative orthopedic orders with the addition of the administration of the randomized intervention. The primary investigator (PI) will draw an envelope containing postoperative orders from a box holding the appropriate number of envelopes as determined by the power analysis. Once the patient is awake, alert, and able to swallow pills following surgery, he or she will receive administration of the first randomly assigned dose as determined by the post-op orders. The pharmacy will then be notified of the time of administration of this initial dose and will schedule consecutive doses every six hours for 48 hours on the electronic medication administration record (EMAR). Prior to the administration of each dose the patient's pain will be assessed and recorded using the eleven point NRS with numbers ranging from zero to ten. Zero represents no pain while ten represents the worst pain possible (see Appendix B). According to Hawker, Mian, Kendzerska, and French (2011), the advantage of the NRS scale over the visual analog scale (VAS) is its simplicity, scoring, and the fact that it can be administered both verbally and in writing. It also takes less time to administer, is easy to complete, and can be used across cultures and languages (2011). The NRS has also shown high reliability and validity. "High test-retest reliability has been observed in both literate and illiterate patients. For construct validity, it is shown to be highly correlated to the VAS" CHAPTER 3 43 (Hawker et al., 2011, p. 242). Hjermstad et al. (2011) echo those results; the NRS and the VAS were viewed as the most reliable and easiest to use. According to Flaherty (2012), the NRS is the most widely utilized pain intensity scale administered in older adults. We, therefore, felt this measurement tool was best suited for our study. The patient's pain will also be scored and recorded 30 minutes after administration of the study dose in the electronic medical record (EMR). Additionally, the facility's routine ongoing pain assessment protocols will be followed. Opioids will be administered for further pain control when requested by the patient. Opioid usage during the 48 hour postoperative period will be tallied from the EMR. The PI will be able to gather this information by chart review after the 48 hour time frame has ended. This information will then be submitted for data analysis. Data Analysis Through a power analysis, we expect to recruit a large enough sample size to use the multivariate analysis of variance (MANOVA) to analyze and compare the data. MANOVA is an extension of the analysis of variance (ANOVA); the parametric procedure for testing differences between means when there are at least three groups to be studied (Polit & Beck, 2012). MANOVA will also increase control for the proposed research, due to its ability to look at the significance of the differences between dependent variables (Polit & Beck, 2012). MANOVA compares the significance of differences for multiple dependent variables (Polit & Beck, 2012, p. 446). If, as per the guidance of an experienced researcher, we are unable to obtain the necessary sample size, a simple ANOVA will be performed (Ford, personal communication, April 15, 2013). Utilization of a double-blind technique will have patients serve as their own controls for the comparison between the two routes of administration of acetaminophen. CHAPTER 3 44 In addition to pain and opioid use, data will be extracted from the EMR related to falls, constipation, delirium, nausea and vomiting. Data will be entered into the most current addition of the Statistical Package for the Social Sciences (SPSS). A paid researcher familiar with this software will enter the data. Descriptive statistics will compare the mean, mode, and median of the amounts of rescue opioids used in conjunction with the route of acetaminophen or placebo. By utilizing SPSS to input data and perform a two-tailed test, we will test at the 0.05 level of significance. Rejection of our null hypothesis will occur if the results are greater than 0.05 (Polit & Beck, 2012, p.409). We can also run a multiple linear regression in SPSS to view the relationship between the multiple variables or provide scatter plots which will show the relationship between the independent and dependent variables. Reliability and Validity A Level III research study “demands the highest degree of validity and reliability testing” (Wood & Ross-Kerr, 2011, p. 203). For this reason, we have chosen to utilize well-known measurement tools that have been tested and proven to be reliable and valid. Reliability is the “degree of consistency or dependability with which an instrument measures an attribute” (Polit & Beck, 2012, p. 741). This equates to the measure’s stability, consistency, or dependability. These components need to be accurate for the study to be reproducible. Validity is a quality criterion referring to the degree by which inferences made in a study are accurate and well founded (Polit & Beck, 2012). Validity in measurement is the “degree to which an instrument measures what it is intended to measure” (Polit & Beck, 2012, p. 745). In this proposed study, control of experimental conditions will be enhanced by keeping procedures as consistent as possible. For example, as we are focusing our study on one type of CHAPTER 3 45 hip fracture repair, ORIF of an IT fracture, discrepancies in surgical technique will be minimized. Equipment will also remain constant. In addition, we will utilize a well-known pain scale. The NRS has been chosen due to its ease in use with both the patients and the nursing staff. The reliability and validity of the NRS was discussed earlier