Hypertension
advertisement
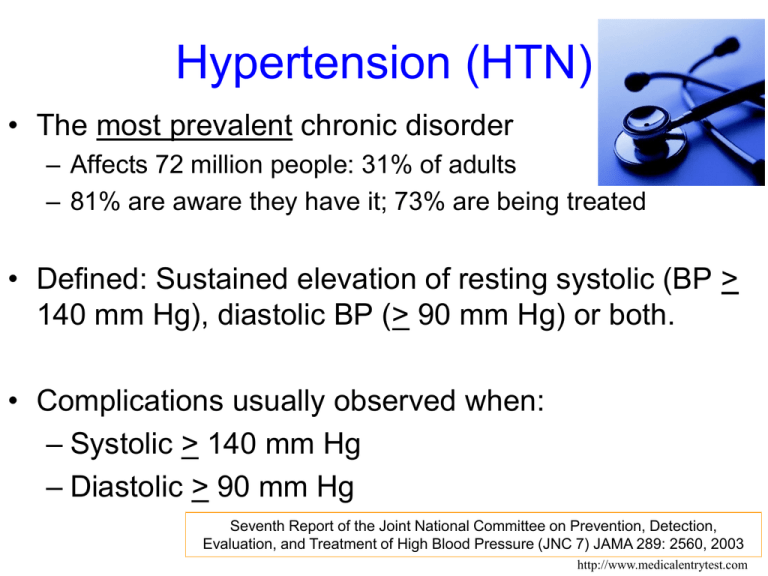
Hypertension (HTN) • The most prevalent chronic disorder – Affects 72 million people: 31% of adults – 81% are aware they have it; 73% are being treated • Defined: Sustained elevation of resting systolic (BP > 140 mm Hg), diastolic BP (> 90 mm Hg) or both. • Complications usually observed when: – Systolic > 140 mm Hg – Diastolic > 90 mm Hg Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) JAMA 289: 2560, 2003 http://www.medicalentrytest.com Objectives: Hypertension (HTN) • Write the physiological formula that describes blood pressure (BP) • Define pulse pressure • Describe the classifications of blood pressure • Identify follow-up recommendations for each classification of BP • List the non-behavioral and behavioral risk factors for hypertension. • Describe the main complications of uncontrolled hypertension. • List at least three components of the DASH diet • Identify foods high in sodium, calcium, and potassium. • Describe recommended methods for reducing high blood pressure. Overview of Hypertension (HTN) • Most prevalent chronic disease – – – – – – 31% of population (65 million with HTN; 45 m – pre-HTN) 41% of blacks (44% in black women) 50% of population > 60ys 90% of normotensive at age 55 will develop HTN Contributes to up to 75% of all strokes and heart attacks 2-3 times more common if taking OCA • Asymptomatic – Dizziness, flushed face, headache, fatigue, and nervousness are not related to hypertension Circulation 2008;117;e25-e146 -- http://circ.ahajournals.org/cgi/content/full/117/4/e25 Prevalence of HBP in adults ≥20 years of age by age and sex (NHANES: 2005–2008). 90 78.5 80 69.3 70 Percent of Population 64.0 60 54.0 66.7 53.3 50 37.1 40 30 35.2 25.1 19.0 20 11.1 10 6.8 0 20-34 35-44 45-54 55-64 65-74 75+ Age Male Female Source: NCHS and NHLBI. Hypertension is defined as SBP 140 mm Hg or DBP 90 mmHg, taking antihypertensive medication, or being told twice by a physician or other professional that one has hypertension. Roger VL et al. Published online in Circulation Dec. 15, 2010 Age-Adjusted Prevalence Trends for HBP in Adults, ≥20 years of age by race/ethnicity, sex and survey (NHANES:1988-1994, 1999-2004 and 2005-2008). 50 42.9 45 40.2 38.6 40 37.5 Percent of Population 35 41.5 38.2 30.5 28.3 28.2 30 25 26.9 27.7 25.6 26.8 25.7 24.6 22.9 25.0 25.0 20 15 10 5 0 NH White Men NH White Women NH Black Men 1988-1994 NH Black Women 1999-2004 Mexican Mexican American Men American Women 2005-2008 Source: NCHS and NHLBI. NH indicates non-Hispanic. Roger VL et al. Published online in Circulation Dec. 15, 2010 Blood Pressure Tracking BP AGE What is the Etiology? • HTN is described as either primary or secondary • Primary – 85-95% of cases (essential): – No known cause – Genetics contribute 30 – 50% • HTN nonexistent in hunter-gatherer populations – Physical activity, low fat/sodium intake, K-rich diet – Sodium retention increases blood volume – Vascular stiffness (with age) increases pressure – Weight gain increases sympathetic activity • Insulin resistance increases sympathetic stimulation • Also increases sodium retention • Secondary – Due to renal disease, connective tissue