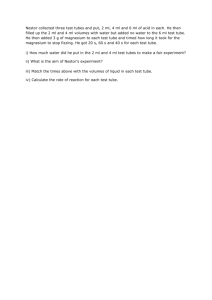
OCR Document - Eclipse Aesthetics
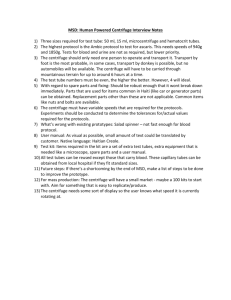
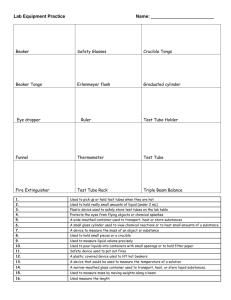
advertisement

PPT-I Platelet Preparation System INTENDED USE Safe and rapid preparation of autologous platelet-rich plasma (PRP) from a small sample of blood at the patient point of care. The PRP is mixed with autograft and/or allograft bone prior to application to a bony defect for improving handling characteristics. 6. Needle disposal container for used needle or needle/holder combination 7. 2-5ml or 10 ml Syringes 8. 2 Blunt needles or 1 sharp needle 9. Optional: filter sleeve REQUIRED EQUIPMENT NOT PROVIDED FOR SPECIMEN PROCESSING 1. Centrifuge capable of generating 1200 G (RCF) (spun for 12 minutes) or 1500 G (RCF) (spun for 10 minutes) at the tube bottom. A horizontal centrifuge head is preferred for barrier quality with Gel Tubes. . PREPARATION FOR SPECIMEN COLLECTION Be sure the following materials are readily accessible before performing venipuncture: 1. See required equipment above. 2. Tubes. PRODUCT DESCRIPTION Vacuum tube for Platelet Rich Plasma (PRP) preparation with gel and anticoagulant. LIMITATIONS OF SYSTEM The quantity of blood draw varies with altitude, ambient temperature, barometric pressure, tube age, venous pressure, and filling technique. Tubes with draw volume smaller than the apparent dimensions indicated may be filled more slowly than tubes of the same size with greater draw volume. For those tubes subjected to centrifugation to generate plasma or serum for testing, standard processing conditions do not completely sediment all cells, whether or not barrier gel is present. NOTE: FOR SINGLE USE ONLY. Discard the entire platelet separation tube after a single use by an acceptable disposable method for devices potentially contaminated with blood products. PRECAUTIONS 1. PRP should be applied to the same patient whom the blood was drawn from!!! 2. Storage of tubes containing blood at or below 0°C may result in tube breakage. 3. Storage of tubes above 40°C may damage the gel stability. 4. Do not remove conventional rubber stoppers by rolling with a thumb. Remove stoppers with a twist and pull motion. 5. Do not use tubes if foreign matter is present. 6. All liquid preservatives and anticoagulants are clear. Do not use tubes after their expiration date. 7. Do not re-sterilize and do not attempt to clean this product. 8. Do not use products if pouch is damaged. 9. Use prepared platelet concentrate material within 4 hours after drawing blood from patient. CAUTION 1. Practice Universal Precautions. Process all procedures under controlled environment, use gloves, gowns, eye protection, other personal protective equipment and engineering controls to protect from blood splatter, blood leakage and potential exposure to blood-borne pathogens. 2. All glass has the potential for breakage. Examine all glass for potential damage in transit before use and take precautionary measures during handling. 3. Handle all biologic samples and blood collection "sharps" (lancets, needles, luer adapters, and blood collection sets) according to the policies and procedures of your facility. Obtain appropriate medical attention in the event of any exposure to biologic samples (for example, through a puncture injury) since they may transmit viral hepatitis, HIV (AIDS), or other infectious diseases. Utilize any built-in used needle protector, if the blood collection device provides one. Estar Technologies Ltd. does not recommend reshielding used needles. 4. Discard all blood collection "sharps" in biohazard containers approved for their disposal. 5. Transferring a sample from a syringe to a tube is not recommended. Additional manipulation of sharps increases the potential for needlestick injury, in addition, depressing syringe plunger during transfer can create a positive pressure, forcefully displacing the stopper and sample and causing a potential blood exposure. Using a syringe for blood transfer may also cause over or underfilling of tubes, resulting in an incorrect blood-to-additive ratio and potentially incorrect analytic results. Tubes with draw volume smaller than the apparent indicated dimensions may not be filled to their stated volume when filled from a syringe. The laboratory should be consulted regarding the use of these samples. 6. Underfilling of tubes will result in an incorrect blood-to-additive ratio and may lead to incorrect analytic results or poor product performance. POSSIBLE ADVERSE EFFECTS 1. Damage to blood vessels, hematoma, infection and/or irritation. 2. Temporary or permanent nerve damage that may result in pain or numbness. 