in this paper, on page 8. The nursing staff will receive instruction by one trainer regarding the utilization of the NRS pain scale and the importance of documenting pain accurately throughout the pre- and post-intervention periods. Using one trainer will decrease teaching bias among several different trainers. Another measurement tool, the Confusion Assessment Method (CAM), will be used to detect delirium among our chosen population post-operatively (see Appendix C). The CAM tool is valid and shows high interrater reliability (kappa=0.79-0.96) (Tate & Happ, 2012, para 4). This test is also easy to administer with minimal training. Testing time is about 2 minutes (Tate & Happ, 2012). Both the NRS and the CAM scales will be serially addressed at regular prescribed intervals and documented in the EMR. Limitations Despite careful preparation and planning, there will be questions that remain unanswered after conducting a research study. It is important for researchers to have appropriate expectations for their work. This requires a discussion related to the potential limitations of the research proposal. For example, limitations of this study include the possibility that despite training and education of nursing staff and test administrators related to the goals of this study, there may still be variance in administration of the intervention, patient assessment, and documentation of study data. CHAPTER 3 46 Due to the age of our sample population, attrition is also a very real threat to this study's success. Although efforts have been made through the inclusion criteria to reduce the risk of attrition, there still remains the possibility that untoward events will cause unavoidable removal from the study. Possible reasons for removal include intolerance of medication administration, error in medication administration, unforeseen medical events, development of delirium, or death. In addition, this study is targeted to the elderly population. Reasons for this have been validated in earlier chapters of this study proposal. This does mean, however, that findings from this study may not be applicable to people of different age groups.Additional limitations may be discovered after completion of the study and analysis of the data. Ethical Concerns When performing research on human beings, especially a vulnerable population such as the elderly, there are ethical concerns to be considered. Involved with this, is the safeguarding of ethical concepts such as beneficence, preservation of human dignity, and justice (Polit & Beck, 2012). The authors of this research proposal will ensure that the study is performed with the utmost integrity by qualified personnel. Informed consent will be obtained in writing after full disclosure of the study's purposes has occurred. Potential participants will have the opportunity to ask questions and request clarification related to the study before signing consent. Participants will also be fully aware of their right to withdraw from the study at any time without question. Participants will be asked to grant permission for dissemination of study results, should this study be recommended for publication. CHAPTER 3 47 As within any healthcare system, confidentiality of patient information and privacy will be maintained. Participant anonymity will be further protected by assigning identification numbers to de-identify individual patient data for reference purposes during data extraction from the EMR. The PI will take the obtained information and deliver it to the paid research statistician who will have signed an agreement of confidentiality prior to handling study data. In addition, the researchers believe the results of this study to be of potential significant benefit to the elderly hip fracture population. Standard post-operative pain management will not be withheld from these patients thereby protecting subjects from clinical equipoise. Rather, by adding IV acetaminophen as an adjunct therapy, we believe there will be a change in postoperative opioid usage. Finally, as previously stated in the text, the proposal will be submitted for review to the IRB of the proposed study site. The IRB of any facility conducting a research study must approve all research prior to implementation to safeguard patient protection and the ethical integrity of the research (ANA, 2010). This board, consisting of experts in research and risk management, will examine the proposal to disclose any unaddressed ethical concerns specific to performing this study on the elderly hip fracture population. Any identified concerns will be corrected by the researchers prior to re-submission of the proposal for IRB approval. Summary In summary, Chapters 1 and 2 have developed rationale for our research proposal in depth. A hypothesis has been developed, research questions posed, literature reviewed, significant variables discussed, and a theoretical framework created. Now, in Chapter 3, specifics related to the research design, methods, setting and sample including inclusion criteria, data analysis, reliability and validity of our chosen tools, limitations, and ethical considerations CHAPTER 3 have been addressed. It is the opinion of these authors that this research proposal has the potential to provide valuable information to ensure evidence based care for this vulnerable population. 