Clinical Case
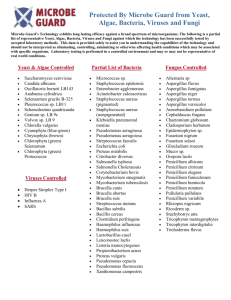
advertisement

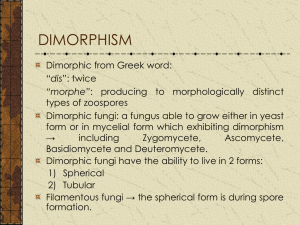
Fascinoma Rounds Penicillium marneffei October 26th, 2005 Sharmistha Mishra, Vanessa Allen, And with great thanks to Subash Mohan Case #1: Penicillium marneffei • What are the clinical risk factors for acquiring disseminated penicillium marneffei? • What are the laboratory features of this organism (courtesy of Subash Mohan)? • What precautions should be taken in the laboratory environment? Clinical Case • 32 M originally from Vietnam, no known PMH • Moved to Canada 16 years ago • Travel to Vietnam every year, – last trip in January/ February 2005 • Illness since March/April 2005 – – – – Cough, SOB and 18 lb weight loss went to family MD and to a local hospital treated for CAP with azithromycin V/Q scan negative CT scan consistent with CAP • Also had two month history of non-pruritic papular rash on face which he attributed to lobster allergy Case continued • Sept 22nd – Presented with SOB, fever, and bilateral chest infiltrates – Started on Ceftraixone and azithromycin for CAP • Laboratory values – – – – Hgb 95 (MCV 75), Leuk 4.4 (0.3 lymphs), platelets 233 Electrolyes and creatinine normal AST 113, ALT 109, ALP 100, bili 5 LDH 514 Case #3 • Bronchoscopy Sept 23rd – Positive for H. influenza – PCP – And ….Penicillium marneffei – Blood cultures from Sept 22nd became positive for Penicillium marneffei – Subsequent HIV+ , CD4 32 Discovery • 1956 bamboo rats in Vietnam • First human case = accidental innoculation in the lab (1959) from a needle • Then 1973 in pt with Hodgkin’s disease • 1985 – pt with HIV in tropical medicine course suspicion of inhalation of spores! • 1988 onwards rising # of cases in HIV+ pts from endemic areas Epidemiology • • • • Bamboo rat & association unclear Soil exposure felt to be a risk factor Inhalation, ingestion, skin puncture - postulated Geographical distribution – Thailand, Myanmar (Burma), Vietnam, Cambodia, Malaysia, northeastern India, Hong Kong, Taiwan, and southern China – Imported disease from patients from these endemic regions Clinical Risk Factors • More commonly seen in immunocompromised (also occurs in immunocompetent individuals) – 29 cases diagnosed 1959-1988 prior to HIV – Now 80% have HIV • CD4 < 70 cells/mm3 – Among HIV + pts in N. Thailand • 1. TB • 2. Cryptococcal meningitis • 3. Penicillium marneffei – Other risk factors are lymphoproliferative disorders, bronchiectasis and tuberculosis, autoimmune diseases and corticosteroid therapy Supparatpinyo K, et al.. Lancet. 1994;344:110-113. Clinical Features • Localized disease • Disseminated disease – – – – – – Fever (99%) Anemia (78%), Pronounced weight loss (76%) Generalized lymphadenopathy (58%) Hepatomegaly (51%). Skin lesions, most commonly papules with central necrotic umbilication (71%) – Pneumonia (CXR abnormalities) Penicillium marneffei Penicillium marneffei is a dimorphic fungus of RES Grows as mycelium at RT and yeast at 370C Usually attacks immunocompromised hosts P. marneffei can also attack immunocompetent hosts Reservoir – bamboo rat in south east Asia Laboratory safety precautions similar to Coccidioides Direct microscopy frequent confusion with Histoplasma Penicillium marneffei Direct Microscopy Specimen: BAL (E1232193) Stain: Fungi-Fluor x400 Structure: • small, round, oval cells • non-budding cells Compare with yeast. Rule out histoplasma. Differentiation difficult. Penicillium marneffei Direct Microscopy Specimen: BAL (E1232193) Stain: Gram stain x1000 Structure: • few oval cells • non-budding • mimic yeast Observe septum Penicillium marneffei Direct Microscopy Specimen: BAL (E1232193) Stain: KOH x400 Structure: • cluster of cells • poorly differentiated • appear non-budding Rule out yeast Interpretation difficult Penicillium marneffei Direct Microscopy Specimen: Blood Stain: Gram stain x1000 (E1221874) Structure: • • • • septate hyphae right angle branching fragmenting Arthroconidia Appear converted Observe branched pattern Not dichotomous Penicillium marneffei Direct Microscopy Specimen: Sputum Stain: GMS x1000 (E1222049) Structure: • cluster of small, round, oval cells • non-budding • bisected cells Septum rules out yeast Suspect P. marneffei A second type yeast not P. marneffei Penicillium marneffei Direct Microscopy Specimen: Sputum Stain: GMS x1000 (E1222049) Structure: • bisected cells • no budding seen • no septate hyphae • no pseudohyphae Go ahead and call it P. marneffei non-budding bisected cells Penicillium marneffei Macroscopic Morphology Medium: IMA Morphology: • rapid growth • mycelial phase • red pigment • suspect P. marneffei Not all red pigment producing Penicillium species are Penicillium marneffei Penicillium marneffei Microscopic morphology Stain: Lactophenol x400 Structures: • phialides • metulae • bi- or univerticiallate • brush type • ID: Penicillium sp. Compare with Paecilomyces Penicillium marneffei Conversion to Yeast Phase Medium: Blood agar Incubation: 370C • glabrous & matted • no mycelium • yeasty consistency • pigmentation lost Conversion phase at higher temperature is essential for confirmation DNA probe not available Penicillium marneffei Confirming conversion Wet Preparation: BA 370C Magnification: x1000 Structures: • arthroconidia • multiplies by fission • bisected cells Compare with yeast and pseudohyphae Treatment • Sensitive to Itraconazole, Ketoconazole and Ampho B • Failure rates in a study of 86 HIV-infected patients were as follows: amphotericin B , 8 of 35 patients (22.8%); itraconazole , 3 of 12 (25%); and fluconazole , 7 of 11 (63.6%) • Current recommendation – Amphotericin B, 0.6 mg/kg/day for 2 weeks, followed by itraconazole, 400 mg/day orally in two divided doses for the next 10 weeks – 97.3% effective in 74 HIV + individuals Sirisanthana T, Clin Infect Dis. 1998;26:1107-1110. Lab Safety and Penicillium marneffei • No formal guidelines • Inhalation and direct inoculation are possible mechanisms of transmission in lab.