Ethics PPT
advertisement

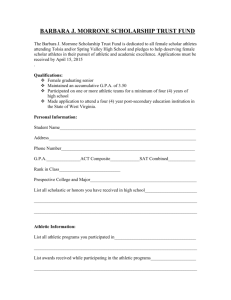
Ethics Ethics in Athletic Training Terminology • Ethics: • the moral principles that determine a person’s conduct • Dictionary Def. - moral principles that govern a person's or group's behavior • Origin - Greek word "ethos" meaning “character" • Morals: • beliefs based on a person’s ideas of what is right and wrong • Dictionary Def. - a person's standards of behavior or beliefs concerning what is and is not acceptable for them to do • Origin - Latin word "mos" meaning "custom" Ethics vs. Morals: What are they? Ethics Morals • The rules of conduct recognized in respect to a particular class of human actions or a particular group or culture. • Where do they come from? • Principles or habits with respect to right or wrong conduct. While morals also prescribe dos and don'ts, morality is ultimately a personal compass of right and wrong • Where do they come from? • Social system – External • Why do we do it? • Because society says it is the right thing to do. • Individual – Internal • Why do we do it? • Because we believe in something being right or wrong. Ethics vs. Morals: The Gray Ethics Morals • A person strictly following Ethical Principles may not have any Morals at all. Likewise, one could violate Ethical Principles within a given system of rules in order to maintain Moral integrity. • Flexibility – • A Moral Person although perhaps bound by a higher covenant, may choose to follow a code of ethics as it would apply to a system. "Make it fit“ • Flexibility – • Ethics are dependent on others for definition. They tend to be consistent within a certain context, but can vary between contexts. • Usually consistent, although can change if an individual’s beliefs change. NATA Code of Ethics 1. Members shall respect the rights, welfare and dignity of all. 2. Members shall comply with the laws and regulations governing the practice of athletic training. 3. Members shall maintain and promote high standards in their provision of services. 4. Members shall not engage in conduct that could be construed as a conflict of interest Principle 1 • Members shall respect the rights, welfare and dignity of all. • 1.1 Members shall not discriminate against any legally protected class. • 1.2 Members shall be committed to providing competent care. • 1.3 Members shall preserve the confidentiality of privileged information and shall not release such information to a third party not involved in the patient’s care without a release unless required by law. Principle 2 • Members shall comply with the laws and regulations governing the practice of athletic training. • 2.1 Members shall comply with applicable local, state, and federal laws and institutional guidelines. • 2.2 Members shall be familiar with and abide by all National Athletic Trainers’ Association standards, rules and regulations. • 2.3 Members shall report illegal or unethical practices related to athletic training to the appropriate person or authority. • 2.4 Members shall avoid substance abuse and, when necessary, seek rehabilitation for chemical dependency. Principle 3 • Members shall maintain and promote high standards in their provision of services. • 3.1 Members shall not misrepresent, either directly or indirectly, their skills, training, professional credentials, identity or services. • 3.2 Members shall provide only those services for which they are qualified through education or experience and which are allowed by their practice acts and other pertinent regulation. • 3.3 Members shall provide services, make referrals, and seek compensation only for those services that are necessary. • 3.4 Members shall recognize the need for continuing education and participate in educational activities that enhance their skills and knowledge. • 3.5 Members shall educate those whom they supervise in the practice of athletic training about the Code of Ethics and stress the importance of adherence. • 3.6 Members who are researchers or educators should maintain and promote ethical conduct in research and educational activities. Principle 4 • Members shall not engage in conduct that could be construed as a conflict of interest • 4.1 Members should conduct themselves personally and professionally in a manner that does not compromise their professional responsibilities or the practice of athletic training. • 4.2 National Athletic Trainers’ Association current or past volunteer leaders shall not use the NATA logo in the endorsement of products or services or exploit their affiliation with the NATA in a manner that reflects badly upon the profession. • 4.3 Members shall not place financial gain above the patient‘s welfare and shall not participate in any arrangement that exploits the patient. • 4.4 Members shall not, through direct or indirect means, use information obtained in the course of the practice of athletic training to try to influence the score or outcome of an athletic event, or attempt to induce financial gain through gambling. Cultural Competence Terminology • Cultural competence: • an awareness of belief and values between cultures • Other