7EFTS Lifetime Limit
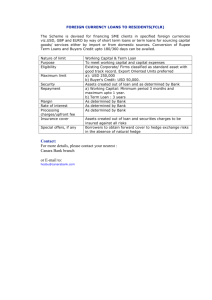
advertisement

7EFTS Lifetime Limit on access to Student Loans Position Statement Date Published: 25/02/15 Document Due for Revision: 25/02/16 Version 2 Hon. Tony Ryal www.nzmsa.org.nz New Zealand Medical Students’ Association C/- PO Box 156 Wellington 6140 New Zealand nzmsa@nzmsa.org.nz www.nzmsa.org.nz INTRODUCTION NZMSA Position Statement on the 7EFTS (equivalent full time student) lifetime limit on access to the Student Loan scheme. NZMSA POSITION NZMSA believes that the 7EFTS lifetime limit on access to the Student Loan scheme negatively impacts on equity of access to the medical degree and will reduce the retention of medical graduates, by not taking into account the length of the medical degree. The cohort of students who enter medicine via postgraduate entry (particularly students from lower socioeconomic backgrounds) or students who wish to pursue study for interest will be unfairly disadvantaged by the 7EFTS lifetime limit to the Student Loan scheme. Postgraduate-entry students (comprising approximately 25-30% of the medical student intake) have to do a minimum of eight years of study to complete a medical degree and may exhaust their EFTS before finishing medicine. Consequently, many such students, particularly those from lower socioeconomic backgrounds, may be forced to borrow from elsewhere (personal finance loans) and accrue higher levels of debt to fund their medical studies, with negative impacts on their retention rates once they graduate. NZMSA is therefore of the position that the 7EFTS lifetime limit on Student Loans will reduce the quality and standard of those studying medicine by making it more difficult for postgraduateentry students with a disproportionate effect on students from lower socioeconomic backgrounds to study medicine. NZMSA calls for targeted exemptions for medical students from the 7EFTS cap on the Student Loan scheme order to protect equity of access to the medical degree for postgraduate-entry students, particularly those students from lower socioeconomic backgrounds. This would ideally take the form of a 10EFTS cap recognizing their length of study. Additionally, NZMSA calls for formal recognition of the BMedSci (Hons) (a research year that can be undertaken during the course of the degree) as a postgraduate course for calculating progress towards EFTS caps. BACKGROUND www.nzmsa.org.nz Budget 2010/11 introduced a series of initiatives to improve the economic performance of the tertiary education sector in light of the growing cost of providing financial support to tertiary education students. One such initiative was a lifetime limit on the number of EFTS that a tertiary student studying in New Zealand could access the Student Loan scheme for tertiary fees and living costs. The 7EFTS lifetime limit on access to the Student Loan scheme took effect in January 2011, with study from 2010 academic year onwards counting toward the limit. The 7EFTS limit will affect students who enter the MBChB course in 2013 and subsequent years. This will remove loan access for these students from 2016 onwards. Key facts about the undergraduate medical degree in New Zealand: ● The undergraduate medical degree (MBChB) is five-year course with competitive entry following a “pre-med” or “health science” first year programme. ● Students who wish to do medicine after already commencing study will undertake a three year undergraduate bachelor degree, or four years with an honours degree in order to gain entry to the MBChB course via a postgraduate entry category. ● Students who enter medicine via postgraduate entry have to do a minimum of eight years of study to complete a medical degree. ● ● Approximately 20-25% of the MBChB intake each year consists of students who have gained postgraduate entry. Honours in MBChB is obtained via a one year BMedSci (Hons) programme completed in between years of medical study taking the total number of years of study to nine. KEY ISSUES FOR MEDICAL STUDENTS: ● Increased financial burden A significant financial burden will be placed on the students who exhaust their 7EFTS of access to student loans before finishing their medical degree, as they will be required to pay for both their tertiary fees and living costs without government support. A survey of medical students showed that 90% would rely on student loan to pay for their course fees. If such students were unable to source financial support from their families, they would be forced to fund their tertiary fees and living costs through work or by taking out expensive personal finance loans from elsewhere to finish their degree. This option has been discounted with refusal from banks to consider lending to students. Medical students in particular are unable to work part-time or earn a supplementary income to pay for their studies and/or living costs once they have exhausted their EFTS due to the demanding nature of the MBChB course. Specifically, the faculties of medicine