BCH 450 Biochemistry of specialized Tissues( Kidney
advertisement

BCH 450 Biochemistry of
Specialized Tissues( Kidney)
Dr. Samina Hyder Haq
Dept of Biochemistry
King Saud University
Kidney structure and
Function
Location: Retroperitonial
Blood Flow: Renal artey &renal vein
Cardiac output: 25%
Function:
1. Filter wastes such as urea and
ammonium.
2. Regulates electrolyte balance,
acid base balance and blood
pressure
3. The production of hormones
including vitamin D, renin and
erythropoietin
Anatomical Location and Gross
Structure
Kidney Cross section
How the Kidney Works
Nephron The functional unit of Kidney
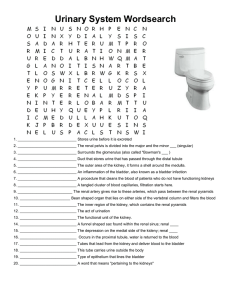
Key words
1.
2.
3.
4.
5.
Glomerulus: dense mass of very fine blood
capillaries at thenephron that act as a filter
Bowman’s capusle:cup-shaped part of the nephron
that holds a glomerulus and collects the products
of filtration from it
Glomerular filtrate:
liquid removed from the
blood by filtration in the kidney
An afferent arteriole delivers blood to a
glomerulus
Efferent arterioles :The blood leaves the
glomerulus through it.
Formation of urine
The three processes of urine formation
1) glomerular filtration,
2) tubular reabsorbt ion and
3) tubular secretion.
Glomerular filteration
1.
Glomerulus brings a large surface
area of blood capillaries in close
contact with Bowman’s capsule
2.
Liquid filtered from blood under
pressure (filtration)
3.
Glomerular filtrate produced
containing:
-water
-glucose
-salts
-urea
(Protein molecules and red blood
cells do not pass into tubule as
they are TOO BIG!!!!)
Tubuler Reabsorbion
A lot of substance needs to
be reabsorbed such as
water, glucose and some
salts.
Final urine contains
Water
Waste urea
Unneeded salts
Glucose
reabsorbed
More water
absorbed
Variable amounts of water and
salts reabsorbed and filtrate
gradually turning into urine
Summary of tubuler reabsorbtion
Tubular secretion
Urine formation is completed as the fluid passes
from the proximal tubule flows through the loop of
henle and distal tubules where the cells through
special mechanism reabsorb most of water,
electrolytes
The reabsorbtion of various electrolytes are under
the control of adrenal cortical hormones, aldostrane,
deoxycorticosterone
The reabsorbtion at distal tubule also under the
control of antidiuretic hormone, vasopressin
Kidney act as a homeostatic organ
Histology of kidney
Hormones controlling water absorption
Water reabsorption is controlled by the antidiuretic hormone
(ADH) in negative feedback. ADH is released from the pituitary
gland in the brain. Dropping levels of fluid in the blood signal the
hypothalamus to cause the pituitary to release ADH into the blood.
ADH acts to increase water absorption in the kidneys. This puts
more water back in the blood, increasing the concentration of the
urine. When too much fluid is present in the blood, sensors in the
heart signal the hypothalamus to cause a reduction of the amounts
of ADH in the blood. This increases the amount of water absorbed
by the kidneys, producing large quantities of a more dilute urine.
Aldosterone a hormone secreted by the kidneys, regulates the
transfer of sodium from the nephron to the blood. When sodium
levels in the blood fall, aldosterone is released into the blood,
causing more sodium to pass from the nephron to the blood. This
causes water to flow into the blood by osmosis.
Other hormones secreted by kidney
1.
Human kidney secretes
Calciteriol:Calcitriol acts on the cells of the intestine to promote
the absorption of calcium from food and bone to mobilize calcium from
the bone to the blood
2.
Erythropoitin:Erythropoietin is a glycoprotein. It acts on
the bone marrow to increase the production of red blood
cells.
3.
Renin:
Renin
One of the functions of the kidney is to monitor blood
pressure and take corrective action if it should drop.
Renin acts on angiotensinogen, a plasma peptide, splitting off a fragment containing
10 amino acids called angiotensin I.
angiotensin I is cleaved by a peptidase secreted by blood vessels called angiotensin
converting enzyme(ACE) — producing angiotensin II, which contains 8 amino
acids. angiotensin II
constricts the walls of arterioles closing down capillary beds.
stimulates the proximal tubules in the kidney to reabsorb sodium ions;
stimulates the adrenal cortex to release aldosterone. Aldosterone causes the
kidneys to reclaim still more sodium and thus water .
increases the strength of the heartbeat;
stimulates the pituitary to release the vasopressin.
All of these actions lead to an increase in blood pressure
Action of renin
Kidney clearance
As the blood containing waste passes through the kidneys, a
certain proportion of these substances is removed per unit
time.
Kidney clearance of a substance excreted in the urine in one
minute.
Plasma rather than whole blood clearance are determined
C = UV/P
U =the conc of substance per milliliter of urine
V= themilliliter of urine secreted per minute
P= the conc of substance per milliliter of plasma.
The polysaccharide inulin Mw 5000 is most commonly used
determination of glomeruler filtration
Kidney Clearance
The clearance of many substances such as Na+,
K+,HCO3,Cl,SO4. HPO4. amino acid glucose, uric acid and
ascorbic acid show clearance less than inulin are reabsorbed by
the tubules.