definitions: • Possession of the knowledge and skills required to manage cross-cultural relationships effectively. • Cultural incompetence in doctors and other medical staff can seriously prejudice clinical management. • Social medicine; The ability to understand, appreciate, and interact with persons from cultures and/or belief systems other than one's own • Defined simply as the level of knowledge-based skills required to provide effective clinical care to patients from a particular ethnic or racial group Verbal Communication 1. Greet the person 2. Call them by name & pronounce his/her name correctly 3. Determine the person’s language and level of English proficiency (speaking, reading and writing) Non-Verbal Communication 1. Personal space • *Close or distant personal space • *Tactile person vs. non-contact person • (Always follow the person’s lead!) 2. Gestures – not universal! • *Pointing at a person - used to call someone or may be considered impolite • *Smiling & nodding may indicate politeness, not understanding or agreement • *Direct eye contact – considered disrespectful in some cultures Non-Verbal Communication 3. Silence – what does it mean? • *Thinking of an answer? • *Doesn’t understand / confused? • *Angry 4. Expressions of pain • *Stoic (afraid to show pain / sign of weakness) • *Emotive (open expression / likes to share) Cultural Considerations 1. Language used in social vs. personal conversation 2. Social organization of the family (head = father or mother? Who makes important decisions?) 3. Traditional or cultural practices (beliefs concerning injuries, healing, use of medicine, etc.) 4. Spiritual or religious practices (ie, fasting during Ramadan) Cultural Considerations 5. Observance of Ethnic & Religious holidays 6. Views of appropriate touch • • • Cultural meaning / significance Religious considerations (body covered?) Always ask for permission! 7. Health issues or disparities • • Diet restrictions Sickle cell & asthma more prevalent in African Americans Cultural Considerations 8. Narrative or storytelling • • Chronological (sequential) Episodic history (highlights major events) 9. Orientation to time • • Future time – value being early/on time Present time – here & now, not worried about the future Legal Liability Terminology • Negligence • A failure to act as a reasonably prudent person would • Gross negligence • A step beyond negligence; failure to provide minimal care • Assumption of risk • An individual may be injured as a result of participating in sports • Permission to treat • Consent obtained from athlete or parent before a medical procedure is performed Terminology • Proximate cause • A direct connection between an individual’s actions and an injury to a second person • Breach of duty • A failure to perform one’s job Components of a Lawsuit 1. Duty 2. Breach of Duty 3. Actual Injury 4. Proximate Cause Professional Ethics Terminology • National Athletic Trainers’ Association (NATA) • The professional membership organization for athletic trainers • Arizona Athletic Trainers’ Association (AzATA) • The membership organization for athletic trainers in Arizona • Board of Certification (BOC) • Provides an entry-level certification program for AT’s, review the standards for the practice of athletic training, and reviews the requirements for continuing education for certified athletic trainers • Continuing education units (CEUs) • Contact hours of additional learning NATA Requirements 1. EDUCATION • Earn a bachelor’s or master’s degree in athletic training from an approved athletic training program • There are 360 entry-level programs throughout the United States • To find a college or university with an approved program, go to http://www.caate.net/ 2. CERTIFICATION • Take and pass the Board of Certification (BOC) exam • For information on the exam, see the BOC website: http://www.bocatc.org/index.php?option=com_content&view=article&id=10&Itemid=8 NATA Requirements 3. STATE LICENSURE • Comply with the laws of the state where he/she practices • Each state has its own requirements for practicing athletic training NATA Member Expectations • Once a member, NATA expects its members to follow certain standards • One of these is the Code of Ethics • For a copy of the NATA’s Standards and Sanctions, go to: • http://www.nata.org/sites/default/files/membership-standards.pdf Recertification Requirements • Requirements for Recertification by the BOC* 1. Follow NATA standards 2. Maintain certification in Emergency Cardiac Care 3. Complete continuing education units (CEU’s) in different areas of study • 50 CEUs every 2 years ( 10 need to be EBP CEUs) 4. Payment of recertification fee http://www.bocatc.org/images/stories/athletic_trainers/recertificationrequirements2013.p df Requirements for State Licensure • Each state has different requirements • Arizona requirements 1. 2. 3. 