Building alliance to address mental health in - ABLE
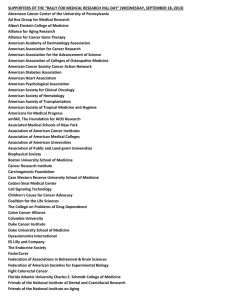
advertisement

Building alliance to address mental health in primary care Larry Wissow, MD MPH Johns Hopkins School of Public Health, Baltimore, MD Goals • Learn about the importance of alliance (patient-doctor; patient-staff; patient-office) in promoting the care of mental health problems • Learn some techniques for fostering patientdoctor alliance • Using the alliance to ask about things that patients/parents might not expect you to ask about Disclosure • No conflicts to report • Grateful to funders and collaborators – Duke Endowment – National Institute of Mental Health – Dr. Anne Gadomski (Bassett Healthcare) • Oregon Pediatric Society Cases to think about • Foster parent brings in the bag of pills and says they aren’t working • Parent seems depressed or has revealed problems on a screening form • In the middle of a short medical visit the family raises a mental health issue Background/philosophy • Pediatric practices see same range of severity as child psychiatrists – But distribution varies • Many different ways to cope – Good triage – Develop your own skills – Co-locate with mental health Core needs • Efficiently rule out emergencies • Provide immediate relief and advice • Develop a mutually agreeable plan for next steps • Stay in control of the visit and balance the needs of this patient with the needs of others To meet core needs • Core capability for any solution might be called “alliance” with family – Partnership, engagement… • Data from adult primary care studies of depression treatment – Relationship with provider predicted engagement and outcome Van Os TW. J Affect Disord 2005;84:43-51. Frémongt P. Encephale 2008;34:205-10. Why start with a focus on alliance? • Advice alone isn’t enough – < 50% of psychosocial concerns disclosed – < 50% of mental health referrals kept – < 50% of children who start mental health treatment finish • Evidence from psychotherapy – Predicts outcome over and above any specific treatment (including medications) Elements of alliance in psychotherapy • Agreement on nature of problem • Agreement on what to do (and when to do it) • “Affective bond” with provider – Trust – Optimism – Relief Why alliance especially with mental health issues? • Particularly stigmatizing • Doubt and equivocation part of the “illness” • Not sure that you’re the one to tell • Afraid to hear the answer What builds alliance? • Evidence that process starts with initial interaction with office – Image of relationship built from staff as a whole, not just the pediatrician – Patients value flexible, open staff who can • • • • pinch hit for each other help trouble shoot problems speed things up when needed realize when the patient’s context has changed Ware NC. Psychiatr Serv. 1999;50:395-400. Pulido R. Arch Psych Nursing 2008;22:277-87. Patient trust and practice climate • Adult primary care patients’ trust in provider related to: – Physicians and staff reporting better collaboration with each other, more autonomy, ability to delegate to each other • Trust then relates to: – Attribution of influence over healthy behaviors to provider recommendations Becker ER, Medical Care 2008;46:795-805 Alliance building 1:1 1. Feeling heard and understood (the bond) 2. Seeking agreement on a working formulation of the problem 3. Seeking permission to offer advice 1. Feeling heard and understood • Heard: active listening – Creating the illusion of taking time – Verbal and non-verbal indicators of paying attention – Actions that “co-construct” the story • Understood: agreement on the nature of the concerns and the highest priorities 2. Seeking agreement on a working formulation of the problem • Asking for permission to gather more information – Opportunity to open up more sensitive areas, rule outs, emergencies • Asking for permission to offer a preliminary idea of the problem – Asking if you’ve got it – Cycling back to more questions 3. Seeking permission to offer advice • Ready to act? – If not, what would it take? • What can we do now? • What might we need to do next? • Responding to “no” 1. Feeling heard and understood Shaping concerns and managing time • • • • Open-ended questions Anything else? Breaking into the story Managing the two-patient visit Skills for rambling (co-construction) 1. “I want to make sure we don’t run out of time…” 2. Summarize your understanding and ask for additional concerns 3. Specifically ask for focus • • • “Which one of those is hardest?” “Pick one of those to start with.” Ask for a specific example “Pick one” Click box to start film clip 0021/Example7 Two in the visit: skills when turn-taking interrupted • Possible tactics Shift in body language • Acknowledge and re-direct • Reminder of “rules” • • Considerations Timing • Status of person interrupting or interrupted • “Enforcing” taking turns - child Skills when participants are angry at each other • Rationale – Want to manage negative affect in the visit (and help people move on to problem solving) – Want to demonstrate that dialog is possible • Several “flavors” of extreme statements – “Black or white” statements leave no room for discussion – Critical comments about family members – Set-ups involving vague, value-laden goals Responding to “black or white” • Characterized by “always,” “never,” or similar words • Point out and ask for restatement – Be prepared if you choose to challenge the generalization – Alternative: ask for “something easier to hear” Responding to “black or white” with “say something easier” Click box to start film clip mhvg0010/stronglang Common issues in agenda setting • • • Parent and child/youth have different priorities Family priorities not same as yours’ Opportunities for additional visits are limited • You really do want to accomplish more than you have time for! Skills for agenda setting • • • • • Making sure this process is clear to patient/parent Playing back the list of concerns Asking for priorities Getting agreement from all parties Openly and collaboratively problem solve about limitations on follow-up visits 2. Getting to agreement on a working formulation • Why ask for permission to get more information? • What is it that you want to know? – Sensitive but important details – Data related to possibly urgent treatment needs (including overall level of function) – What they think might be the underlying cause Small group task • Pick a common condition (ie, depression) • Brainstorm most efficient ways to ask about: – Overall function and possible indicators of need for urgent care – Sensitive but possibly important information related to the child or family – Initial somatic causes/rule outs – What child/family has already thought about as cause/underlying issue Reports from groups • Focus on the first 2-3 minutes worth of questions that will help you decide where you are going with this problem Hint about severity/function • Questions from “SDQ” – Do the difficulties you mentioned distress you (teen) or your child (younger child)? • How much? – How much do they interfere with life? • • • • At home With friends In school In other activities 3. Asking for permission to offer advice • Summing up your thinking and checking for agreement – May need to cycle back to get more information • Do they still agree that this is something they want to do something about? – If no, what should be monitored, what would it take? Giving advice • Rationale – Being directive can fail even when people want help • Anxiety, ambivalence, shame, loss of control – Medical provider is usually not the first person in the chain of consultation • People come with prior ideas and opinions (about cause, condition, treatment) that need to be incorporated – People will accept advice they can’t follow • Need to actively identify barriers Asking about readiness to act • People may be aware of a problem but not yet ready to act on it – The kind of advice needed depends on this “stage of change” – Mis-matched advice likely to be rejected • If ready: get permission to give advice • If not ready: what would motivate action? What would be grounds to act? Click box to start film clip Gloss2/whatwouldittake2 When you get to give advice • Ask for permission – Helps patients maintain sense of control • Ask for their ideas • Offer advice as set of choices – Preferably include their ideas among choices • Frame as short and long term plans – What might help now – What diagnostic steps to take Asking about barriers • Easy to skip this step in a quick visit • Evidence suggests even motivated patients appreciate help with logistics • Asking allows people to think through and get more committed to plan • Opportunity to build alliance and anticipate “resistance” Responding to “resistance” • Overall, emphasize choice and time to discuss • Apologize for getting ahead • Agreeing with a twist • What would it take? Getting information: apologize for “getting ahead” Click box to start film clip gloss10/example3_9cine Getting information: what would be grounds to act? Click box to start film clip example3_10cine Agree “with a twist” and inform Click box to start film clip example3_11cine Summing up • Evidence suggests these skills are worth the time it takes to use them – Also suggests they don’t take that much time • It’s a team effort – worth thinking about who on the team does what part best • Only a part of building a larger system of care – But may be an essential part Much thanks