Complications During Pregnancy
advertisement

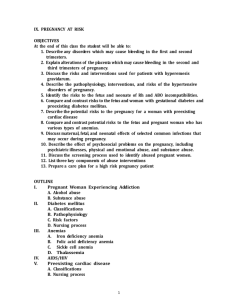
Clinical aspects of Maternal and Child Nursing Complications During Pregnancy Lectur 6 Othman Ta’ani RN-MSN Characteristic Causes of High-Risk Pregnancies Can relate to the pregnancy itself Or the woman has a medical condition or injury Or from environmental hazards that affect the mother or her fetus Or from maternal behaviors or lifestyles that have a negative effect on the mother or fetus Assessment of Fetal Health The Goal of fetal assessment Positive outcomes Nursing responsibilities Preparing the patient Explaining procedures/tests Clarifying and interpreting results Collaboration with other healthcare providers Psychosocial support Danger Signs in Pregnancy Sudden gush of fluid from the vagina Vaginal bleeding Abdominal pain Persistent vomiting Epigastric pain Edema of face and hands Severe, persistent headache Blurred vision or dizziness Chills with fever over 38.0° C (100.4° F) Painful urination or reduced urine output Pregnancy-Related Complications Hyperemesis Gravidarum Excessive Nausea and vomiting Electrolyte/acid base imbalance Significant weight loss Decreased urine output High hematocrit Treatment Correct dehydration and inadequate nutrition Nursing Care for Hyperemesis Patient Education Reduce factors that trigger nausea and vomiting Keep accurate I&O Frequent, small meals Easley digested carbohydrates Drinking liquids between meals Reduce stress Pregnancy-Related Complications Bleeding Disorders of Early Pregnancy Abortion Ectopic Pregnancy Bleeding Disorders of Late Pregnancy Placenta previa Abruptio placentae Bleeding Disorders of Early Pregnancy Abortion Spontaneous Abortion The involuntary loss of the products of conception prior to 24 weeks’ gestation Threatened Abortion Cervix is closed & no tissue is passed Inevitable Abortion Increased bleeding & cervix dilates Incomplete Abortion Bleeding tissue dilation of cervix & passage of Abortion Bleeding Disorders of Early Pregnancy (continued) Abortion Complete Passage of all products of conception, cervix closes and bleeding stops Missed Fetus dies in uterus but is not expelled, uterine growth stops and sepsis is possible Recurrent 2 or more consecutive spontaneous abortions Induced Abortions Therapeutic Abortion Intentional termination of pregnancy before age of viability to preserve the health of the mother Elective Abortion Intentional termination of pregnancy for reasons unrelated to mothers health Nursing Care of Early Pregnancy Bleeding Disorders Document amount and character of bleeding Save anything that looks like clots or tissue for evaluation by a pathologist Monitor vital signs If actively bleeding, woman should be kept NPO in case surgical intervention is needed Post-Abortion Teaching Report increased bleeding Take temperature every 8 hours for 3 days Take an oral iron supplement if prescribed Resume sexual activity as recommended by the health care provider Return to health care provider at the recommended time for a checkup and contraception information Pregnancy can occur before the first menstrual period returns after the abortion procedure Emotional Care Spiritual support from someone of the family’s choice and community support groups may help the family work through the grief of any pregnancy loss Review effective and ineffective communication techniques Effective Communication Ectopic Pregnancy 95% occur in fallopian tube Scarring or tubal deformity may result from: Hormonal abnormalities Inflammation Infection Congenital defects Ectopic Pregnancies (Continued) Manifestations Lower abdominal pain, may have light vaginal bleeding If tube ruptures: May have sudden severe lower abdominal pain Vaginal bleeding Signs of hypovolemic shock Ectopic Pregnancies (Continued) Treatment Pregnancy test Transvaginal ultrasound Laparoscopic examination Priority is to control bleeding Actions can be taken: Using medications Or by surgery to remove pregnancy from the tube Signs and Symptoms of Hypovolemic Shock Changes in fetal heart rate Rising pulse (tachycardia) Rising respiratory rate (tachypnea) Shallow, irregular respirations; air hunger Falling blood pressure (hypotension) Decreased or absent urinary output (usually less than 30 ml/hr) Pale skin or pale mucous membranes Cold, clammy skin Faintness Thirst Urinary Tract Infections Pregnancy alters self-cleaning action due to pressure on urinary structures Prevents bladder from emptying completely May develop cystitis Burning with urination Increased frequency and urgency of urination Normal or slightly elevated temperature Pyelonephritis High fever Chills Flank pain or tenderness Nausea and vomiting Effects of a High-Risk Pregnancy on the Family Disruption of usual roles Financial difficulties Delay attachment to the infant Loss of expected birth experience Postpartum complication Postpartum complications Preexisting maternal health problems contribute to many postpartum complications. Overall nursing objectives for high risk post partum clients include: a-Promote diagnosis and treatment of post partum complications to minimize risk morbidity and mortality. b- Promote comfort . c- Explore emotional aspects. d- Minimize separation of the mother and infant. e- assist the client and family to deal with anger, anxiety and fear. Nursing Process for women with postpartum complications 1- Assessment a- Health history Cardinal signs and symptoms. b- Physical examination -vital signs. -inspection. -palpation. c- laboratory and diagnostic studies. Nursing Process for women with postpartum complications 2- Nursing diagnosis. a- general diagnosis. b- complication related diagnosis. 