disorders, hyperthyroidism, NSAIDS, licorice, steroid use Blood Pressure: Pathophysiology • BP ≈ Q x TPR – Q = cardiac output (4-8 L/min) • Q = HR x SV (50 – 100 mL) – TPR = total peripheral vascular resistance • Abnormal Na+ transport • Sympathetic nervous stimulation – high resting heart rate may indicate this • Vasodilator deficiency rather than excess vasoconstrictor *Circulation, 1999; 100: 354-360 Diagnosis On separate occasions of at least two readings: average of seated and after standing for > 2 min on 3 separate days. • • • • Category Normal Prehypertension Hypertension, Stage 1 Hypertension, Stage 2 • • • • SBP <120 and 120-139 or 140-159 or >160 or Resources: http://www.nhlbi.nih.gov/guidelines/hypertension/index.htm Hypertension. 2005;45:142-161. * http://www.guideline.gov/summary/summary.aspx?doc_id=8326 DBP <80 80-89 90-99 >100 What recommendations should we provide? • • • • Initial BP: Normal Prehypertension Hypertension, Stage 1 Hypertension, Stage 2 • • • • Recommendation: Check in 2 yrs Recheck in 1 yr Confirm in 1 month Evaluate immediately or within 1 week http://www.nhlbi.nih.gov/guidelines/hypertension/index.htm Types of Hypertension – Primary (essential) – no identified cause • 90% of all cases – Secondary – has cause (reversible potential) • Kidney dz, sleep apnea • Medications (corticosteroids, NSAIDS, OCAs) • Alcohol, smoking, caffeine, stress – Isolated Systolic Hypertension • > 160 mm HG (atherosclerosis) – Pregnancy Induced Hypertension – White Coat Hypertension – (a possible risk factor) What are the Risk Factors for HTN? • Advanced age – lifetime risk is 90% – > 45 for men; 55 for women • Gender – men > women until age 55 then more common in women • Race – African American highest in world (41%) – Hispanic, Caucasian, Native Am same (24%) – Asian/Pacific Island (9.7%) What are the Risk Factors for HTN • • • • • • • • • • Obese (BMI > 30) High sodium intake & low potassium Diabetes Alcohol intake Physical inactivity Prehypertension Stress Low education levels Sleep apnea Family history Risk Factors (HTN) • Weight – Obesity (33% of hypertensives are overweight) • Increased visceral fat – Thin with HTN at higher risk of MI & stroke than obese with HTN – Low birth weight associated with obesity & HTN http://staciel.hubpages.com Risk Factors for HTN • Sodium Retention (salt sensitivity) – Sodium blood volume BP – Assume all are salt sensitive • Diabetes and Insulin Resistance – Occurs in thin and overweight diabetics http://www.hcgdiet.com Salt Sensitivity • Not feasible to test in most people • Factors associated with salt sensitivity: – Female – Age (increasing age increases sensitivity) – Obesity (abdominal obesity) – Alcoholism – African-American origin – Level of blood pressure • higher pressure = more sensitive – Diabetes – Positive family history http://foodandhealth.com Complications* • Stroke (or TIA’s) – 10x normal risk in hypertensive • Coronary Heart Disease / MI / Sudden Death – ½ of those with MI have HTN – Each 20/10 mmHg increase doubles MI risk • Heart Failure – Muscles thicken (left ventricular hypertrophy) – HTN factor in 75-90% of HF *Complication: a secondary disease or condition that develops as a result of the primary