4. College transcripts Proof of certification from BOC Proof of citizenship / right to work in the United States Fee for licensing process • http://www.athletictrainingboard.az.gov/default.asp • Renewal Requirements • Annual renewal form • Pay recertification fee • For more information, see: http://www.athletictrainingboard.az.gov/board_info/statutes.asp Supervisory Responsibilities Terminology • Certified Athletic Trainer (AT or ATC): • An athletic trainer is a certified health care professional who practices in the field of sports medicine. • Certified athletic trainers are allied health care providers who specialize in the prevention, assessment, treatment and rehabilitation of injuries and illnesses that occur to athletes and the physically active. (NATA definition) • Athletic Training Student Aides (ATSAs): • students who act under the direct supervision of an athletic trainer Responsibilities of ATSA’s • • • • • • • • Stock first aid kit Check equipment Stock ice chest Fill water bottles Check injury list from previous practice or game Communicate with AT and coaches Check out equipment Help with treatment & taping under direct supervision of their sponsoring athletic trainer • Clean training room before & after game or practice • Update supply list • Review activities NATA Position Statement on Student Aides • Excerpts: • Student aides must only observe the licensed/certified athletic trainer outside of the educational environment. Coaches and school administrators must not allow or expect student aides to assist or act independently with regard to the evaluation, assessment, treatment and rehabilitation of injuries. Additionally, it is paramount that student aides not be expected, asked or permitted to make “return to play” decisions. • Specifically, licensed/certified athletic trainers, coaches and administrators must not ask athletic training student aides to engage in any of the following activities: 1. 2. 3. 4. 5. Interpreting referrals from other healthcare providers Performing evaluations on a patient Making decisions about treatments, procedures or activities Planning patient care Independently providing athletic training services during team travel Equipment Safety Terminology • National Operating Committee on Standards for Athletic Equipment (NOCSAE): • an organization that works to improve athletic equipment in order to decrease sport-related injuries • http://nocsae.org/ • Catastrophic injury: • a sports injury resulting in a brain or spinal cord injury, or a fracture of the skull or spine Sports That Require Helmets • Bicycling • Skating • BMX • Downhill Mountain biking • Longboarding • Skateboarding • ATV • Motocross • Go-Karting • Motorcycles • Bull riding • Horseback (equestrian) • Rock climbing • Baseball • Softball • Football • Ice hockey • Lacrosse • Polo • Snowboarding • Snowmobiling NOCSAE Seal • Why is NOCSAE seal so important? 1. Indicates that the helmet was made to meet certain standards 2. Even though the helmet is certified, an injury could still occur if it is not used correctly ! Football Helmet Warnings • WARNING: Do not strike an opponent with any part of this helmet or face mask. This is a violation of football rules and may cause you to suffer severe brain or neck injury, including paralysis or death. Severe brain or neck injury may also occur accidentally while playing football. NO HELMET CAN PREVENT ALL SUCH INJURIES. USE THIS HELMET AT YOUR OWN RISK. Head Protection • Direct collision sports require head protection due to impacts, forces, velocities and implements • Football Helmets • Must be protective against concussive force • While helmets must be certified, they may not always be fail-safe • Athletes and parents must be aware of inherent risks Head Protection • Each helmet must have visible exterior warning label • Label indicates that helmet should not be used to strike an opponent due to risk of injury • Also indicates risk of injury accidentally and that athlete plays at own risk while using helmet • Athlete must be aware of risks and what label indicates • Athlete reads and signs statement regarding warning label • There are a number of helmet manufacturers, and even more have closed due to lawsuits and liability cases • Football Helmets are good for Football Helmet Fitting Guidelines 1. 2. 3. 4. 5. 6. 7. Helmet fits snugly around player’s head Helmet covers the base of the skull Sits two-finger widths above the eyes Ear holes should line up Cheek pads should fit snugly against the sides of the face Chin strap should be centered and prevent movement Facemask should be securely attached, about three finger widths from the nose http://www.youtube.com/watch?v=mgoS-jnmEJY Football Helmet Fitting Video Emergency Action Plans Emergency Action Plans • Emergency Action Plan (EAP) • a written document that outlines the steps to follow in case of an emergency • Emergency action plans provide guidelines and templates for documentation of emergency planning to help prepare individuals for a catastrophic injury situation within sports. • The EAP should be reviewed at least once per year with all athletic personnel along with CPR and first aid refresher training. • It is important to remember that this is a working document. • Always being modified as things change or happen Why are EAPs important? • The top causes of sudden death in sport: cardiac, head injuries, heat stroke, exertional sickling, asthma, anaphylaxis, direct trauma, lightening, and hyponatremia • 425 catastrophic injuries resulted in permanent disability injuries and 398 catastrophic injuries resulted in full recovery • 4% of sport related deaths in the US in 2013 were youth athletes under the age of 17 Components of the Emergency Action Plan 1. 