3. As with any injection-based treatment, infection is a slight possibility. STORAGE Store tubes at 4-25°C (39-77°F), unless otherwise noted on the package label. SPECIMEN COLLECTION AND HANDLING Read this entire circular before performing venipuncture. REQUIRED ACCESSORIES 1. Practice Universal Precautions. Use gloves, eye protection, coats or gowns, and other appropriate apparel for protection from exposure to blood-borne pathogens or other potentially infectious materials 2. Holder, Luer Adapter and PSV Set (our vacu10 or other available devices for venous blood collection via vacuum) 3. Alcohol swab for cleansing site 4. Dry sterile gauze 5. Tourniquet Version 15-US, 03.01.15 PREVENTION OF BACKFLOW Since the evacuated blood collection tubes contain chemical additives, it is important to avoid possible backflow from the tube, with the possibility of adverse patient reactions. To guard against backflow, observe the following precautions: 1. Place patient's arm in a downward position. 2. Hold tube with the stopper uppermost. 3. Release tourniquet as soon as blood starts to flow into the tube. 4. Make sure tube additives do not touch stopper or end of the needle during venipuncture. VENIPUNCTURE TECHNIQUE AND SPECIMEN COLLECTION GENERAL INSTRUCTIONS WEAR GLOVES DURING VENIPUNCTURE AND WHEN HANDLING BLOOD COLLECTION TUBES TO MINIMIZE EXPOSURE HAZARD. 1. Select a PPT-I tube. 2. Gently tap tubes containing additives to dislodge any material that may be adhered to the stopper. 3. Place tube into holder. Note: Do not puncture stopper. 4. Select site for venipuncture. 5. Apply tourniquet. Prepare venipuncture site with an appropriate antiseptic. DO NOT PALPATE VENIPUNCTURE AREA AFTER CLEANSING. 6. Place patient's arm in a downward position. 7. Remove needle shield. Perform venipuncture WITH ARM DOWNWARD AND TUBE STOPPER UPPERMOST. 8. Push tube onto needle, puncturing stopper diaphragm. Center tubes in holder when penetrating the stopper to prevent sidewall penetration and resultant premature vacuum loss. 9. REMOVE TOURNIQUET AS SOON AS BLOOD APPEARS IN TUBE. DO NOT ALLOW CONTENTS OF TUBE TO CONTACT THE STOPPER OR END OF THE NEEDLE DURING PROCEDURE. Note: Blood may occasionally leak from the needle sleeve. Practice Universal Precautions to minimize exposure hazard. If no blood flows into tube or if blood ceases to flow before an adequate specimen is collected, the following steps are suggested to complete satisfactory collection: a. Push the tube forward until tube stopper has been penetrated, if necessary, hold in place to ensure complete vacuum draw. b. Confirm correct position of needle cannula in vein. c. If second tube does not draw, remove needle and discard. Repeat procedure from Step 1. 10. Once the tube has been filled to its stated volume and blood flow ceases, remove the tube from holder. 11. Remove needle from vein, applying pressure to puncture site with dry sterile swab until bleeding stops. 12. Once clotting has occurred, apply bandage if desired. 13. After venipuncture, the top of the stopper may contain residual blood. Take proper precautions when handling tubes to avoid contact with this blood. Any needle holder that becomes contaminated with blood is considered hazardous and should be decontaminated with bleach or disposed of. 14. Dispose of the used needle using an appropriate disposal device. DO NOT RESHIELD. Reshielding of needles increases the risk of needlestick injury and blood exposure. 15. Turn the filled tube upside-down and return it to an upright position. That is one complete inversion. 16. For proper additive performance, invert tube 5 times. Do not shake. Vigorous mixing may cause foaming or hemolysis. In tubes with anticoagulants, inadequate mixing may result in platelet clumping, clotting and/or incorrect test results. CENTRIFUGATION Caution: Do not centrifuge glass tubes at forces above 1550 RCF in a horizontal head (swinging bucket) centrifuge as breakage may occur. Follow manufacturer instruction when using centrifuge. Glass tubes may break if centrifuged above 1550 RCF in fixed angle centrifuge heads. Use of tubes with cracks or chips or excessive centrifugation speed may cause tube breakage, with release of sample, droplets, and aerosols into the centrifuge bowl. Release of these potentially hazardous materials can be avoided by using specially designed sealed containers in which tubes are held during centrifugation. Centrifuge carriers and Inserts should be of the size specific to the tubes used. Use of carriers too large or too small may result in breakage. Ensure that tubes are properly seated in the centrifuge carrier. Incomplete seating could result in separation of the stopper closure from the tube or extension of the tube above the carrier. Tubes extending above the carrier could be caught on centrifuge head, resulting in breakage. Balance tubes to minimize the chance of glass breakage. Always allow centrifuge to come to a complete stop before attempting to remove tubes. When centrifuge head has stopped, open the lid and examine for possible broken tubes. If breakage is indicated, use mechanical device, such