illness or from independent causes More HTN Complications • • • • • Atrial fibrillation Aneurysms Kidney Disease Retinopathy Bone loss – HTN increases calcium loss mayfieldclinic.com • Sexual dysfunction • Preeclampsia – complicates 10% of pregnancies • Cognitive dysfunction & dementia – short term memory loss & mental decline What about Pulse Pressure? • • • • • • • • • • • PP = SBP – DBP Pulse pressure* – change in BP when heart contracts Indicates stiffness in the aorta Indicates stretching of arteries and eventual rigidity Increases risk for aneurysms Mean Arterial Pressure = Diastolic + (1/3 x PP) BP of 170/100 is better than 170/80 Linked with CVD mortality < 50 mmHg = normal > 60 – abnormal < 25 – heart failure? *Hypertension, 1999;34:372-374 Mean Arterial Pressure (MAP) • Average arterial pressure - more accurate than SBP DBP • Better indicator of arterial perfusion of tissue/organs • Low = decreased perfusion. High = increased cardiac workload • Vasoconstriction increases MAP, vasodilation decreases • Normal MAP = 70 – 100 mm Hg • A risk factor for CVD • Formula – MAP = 1/3 (PP) + DBP Non-Pharmacological Treatment • Weight loss and exercise – Wt loss to a BMI of 18.5 – 24.9 – Exercise: 30 min/day most days • Smoking cessation • Diet: increased fruits and vegetables, decreased salt, limit alcohol – – – – DASH diet Rich in fruit and veges, reduced saturated fat Include fish and/or omega 3 fatty acid (2x/wk) Reduce sodium intake to 1500 mg/day • 1/2 teaspoon salt = 1,200 mg sodium – Alcohol < 1 oz/day in men and < 0.5 oz/day in women National Heart, Lung, and Blood Institute, National Institutes of Health. The Seventh Report of the Joint National Committee on Prevention,Detection, Evaluation, and Treatment of High Blood Pressure — Complete Report. National Heart, Lung, and Blood Institute, National Institutes of Health. NIH Publication No. 04-5230, 2004 The Salty Six www.heart.org List components of the DASH Diet • • • • • • Avoid saturated fat Select monounsaturated oil (olive, canola) Choose whole grains over white flour Choose fresh fruits and vegetables every day Include nuts, seeds and legumes every day Include calcium-rich dairy products (low or no fat) http://www.nhlbi.nih.gov/health/public/heart/hbp/dash/ Medications for HTN • Diuretics – promote water loss, remove potassium – Side effects: dizziness, fatigue, impotence, orthohypo, nausea, constipation, dry mouth – May worsen type 2 diabetes in overweight patients • Beta blockers – block actions of adrenalin – Numerous side effects • ACE Inhibitors – block action of angiotensin (a vasoconstrictor) • Calcium channel blockers – dilate peripheral arteries – decrease TPR References • Chobanian AV et al. JAMA. 2003;289:2560-2572 • Sacks FM, Svetkey LP, Vollmer WM, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension(DASH) diet. DASH-Sodium Collaborative Research Group. N Eng J Med. 2001;344:3-10. • Eckel RH, Jakicic JM, Ard JD, Hubbard VS, de Jesus JM, Lee I-M, Lichtenstein AH, Loria CM, Millen BE, Houston Miller N, Nonas CA, Sacks FM, Smith SC Jr, Svetkey LP, Wadden TW, Yanovski SZ. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2013:November 12, 2103, 10.1161/01.cir.0000437740.48606.d1