from both the University www.nzmsa.org.nz of Auckland and University of Otago actively discourage medical students from working part-time during their study. ● Proportionality of the 7EFTS cap on Student Loans The 7EFTS cap on access to Student Loans does not take into account the length of the undergraduate medical degree (six years minimum for entry after the competitive first year, and eight years minimum for postgraduate-entry) in comparison to other undergraduate bachelor degrees (three years minimum). Assuming that the 7EFTS cap applies to a standard undergraduate bachelor degree (3EFTS + 4EFTS leeway), proportionality would suggest at least a 10EFTS cap for the undergraduate medical degree (6EFTS + 4EFTS leeway). Given that doctoral students (PhD) receive a 3EFTS extension to their Student Loans in addition to significant scholarship support (for living costs) due to a perceived shortage of doctoral students, medical students should also be granted an extension given the significant shortage of medical doctors in New Zealand. ● Effects of indebtedness on retention Those who exhaust their EFTS and are forced to take out expensive loans in order to complete their medical degrees will accrue higher levels of debt than those who can fund their study with government and/or family support. High levels of indebtedness are a strong driver of doctors choosing to practice medicine overseas, and have a strong influence over what vocational specialty doctors in training choose (1). ● Discrimination against Postgraduate-entry and “Other-entry” students Postgraduate-entry and other-entry students are discriminated against by the 7EFTS lifetime limit on access to Student Loans, as they have to study for a minimum of eight years to finish their medical degree. Making it more difficult for postgraduate-entry and other-entry students to study medicine may have a detrimental impact on the diversity of the medical student body. Postgraduateentry and “Other-entry” students appear to be more likely to stay in New Zealand and more likely to specialize in General Practice after graduation (2, 3). ● Discrimination against students from lower socioeconomic backgrounds www.nzmsa.org.nz Students from lower socioeconomic backgrounds are less likely to be able to rely upon family support if they exhaust their 7EFTS of access to Student Loans. Indeed, currently 50% of the University of Otago Health Professional Programme students come from the top three socioeconomic deciles, while only 3.4% come from the bottom three (4). The 7EFTS policy works to directly negate programmes that attempt to actively increase both ethnic and socioeconomic diversity of the medical school cohort. ● Deters Medical Students from following wider interests The 7EFTS policy prevents students from formalising their wider interests in the form of a qualification. For example, students wanting to do a qualification in Te Reo Maori or those relating to a hobby (such as music) are restricted from following those options. This opposes advice from the medical faculties that medical students should undertake interests outside of medicine in the interests of wellbeing and mental health. CORRESPONDENCE WITH THE GOVERNMENT ● “The cap is not in place to save money but to ensure that students make wise decisions and complete their degrees in the fastest time possible” - Medicine is a wise decision for anyone capable of attaining the grades required for entry. The 7EFTS cap is preventing people from entering Medicine, as 30% of graduate entry students know someone who was put off Medicine by the cap. Therefore, this cap is in fact preventing people from making wise decisions about their education. - Postgraduate medical students are completing their degrees in the minimum time; it takes eight or nine years. Therefore, they are not the target of this cap and should be exempt from it. - This is not a small subset of the class who are affected, as postgrad students comprise about 25% of the class. Therefore it will have a heavy impact and will not save a large amount of money. - This cap is in blatant opposition to schemes aiming to increase diversity in the class like rural entry and Pacific or Maori student entrance categories. ● “The administrative cost is too high” - There are already exemptions for postgraduate study and PhD students so it would not cost much to include Medicine students in that list www.nzmsa.org.nz - It shows a complete disregard for the stress the potential for loss of financial support causes by placing administrative costs as more important. ● “High achieving students will not be affected as they got into medicine without needing to do a degree” - Not everyone is able to enter via the first year pathway. Some students will do a year of another degree before trying to do Medicine. They are now ineligible to entry directly into Medicine and must enter via the graduate category. - Postgraduate medical students have maintained high grades over a three year period to have the