48 CHAPTER 3 49 References American Nurses Association (ANA, 2010). Guide to the code of ethics for nurses: interpretation and application. Silver Spring, MD: Nursesbooks.org. Burns, N., & Groves, S. K. (2007). Understanding nursing research (4th ed.). St Louis, MO: Sanders Elsevier. Feliciano, L., Baker, J. C., Anderson, S. L., LeBlanc, L. A., &Orchanian, D. M. (2011).Concurrent validity of the cognitive assessment of Minnesota in older adults with and without depressive symptoms.Journal of Aging Research, 2011, 1-6. http://dx.doi.org/10.4061/2011/853624 Flaherty, E. (2012). Best practices in nursing care to older adults. Retrieved from http://consultgerirn.org/uploads/File/trythis/try_this_7.pdf Hawker, G. A., Mian, S., Kendzerska, T., & French, M. (2011).Measures of adult pain. Arthritis Care and Research, 63(11), 240-252. http://dx.doi.org/10.1002/acr.20543 Hjermstad, M. J., Fayers, P.M., Haugen, D. F., Carceni, A., Hanks, G. W., Loge, J. H., Kaasa, S. (2011). Studies comparing numerical rating scales for assessment of pain intensity in adults: a systematic literature review. Journal of Pain and Symptom Management, 41, 1073-1092. http://dx.doi.org/10.1016/j.jpainsymman.2010.08.016 Polit, D. F., & Beck, C. T. (2012). Nursing research: Generating and assessing evidence for nursing practice (9th ed.). Philadelphia, PA: Lippincott, Williams & Wilkins. Stanley, K. (2007). Statistical primer for cardiovascular research: Design of randomized controlled trials. Circulation, 115, 1164-1169. http://dx.doi.org/10.1161/CIRCULATIONAHA.105.594945 CHAPTER 3 50 Tate, J. A., &Happ, M. B. (2012).The confusion assessment method for the ICU (CAM-ICU) [Issue brief 25]. Retrieved from The Hartford Institute for Geriatric Nursing, New York University, College of Nursing. www.harfordign.org Vadivelu, N., Mitra, S., & Narayan, D. (2010). Recent advances in post-operative pain management. Yale Journal of Biology and Medicine, 83, 11-25. Wood, M. J., & Ross-Kerr, J. C. (2011). Basic steps in planning nursing research: From question to proposal (7th ed.). Sudbury, MA: Jones and Bartlett. CHAPTER 3 51 Appendix A CHAPTER 3 52 Appendix B CHAPTER 3 53 Appendix C The Confusion Assessment Method Instrument: 1. [Acute Onset] Is there evidence of an acute change in mental status from the patient’s baseline? 2A. [Inattention] Did the patient have difficulty focusing attention, for example, being easily distractible, or having difficulty keeping track of what was being said? 2B. (If present or abnormal) Did this behavior fluctuate during the interview, that is, tend to come and go or increase and decrease in severity? 3. [Disorganized thinking] Was the patient’s thinking disorganized or incoherent, such as rambling or irrelevant conversation, unclear or illogical flow of ideas, or unpredictable switching from subject to subject? 4. [Altered level of consciousness] .Overall, how would you rate this patient’s level of consciousness? (Alert [normal]; Vigilant [hyperalert, overly sensitive to environmental stimuli, startled very easily], Lethargic [drowsy, easily aroused]; Stupor [difficult to arouse]; Coma; [unarousable]; Uncertain) 5. [Disorientation] Was the patient disoriented at any time during the interview, such as thinking that he or she was somewhere other than the hospital, using the wrong bed, or misjudging the time of day? 6. [Memory impairment] Did the patient demonstrate any memory problems during the interview, such as inability to remember events in the hospital or difficulty remembering instructions? 7. [Perceptual disturbances] Did the patient have any evidence of perceptual disturbances, for example, hallucinations, illusions or misinterpretations (such as thinking something was moving when it was not)? 8A. [Psychomotor agitation] At any time during the interview did the patient have an unusually increased level of motor activity such as restlessness, picking at bedclothes, tapping fingers or making frequent sudden changes of position? 8B. [Psychomotor retardation].At any time during the interview did the patient have an unusually decreased level of motor activity such as sluggishness, staring into space, staying in one position for a long time or moving very slowly? 9. [Altered sleep-wake cycle]. Did the patient have evidence of disturbance of the sleep-wake cycle, such as CHAPTER 3 54 excessive daytime sleepiness with insomnia at night? The Confusion Assessment Method (CAM) Diagnostic Algorithm Feature 1: Acute Onset and Fluctuating Course This feature is usually obtained from a family member or nurse and is shown by positive responses to the following questions: Is there evidence of an acute change in mental status from the patient’s baseline? Did the (abnormal) behavior fluctuate during the day, that is, tend to come and go, or increase and decrease in severity? Feature 2: Inattention This feature is shown by a positive response to the following question: Did the patient have difficulty focusing attention, for example, being easily distractible, or having difficulty keeping track of what was being said? Feature 3: Disorganized thinking This feature is shown by a positive response to the following question: Was the patient’s thinking disorganized or incoherent, such as rambling or irrelevant conversation, unclear or illogical flow of ideas, or unpredictable switching from subject to subject? Feature 4: Altered Level of consciousness This feature is shown by any answer other than “alert” to the following question: Overall, how would you rate this patient’s level of consciousness? (alert [normal]), vigilant [hyperalert], lethargic [drowsy, easily aroused], stupor [difficult to arouse], or coma [unarousable]) The diagnosis of delirium by CAM requires the presence of features 1 and 2 and either 3 or 4. CAM Instrument and Algorithim adapted from Inouye, S., van Dyck, C., Alessi, C., Balkin, S., Siegal, A. &Horwitz, R.(1990). Clarifying confusion: the confusion assessment method. Annals of Internal Medicine, 113(12), 941-948.