3- Planning. 4- Implementation a- promote a full physical recovery. b- assist client and family to deal with physical and emotional stresses of postpartum complication. c-encourage parent- newborn bonding. d- provide client and family teaching. 5- outcome evaluation. 1-Postpartum hemorrhage -Postpartum hemorrhage is blood loss of more than 500 ml following the birth of a newborn. -Early post partum hemorrhage which is usually due to uterine atony, laceration or retained placenta fragments, occurs in the first 24 hours after delivery. -Late postpartum hemorrhage occurs after 24 hours after delivery and is generally caused by retained placental fragments or bleeding disorder. -Delayed uterine atony or placental fragments prevent the uterus from contracting effectively. The uterus is unable to form an effective clot structure and bleeding continues. -Nursing management includes -prevent excessive blood loss and resulting complications. -assist the client and family to deal with physical emotional stress of postpartum complications. 2- subinvolution -It is delayed return of the enlarged uterus to normal size and function. -It results from retained placental fragments and membranes, endometritis, or uterine fibroid tumor. -Uterine atony or placental fragments prevent the contracting effectively. -Clinical manifestations – prolonged lochial discharges. -irregular or excessive bleeding. -larger than normal uterus. -Nursing management 1-prevent excessive blood loss, infection, and other complications. 2-assist the client and family to deal with physical and emotional stresses of postpartum complications. 3-Puerperal infection -It is an infection developing in the birth structures after delivery. -It is a major cause of maternal morbidity and mortality. -The most common site of post partum infection is the pelvic cavity. -It can be caused by poor sterile technique, cesarean birth. -clinical manifestations: -Fever. -pain, redness, tenderness and firmness. 4- Mastitis -It is inflammation of the breast tissue that is usually caused by infection or by stasis of milk in the ducts. 5-Thrombophlebitis and thrombosis -Thrombophlebitis is an inflammation of the vascular endothelium with clot formation on the vessels wall. -A thrombus forms when blood components (platelets and fibrin) combine to form an aggregate body (clot). -Pulmonary embolism occurs when a clot traveling through the venous system lodges within the pulmonary circulation system, causing occlusion or infarction. -Predisposing factors -Hx of thrombophlebitis. -obesity. -Hx of cesarean delivery. -Maternal age older than 35 years. -Varicosities. -Anemia . -Pathophysiology -The three major causes of thrombus formation and inflammation are-venous stasis, hypercoagulable blood, and injury to innermost layer of blood vessel. The level of most coagulation factors are increased during pregnancy. A-Clinical manifestations -superficial thrombophlebitis within the saphenous vein system manifests as pain, tenderness, and warmth along the vein. -Pathophysiology -DVT symptoms include muscle pain. -Femoral thrombophlebitis generally occurring 10-14 days after delivery, produces chills, fever, stiffness, and pain. -Pulmonary embolism is heralded by sudden intense chest pain with severe dyspnea followed by tachypnea, pleuratic pain cough, tachycardia, hemoptysis, and temperature above 38 C. B-Lab. Findings. -Venography. -Doppler ultrasound. Nursing Management 1- promote resolution of symptoms and prevent the development of embolus. -Anticoagulant therapy. -It is important not to administer estrogen for lactation suppression .because it may encourage clot formation. 2- Provide client and family teaching. 3- Assist the client and family to deal with physical and emotional stresses of postpartum complications. 6- Urinary tract infection -It is indicated by more than 100 thousands bacterial colonies /ml of urine in two consecutive clean, voided, midstream specimens. -Two common types of UTIs are cystitis, inflammation of the urinary bladder, and pyelonephritis, inflammation of the renal pelvis. -Another cause of UTIs is retention and residual urine due to over distention and incomplete emptying of the bladder. - E-coli, (the most common causative organism). -Clinical manifestation -cystitis manifestations include frequency ,urgency, dysuria, hematuria, temperature elevation, and suprapubic pain. -Pyelonephritis manifestations include high fever, chills, flank pain, nausea and vomiting. -Nursing management – -recognize signs of infection and prevent the development of further complications. 7-Postartum mood disorder -The disorders are1 -Postpartum blues.-include fatigue, anxiety, mood instability, with onset 1 to 10 days postpartum and lasting 2 weeks or less. 2 -Postpartum depression without psychotic features. includes confusion, fatigue, feeling of hopelessness and shame, and alteration in mood. 3 -Postpartum depression with psychotic features (postpartum psychosis)-includes symptoms of postpartum depression plus delusion, auditory hallucinations, and hyperactivity.