Injection
advertisement

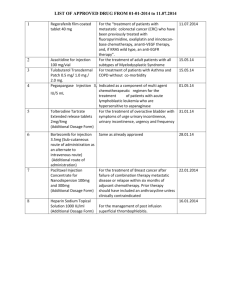
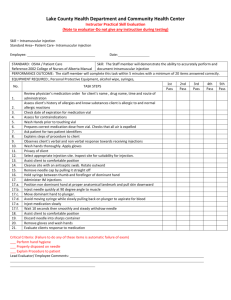
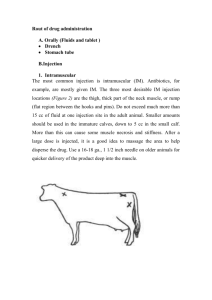
DRUG’S ADMINISTRATION 2015 Anna Molnár Route of administration • The path by which a drug is taken into the body. Route of administration • Routes of administration are generally classified by the location at which the substance is applied ( e.g. oral,intravenous …). • Routes can also be classified based on where the target of action is. – topical (local), – enteral (system-wide effect, but delivered through the GI tract), – parenteral (systemic action, but delivered by routes other than the GI tract). Route of administration Topical • epicutaneous (application onto the skin), e.g. allergy testing, typical local anesthesia (LA) • inhalational, e.g. asthma medications • enema, e.g. contrast media for imaging of the bowel • eye drops (on the conjunctiva), e.g. antibiotics • ear drops • through mucous membranes in the body (LA) Route of administration Enteral • Involves any part of the gastrointestinal and has systemic effects: – By mouth (orally), many drugs as tablets, capsules, or drops – By feeding tube ( drugs and enteral nutrition) – Rectally :various drugs in suppository Route of administration Parenteral • Subcutaneous (under the skin) • Intra-muscular • Intravenous (into a vein), e.g. many drugs, total parenteral nutrition • Intra-arterial (into an artery), e.g. thombolytic drugs for treatment of embolism • Intracerebroventricular (into cerebral ventricular system) • Intrathecal (an injection into the spinal canal) Route of administration Parenteral (cont.) • intraosseous infusion (into the bone marrow) is, in effect, an indirect intravenous access because the bone marrow drains directly into the venous system. This route is occasionally used for drugs and fluids in emergency medicine and pediatrics when intravenous access is difficult. Choice of route Depends on: • Available forms of any given drug. • Advantages and disadvantages of administration. • Urgency (patient actual clinical situation) • Patient preferences Choice of route advantages • generally the most convenient • low cost Oral disadvantages • Gastrointestinal tract irritation • Delayed effect • Time-release formulations, breaking the tablets or capsules can lead to more rapid delivery of the drug than intended. Route of administration Parenteral – Injection • Encompasses intravenous (IV), intramuscular (IM), and subcutaneous (SC) administration. • Injections act rapidly, with onset of action – in 15-30 seconds for IV, – 10-20 minutes for IM, – 15-30 minutes for SC. Route of administration Parenteral – Injection • Advantages: – 100% bioavailability, – can be used for drugs that are poorly absorbed or ineffective when given orally. – Some drugs (e.g. anitpsychotics) can be administered as long-acting intramuscular injections – Ongoing IV infusions: deliver continuous medication or fluids. Route of administration Parenteral – Injection • Disadvantages: – potential pain or discomfort for the patient, – requirement of trained staff using aseptic techniques for administration, – risk of overdose, – increased risk of side effects. Uses of routes • Topical or systemic purpose e.g. through inhalation: inhalation of asthma drugs is targeted at the airways (topical effect), whereas inhalation of volatile anesthetics is targeted at the brain (systemic effect). • Identical drugs can produce different results depending on the route of administration. (e.g. Naloxon IV/ PO).. Uses of routes • In acute situations, in emergency medicine and intensive care medicine, drugs are most often given intravenously. – reliable route, as in acutely ill patients the absorption of substances from the tissues and from the digestive tract can often be unpredictable due to altered blood flow or bowel motility The injections General rules: Before injection the skin must be disinfected carefully The air must be removed from the syringe After an ampoule is opened, the drug most be utilized in a short time When the drug is sucked out, the needle must not touch the outside of the ampoule When the drug is sucked out, change the needle before administration In case of powder vials the diluent is first added to the vial, the vial is shaken and the solution is sucked into the syringe The drug must be checked carefully before administration! (Once you have injected a solution, it cannot be removed!) The injections Intracutaneous injection: - This is administered to layers of the skin - Aim: allergy testing, tuberculosis screening - A tuberculin type syringe and thin needle are used - The needle should be inserted at an angle of 10-20o - Sites: inner forearm, posterior of upper arm The injections Subcutaneous injection - This is administered into the fat or connective tissue underlying the skin (insulin and heparin) - Thin needle is applied - The skin should be gently pinched into a fold to elevate the sc. tissue. The injection should be given at an angle of 45o into the raised skin fold - Sites: external upper third of the upper arm, abdomen, external medial area of the thigh The injections Intramuscular injection - This is used for the injection of a larger volume (max. 5 ml) - The needle should be inserted at an angle of 90o - The skin should be stretched - Sites: gluteal muscle, (borders: anterior superior iliac spine and the iliac crest) in adults - lateral side of the femoral muscle (above the medial third of the femur) in children - Contraindicated for patients treated with anticoagulants The injections Intravenous injection: - Fast effect - Use a tourniquet; the vein must be punctured at an angle of 30-45o - Once the needle is in place, it is helpful to draw blood - Torniquet is released and injection is given slowly - Sites: v. mediana cubiti, v. cephalica, dorsal veins of hand, foot Intravenous injection Central venous catheter insertion Medication safety and errors • One of the recommendations to reduce medication errors and harm is to use the “five rights”: 1.the right patient, 2.the right drug, 3.the right dose, 4.the right route, 5.the right time. Medication safety and errors • When a medication error does occur during the administration of a medication, we are quick to blame the nurse and accuse her/him of not completing the five rights. The five rights should be accepted as a goal of the medication process not the “be all and end all” of medication safety. Adverse drug reaction • “an appreciably harmful or unpleasant reaction, resulting from an intervention related to the use of a medicinal product, which predicts hazard from future administration and warrants prevention or specific treatment, or alteration of the dosage regimen, or withdrawal of the product.” Adverse drug reaction • WHO's Adverse Reaction Terminology (with mnemonics): 1. 2. 3. 4. 5. 6. dose-related (Augmented), non-dose-related (Bizarre), dose-related and time-related (Chronic), time-related (Delayed), withdrawal (End of use), and failure of therapy (Failure). Adverse drug reaction • Management: – withdrawal of the drug if possible – specific treatment of its effects. Suspected adverse drug reactions should be reported. Adverse drug reaction • Seriousness and severity (FDA) – – – – Death Life-threatening (e.g. anaphylactic) Hospitalization (initial or prolonged) Disability – change in the patient's body function/structure, physical activities or quality of life. – Congenital anomaly – Requires intervention to prevent permanent impairment or damage Vancomycin (antibiotic) iv to drug allergic pt Thanks for your attention!