2. 3. 4. 5. 6. 7. Emergency Personnel Roles of First Responder Emergency Communication Emergency Equipment Emergency Transportation Venue Directions with Map Individual Sport EAPs a. b. c. d. e. f. g. 8. 9. Practice Football Field Louis Crews Football Stadium Volleyball, Women’s Basketball, Men’s Basketball Tennis Baseball and Softball Men’s and Women’s Soccer Track/Cross Country On-Field Emergency Protocol Emergency Action Plan Checklist for non-medical emergency Essential Framework • Key Personnel • • • • • Athletic Trainers Coaches Parents Administrators Emergency Medical Services • Equipment • • • • • Keys to gates AEDs and other emergency equipment Lamination of EAP and posting First Aid kit CPR/AED Training for coaches Essential Framework • Implementation Sequence or Strategy • • • • • • • Identify what your organization does well Identify what your organization can improve upon Increase knowledge by reviewing example documents Consider who key personnel are to your organization Consider all possible venues Draft a general EAP Have several people review the EAP • Including medical personnel, EMS, coaches and parents • Create a final EAP • Post the EAP in several different locations • Revisit policy annually and revise as necessary Potential Barriers • Problems/Barriers: 1. Public fields may be hesitant to post EAPs on the fields when other people also use them. 2. No medical staff at the event 3. Too many different venues with different addresses 4. What if people don’t understand the EAP? I can’t possibly go to every person involved in our school and explain the whole thing to them! Why its Important to have an EAP • Ensure every school develops an EAP for managing serious and or potentially life-threatening injuries • Develop EAPs specifically for each venue, including appropriate contact information for EMS, facility address, location and maps and/or specific directions to that venue • Identify personnel and their responsibilities to carry out the plan of action with a designated chain of command • Develop, coordinate, include and distribute the EAP to local EMS, venue public safety officials, on-site medical personnel, staff members, health care professionals or organization administrators • Identify and list the equipment needed in an emergency situation • Specify documentation actions that need to be taken post emergency • Review and rehearse the EAP annually by all parties involved Medical Records TERMINOLOGY • Pre-Participation Physical Examination (PPE): • a checkup to evaluate a person’s health and determine if they are able to participate in sports WHY WE KEEP MEDICAL RECORDS 1. 2. 3. 4. 5. 6. Required part of an AT’s professional practice Communication purposes Legal responsibility Research ROI (Records of Information) Reimbursement FACTS • Create a detailed, chronological ‘story’ of a patient’s interaction with health care providers. • Explain why decisions were made, what care was provided, and what outcome was outcome • Help plan and evaluate treatments and monitor progress WHAT WE KEEP FOR MEDICAL RECORDS • Types: 1. Medical information forms • • • • Personal medical history Family medical history Orthopedic history Pre-participation physical examination (PPE) 2. Injury evaluation form 3. Treatment form 4. Referral form HOW WE KEEP MEDICAL RECORDS • In todays electronic era, we can keep more than “Paper” records. • Types of methods • Paper • • • • • Standardized blank forms by the school or heath care provider Standardized insurance forms “Journal –style” briefs or narratives SOAP notes Carbonless forms • Computer • Software Packages • ATS, Presagia Sports, Sim Trak, Sportsware and more • Length and Manner of storage can be an issue in both cases 10 Tips for Documenting From the Article 1. Label every page with the patient’s name and the date. 2. Indicate the date and time of each entry and sign the entry in ink, complete with your professional title. 3. Use language that is specific, objective, concise and complete. 4. When in doubt, RECORD IT. 5. Stay up-to-date on your documentation. Record entries within 24 hours of patient contact. 6. To correct an inaccurate record, make sure the original entry remains legible and clearly state why it is being changed. NEVER obliterate any part of a record. 7. Document each episode of physical medicine and rehabilitative care and treatment. 8. Maintain permanent records for every case. 9. Keep your files orderly and professional, complete, accurate and legible. 