grades to enter medicine and have completed their degrees in the fastest possible time to be allowed to apply for medicine. Therefore, they are also high achieving students that should be funded. - Interestingly, a student who takes seven years to do a three year degree and passes only half their papers through their degree can get student loan for the full time but a medicine student cannot. ● “Students are aware of the cap and are taking it into consideration” - 40% of post grad students from second year in Otago and Auckland were not aware of the cap until they entered medicine. These are the affected students and they do not all know about it. The government is not doing a good enough job of informing people about their changes. - 30% of post grad students from second year in Otago and Auckland know people who were put off medicine by the cap. These people are those who the class needs to increase diversity and it is tragic that financial barriers are preventing people from studying medicine. Additionally, the cap is now having a measurable negative impact on class diversity and actively working against initiatives to increase class diversity. ● “There is already a large subsidy on training medical students” - Regardless of whether medical students fund their own study or use student loan to pay for their fees the training subsidy will remain in place. - by and large the affected medical students would be using the student loan scheme to pay fees for their final year. Within twelve months of the loan being drawn the students will be practising, earning and therefore contributing repayments to their outstanding loan. REACTION TO PROPOSED ALTERNATIVE FUNDING METHODS ● TI grant www.nzmsa.org.nz - this is a $26,000 stipend through the sixth year of Medicine - Medical students will need to pay the $15,000 fees before you get any part of the grant so it is completely useless in terms of paying fees - the grant is paid as a monthly stipend so does not help with the lump sum fee payment - Does not help those who lose their loan in the fifth year of Medicine of which we know of at least 18 medical students who will have to fund two years of fees themselves (i.e. at least $30,000). ● Bank loan - NZMSA and the Minister for Tertiary Education have been to all the major banks and found that no bank is willing to loan a student with no income and no assets $20,000+ (or even $40,000+). - A bank loan requires a guarantor, which will put undue strain on students’ families from lower socioeconomic backgrounds. - A bank loan is interest bearing so this would only push students further into debt that would only increase stress in the Medical student population. ● Voluntary Bonding Scheme (VBS) - This scheme is entered into after graduation and doctors must be enrolled in it for three years before any contribution to the student loan is made. - For the above reason it is not an option for Medical students because we have to graduate before we can apply for the VBS and the first payment is after three years in the workforce. - We cannot graduate if we cannot pay for the fees for the medical programme so it can be concluded that this scheme does not help. ● Family - Students in their mid to late 20’s should not be expected to go to their parents to ask for this amount of money. - Those for whom this isn’t an option are exactly the students that we want to be encouraging into medicine, as they will be adding diversity to the profession. ● Saving - The situation is dire for those losing student loan access in sixth year but even worse for those affected in fifth year also. - Students can hope to earn between $5,000 and $6,000 realistically during work over the summer break. This is mostly needed to cover expenses for the year and saving the amounts of money we are looking at is not an option. www.nzmsa.org.nz ● “Doctors earn high wages, you’ll be alright” - We need to graduate before we can earn these high wages - The high wages at the end have no relevance to the issue of paying for the course - They do not help with getting a bank loan because banks do not take into account future income. Students are seen as ‘too much risk’ to lend money to in the opinion of the bank. NZMSA POSITION STATEMENTS No other current NZMSA positions statements relates to this particular one. REFERENCES 1. Perry WR, Wilkinson TJ. Taking the pulse: medical student workforce intentions and the impact of debt. N Z Med J. 2010 Jul 16;123(1318):15-23. 2. Shelker W, Belton A, Glue P. Academic performance and career choices of older medical students at the University of Otago. N Z Med J. 2011 Nov 25;124(1346):63-8 3. Health Workforce New Zealand. An assessment of the utility of Graduate-entry medical education Programmes for New Zealand. Ministry of Health. Mar 2011. 4. Crampton P, Weaver N, Howard A. Holding a mirror to society? The sociodemographic characteristics of the University of Otago's health professional students. N Z Med J. 2012 Sep 7;125(1361):12-28. www.nzmsa.org.nz