SARS A Survival guide - Mount Sinai Hospital
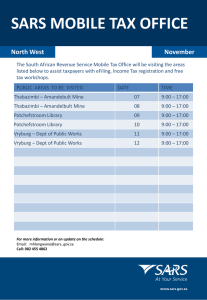
advertisement

SARS The Toronto Outbreak April 20, 2003 SARS in Toronto I: Index Case • February 23 – A 78 year old woman arrives back in Toronto from trip to Hong Kong • February 25 – Develops febrile illness with anorexia, myalgias, sore throat, cough • February 28 – Sees MD, given antibiotics • March 2 – Develops shortness of breath • March 5 – Dies at home (thought to be heart attack) SARS in Toronto 2: Spread within Household • Feb 27 - 43 year old son of index case develops febrile illness (case #2) • Admitted to Scarborough Grace March 7th, died March 13th • March 3 to 12 – all of index case’s other household contacts develop illness • 24 year old daughter in law, 5 month old grandson, 34 year old son, 79 year old husband SARS in Toronto 3: First spread outside household • March 5th – Daughter of index case, who had visited her mother while ill, develops SARS • March 9th – Family MD who saw 3 ill family members on March 6th develops SARS • March 10th, 13th – Two patients (cases #8 and #9) who spent time in ER observation area with (Case #2) on March 7/8th develop SARS SARS in Toronto 4: Spread at Scarborough Grace - I • From case #2 and ill family to 5 ICU nurses • From case #8 to two paramedics, one firefighter, four ER staff, one anaesthetist (precautions initiated in ER; no further transmission except to anaesthetist performing intubation) • From case #8’s ill wife to 7 ER visitors, one housekeeper • From case #9 (admitted before outbreak recognized) to at 20 hospital staff and students in CCU and on medical unit (nurses, MDs, support staff, radiology, pharmacy, etc.) SARS in Toronto 5: Spread at Scarborough Grace - II • Case #10 – prior exposure only to one clinic at Scar Grace; admitted 22/3 with community-acquired pneumonia – Spread to visitors and at least 2 nurses on medical unit SARS in Toronto 6: Spread to Other Hospitals • Mount Sinai Hospital – Case #10 transferred to ICU – 7 staff infected • York County Hospital – Case #9 transferred to ICU – Wife of case #9, also admitted with #hip (but had SARS as well) – 14 staff and one patient infected SARS in Toronto 7: Other Spread • Household contacts of cases – Estimated risk of unprotected exposure 24% • Doctors offices when SARS patients were present • Persons visiting SARS patients at home • Funerals of SARS patient at which family members were ill • Religious retreats • Workplace SARS in Toronto 8: Transmission “through precautions” • Two problems: 1. INTUBATION: Three episodes in Toronto hospitals (March 17 at Scar Grace, March 23 at MSH, April 10th at SBK) of transmission to all HCW in the room of patients being intubated 2. PATIENT CARE - over the last month, 6 HCW at 4 Toronto hospitals have acquired SARS despite the use of SARS precautions SARS in Toronto 9: Where are we? • Community cases remain linked to index case, but outbreak still expanding – Intensive public health effort to identify all contacts and prevent further spread • Hospital closures and precautions have substantially but incompletely reduced spread – SARS precautions enhanced April 19/20 – Intensive investigation into reasons for continuing transmission, and methods to prevent Probable and Suspect Cases of SARS in Ontario by Date of Onset (April 22, 2003 as of 9:00 a.m.) Number of Cases Suspect Probable 25 20 15 10 5 0 Apr-16 Apr-14 Source: Ontario Ministry of Health and Long Term Care, April 22, 2003 as of 9:00am Apr-12 2) Cases in epi curve includes individuals with known onset dates from all health units with reported cases Apr-10 1) Total Probable Cases = 136 (1 case with unknown onset date); Total Suspect Cases = 125(2 cases with unknown onset date) Apr-08 Apr-06 Apr-04 Apr-02 Mar-31 Mar-29 Mar-27 Mar-25 Mar-23 Mar-21 Mar-19 Mar-17 Mar-15 Mar-13 Mar-11 Mar-09 Mar-07 Mar-05 Mar-03 Mar-01 Feb-27 Feb-25 Feb-23 Date of Onset Notes: Severe Acute Respiratory Syndrome (SARS) Toronto (21/04/03) Exposure No. (%) Healthcare worker 95 (36) Nosocomial patient or visitor 49 (19) Household contact 77 (29) Travel 12 (5) Under investigation 28 (11) Severe Acute Respiratory Syndrome (SARS) Case-Fatality Age (yrs) No. cases No. (%) deaths <18 17 0 18-35 68 0 36-64 128 3 (2.3) 65 45 11 (24.4) Total 258 14 (5.4) SARS in Toronto 10: What have we learned? • Cases of SARS that are not suspected pose the greatest danger to staff – High index of suspicion and SARS isolation for febrile patients best protection • Ill visitors can spread the disease in the hospital to staff and patients – Visitor restrictions essential until outbreak is over SARS in Toronto 11: What have we learned? • Early detection of infection vital so that precautions can be used to prevent spread – Fever surveillance in patients and staff critical to ensuring that transmission is stopped • Infection control precautions are effective, but require very careful attention to detail to be most effective – Intensive investigation into how to enhance precautions effectively is underway SARS in Toronto 12: What have we learned? • Intubation, and potentially other coughinducing procedures in the ICU, poses special risks from some, but not all patients – Enhanced precautions being implemented in ICUs for such procedures • Some patients much more infectious than others – No means to identify these patients currently; many investigations underway