10. Use only standard English and only universally recognized medical abbreviations. If an abbreviation would allow room for confusion, do not use it. Release of Medical Records Terminology • Health Insurance Portability and Accountability Act (HIPAA): • a federal law to protect the confidentiality of an individual’s medical records • Family Educational Rights and Privacy Act (FERPA): • a law to protect the privacy of parents and students with respect to education records HIPPA • A federal law which states that an organization must follow certain privacy rules if it is a ‘covered’ entity. • A ‘covered’ entity means that the person or organization performs electronic transactions of medical records. • Most high school athletic training programs are not covered entities; however, they do exchange information with these covered entities. • AT’s must protect the information they receive. They can share it for: A. Billing purposes (Insurance companies) B. Treatment purposes (Other healthcare providers) HIPP Authorization Forms • ITEMS THAT MUST BE INCLUDED: 1. 2. 3. 4. An expiration date (usually 1 year) A statement of who the information will be released to (can be general) A statement that no one will be denied treatment for not signing A notice that authorization can be withdrawn anytime through a written statement 5. A reminder that information released to an outside entity is no longer protected FERPA • A federal law that protects the privacy interests of parents and students with regards to education records • It affects all educational institutions that accept federal funding (most high schools and universities) • It allows AT’s to share medical information with a school nurse, team doctor or other medical profession who shares responsibility for the athlete’s care FERPA Authorization Form • WHAT IS PROTECTED? 1. Files, documents or materials (including films, photographs, videos, etc.) that contain student information. Student education records (report cards, surveys and assessments & special education records) and school information about parents. Medical & health records 2. 3. • WHAT ISN’T PROTECTED? • General (‘Directory’) Information Student’s name Phone number Address Date and place of birth Honors & awards Dates of attendance Compliance with FERPA • Even though sharing of medical information is permitted through FERPA, AT’s should still have a parent sign a release to prevent legal issues! • AT’s should also make sure that the information is protected by the other health care providers. Medical Billing Terminology • Third Party Payer: • a group other than the patient (1st party) or health care provider (2nd party) that pays for health services • Health Maintenance Organization (HMO): • a health service plan that provides care for its members in a central health center • Preferred-Provider Organization (PPO): • a health service plan that allows members to choose their own physicians and hospitals within certain limits • Current Procedural Terminology (CPT): • a code from the American Medical Association that permits licensed health care providers to bill for their services • National Provider Identifier (NPI): • Healthcare providers acquire their unique 10-digit NPIs to identify themselves in a standard way throughout their industry. Third Party Reimbursement • What is: • A 1st party payer? • The patient • A 2nd party payer? • The healthcare provider • A 3rd party payer? • The insurance company • With a 3rd party payer, some or all of the patient’s healthcare services are paid for by insurance Types of Health Insurances • Exclusive Provider Organization (EPO): • A managed care plan where services are covered only if you use doctors, specialists, or hospitals in the plan’s network (except in an emergency). • Health Maintenance Organization (HMO): • A type of health insurance plan that usually limits coverage to care from doctors who work for or contract with the HMO. It generally won't cover out-of-network care except in an emergency. An HMO may require you to live or work in its service area to be eligible for coverage. HMOs often provide integrated care and focus on prevention and wellness. • Point of Service (POS): • A type of plan where you pay less if you use doctors, hospitals, and other health care providers that belong to the plan’s network. POS plans require you to get a referral from your primary care doctor in order to see a specialist. • Preferred Provider Organization (PPO): • A type of health plan where you pay less if you use providers in the plan’s network. You can use doctors, hospitals, and providers outside of the network without a referral for an additional cost. Advantages of rd 3 Party Reimbursement 1. Athletic trainers can show their value to the district by the number of treatments they provide 2. Athletic trainers can get reimbursed for the treatments they are already providing 3. The extra money coming in can be used to pay for supplies, equipment, or possibly even part of the athletic trainer’s salary Disadvantages of rd 3 Part Reimbursement 1. Some athletes don’t have insurance 2. Athletic trainers have to spend more time on paperwork, leaving them less time to help their athletes 3. Insurance companies may decide what the best care for the athlete is rather than the athletic trainer 4. An athletic trainer’s salary may depend on reimbursement