There are no of substances which have clearance greater than
inulin which means that these substances are secreted into tubular
fluid by the tubular cells
Renal Clearance: If a substance is not reabsorbed or secreted,
then the amount excreted = amount filtered
Quantity excreted (mg/min) = V x U
V = rate of urine formation;
U = inulin concentration in urine
Renal Threshold Tm
Tm represent the maximum rate at which the tubule
can reabsorb or excrete a substance. At normal
blood sugar level 100mm/100ml of plasma. Urine
contains essentially no glucose
The amount appearing in the urine per minute when
the plasma level exceeds the excretory capacity
represent the excretory Tm.
Similarly various substances such as glucose,
ascorbic acid, Na, Cl do not appear in urine until
their plasma concentration rise to certain values
called threshold substances
Tubular Function
The quantity of glomerular fluid formed in the kidney is enormously
greater than the amt of urine excreted due to reabsorbtion of most of
the water as the fluid passes the tubules
The solute concentration in plasma and glomerular fluid is normally
around 0.3osmolar/litter in urine the solute concentration may rise to
1.4osmolar/litter
The pH of glomerular filtrate is about the same as that of plasma and
filtrate as 7.4
As the glomerular filtrate passes through the proximal tubule 8085%of the electrolyte Na, k, Cl, HCo3, HPO4, SO4. practically all of
glucose, amino acid and ascorbic acids are reabsorbed.
125ml of glomerular filtrate passing through the proximal tubule
only some 20-25ml reaches the loop of Henley and distal tubule.
About 80% of water is absorbed into the plasma by the proximal
tubules 20% passes to the distal tubule.
Kidney as acid-base balance
The acid –base balance of the body is concerned with the
metabolism of H ions or protons their excretion and
handling pH7.4
Normal urine normally is slightly acidic because the kidneys
reabsorb almost all HC03-and excrete H+.
The chief acids are H2CO3,HHb, HHb,HHbO2, protein,HPO4
Proton added to body fluids are taken by the buffer basis(anions)to
form the buffer acids when there is deficiency they are given to body
fluid by the buffer acid H+ buffer bases __H+ increases
Buffer acids _H +decreases_
Kidney regulates {H+}
The total cation equivalence to the total anions in your plasma
Acid base Balance
1.
2.
3.
A buffer is a mixture of a weak acid and a
salt of its conjugate base that resist changes
in pH. No of buffer system in our body
HCO3/CO3 acid buffer system
Phosphate buffer system
Plasma protein and haemoglobin buffer
system
Renal Buffer
Renal excretion of acid and conservation of
HCO3 occur through several mechanism
1. The Na H+exchange
2. Production of ammonia and excretion of
NH4
3. Reclamation of bicarbonate
Na+ H+ exchange
All mammalian cells contain ATP-hydrolyzing
protein capable of exchanging Na+ions for protons
the so called Na,H exchanger,
In renal tubules the exchanger extrudes H ions into
the tubular fluid in exchange for Na ions.it enhances
in estate of acidosis and inhibited in alkalotic states.
The proximal tubule cannot maintain an H gradient
of more than pH=1,wheras the distal tubules cannot
maintain more than pH=3max acidity =4.4
K ions compete with H in the renal tubular Na,-H+
exchanger.
Renal production of ammonia and
excretion of ammonium ions
Renal tubular cells are able to generate ammonia from glutamine and
other amino acids derived from muscles and liver cells.
L-Glutamine + H2O glutaminase L-Glutamate + NH4.............(reaction 1)
Glutamate + NH3 + ATP
(Glutamine synthetase) Glutamine + ADP + Pi.......(reaction 2)
NH4 + 2-oxoglutarate + NADPH glutamate dehydrogenase
NH4
L-glutamate + NADP+ H2O.....(reaction 3)
NH3 + H
NH4 ions transported to tubular lumen without dissociation in NH3 and
H. At normal pH the ratio of NH3 to NH4 is about 1 to 100. NH3 is a
gas diffuses quickly through the cell membrane into the tubular
lumen where it combines with H to form NH4 . In individual with
critical acidosis NH3 production is not achieved to buffer the nonvolatile acids.
H+ secreted by Na+ H+ exchanger may react with
HPO4. to form H2PO4 . In renal disease less
excretion of H2PO4
Strong acids like sulfuric,hydrochloric and
phosphoric ionized freely at pH of urine and
excreted only when H reacts with the buffer base,
excretion of these anions is accompanied by
simultaneous removal of cations Na, k, NH+ to
provide electrolytic balance.
Reclamation of filtered bicarbonate. For each H+
secreted into the tubular fluid one Na+ and one
HCO3 absorbed. When concentration exceed
26mmol it is excreted out.
In increase acidosis of proximal tube, urine CO2
increases and HCO3 decreases
Ammonia Toxicity
Brain tissue very sensitive to ammonia. High conc
of ammonia causes Coma. Cells get rid of ammonia
by Reaction 2
High concentration of ammonia shifts the reaction
towards glutamine, Glutamine synthetase uses
ATP, this depletes the brain cell of ATP hence
essential for vital function
Glutamate is a precursor of GABA. High
concentration of ammonia deplete glutamate, in turn
deplete GABA which is a basic neurotransmitter.
Conditions associated with
abnormal Acid base balance
Metabolic acidosis
Metabolic alkalosis
Respiratory acidosis
Respiratory alkalosis