as forceps or hemostat to remove tubes. Caution: Do not remove broken tubes by hand. See centrifuge instruction manual for disinfection instructions. RCF is related to centrifuge speed setting (rpm) using either of the following equations: rpm RCFx10 1.12 xr 5 or approximately rpm r CENTRIFUGATION SPEED AND TIME RCF(g) TIME (min) PPT-I Vacuum Tube – Model 614B 1200 PPT-I Vacuum Tube – Model 642VES 1496 Choose Speed and Time based on Centrifuge RCF = Relative Centrifugal Force, g' 12 10 Authorized Representative in the European Community Caution, consult accompanying documents Keep away from sunlight Keep dry Temperature limitation Fragile, Handle with care Do not Use if Package is Damaged CENTRIFUGE RADIUS I SPEED SPEED (rpm) RADIUS (cm) SPEED (rpm) 7 3750 17 2400 8 3500 18 2350 9 3300 19 2280 10 3150 20 2200 11 3000 21 2160 12 2900 22 2100 13 2750 23 2060 14 2650 24 2030 15 2550 25 2000 16 2500 26 1950 1. After centrifugation remove cap from tube. 2. Invert the PRP tube gently 6 to 7 times. 3. Removal of PPP phase. Place the tube in the rack. Attach the 10 cm blunt needle to 10 ml syringe. Open the tube and place the cap upside down on a sterile surface (to maintain sterility). Insert 10 cm needle until you reach the surface of plasma. Then carefully draw plasma from the surface for about 50% to 80%, leaving 1.5 to 3.5 ml in the tube. You are now removing the PPP phase. Do not insert the needle too deep from the surface of plasma. After drawing PPP into the syringe, discard this PPP. 4. PRP harvesting: Using the same 10 ml syringe with 10 cm blunt needle, you will reach the remaining plasma. You are now handling PRP. Suspend the PRP fraction by gently mixing it through pumping up and down the fluid against the gel surface and around the tube wall to lift platelet on the gel surface. Carefully repeat this process 3 to 4 times. Alternatively, close the tube by re-placing the cap and invert it 10 times. This is a very important process to harvest as many platelets as possible. The PRP is now ready for use. 5. Optional: place the tube in the rack. Take the sleeve filter, peel sterile cover to a half way from filter side to expose bottom side of sleeve. Hold cap with sterile cover on and insert filter into the tube until filter gently touches the gel surface. PRP now enters inside the sleeve chamber. Insert a new 10 cm blunt needle into the sleeve chamber through MonoCap® hole to collect the PRP. The PRP is now ready to use. CAUTION: Federal law (USA) restricts this device to sell by or on the order of a physician. It is the laboratory's ultimate responsibility to determine reference intervals for all analytes based upon the tubes used for sample collection by that laboratory. The clinical laboratory should establish/verify its reference ranges if changing specimen collection tube types and sizes, as this could potentially affect analytic results from patient samples. Catalog Number FDA cleared 510(k) Class II medical device. Eclipse PRP is intended for the safe and rapid preparation of autologous platelet-rich plasma (PRP) from a small sample of blood at the patient point of care. The PRP is mixed with autograft or allograft bone prior to application to an orthopedic surgical site. 510(k) number: BK110035 Estar Technologies Ltd., 15, Hamerkava St. Holon, Israel 5885111 Tel: +972-3-5596414/35/36, Fax: +972-3-5596424 E-mail: aaron@estar-medical.com BALANCE PRP SEPARATION REF Federal (USA) law restricts this device to sale by or on the order of a physician The flow properties of the barrier material are temperature-related. Flow may be impeded if chilled before or during centrifugation. Gel separation tubes should be centrifuged no later than 2 hours after collection. Tubes should not be recentrifuged once barrier has formed. Barriers are more stable when tubes are spun in centrifuges with horizontal (swinging bucket) heads than those with fixed angle heads. When processing odd number of PPT-I tubes place filled contra balance tube with the same weight directly opposite from the platelet preparation tube in the centrifuge. When processing even number of PPT-I tubes, place tubes directly opposite from each other in the centrifuge. Manufacturer Do not re-sterilize Latex Free RADIUS (cm) Version 15-US, 03.01.15 Do not reuse Use by Recyclable package The following table relates radius of centrifuge arm to required speed in order to obtain the appropriate g-force. Footnotes PRP - Platelet Rich Plasma PPP – Platelet Poor Plasma Symbols & Mark Key Method of Sterilization Using Irradiation 10,000 where "r", expressed in cm, is the radial distance from the center of the centrifuge head to the bottom of the tube. The following table gives recommended centrifuge speed and time. PRODUCT Batch Code Manufactured for: Eclipse Aesthetics, LLC 13988 Diplomat Dr., Suite 160 Dallas TX 75234 Tel: 800-759-6876 Fax: 866-558-0415 E-mail: info@eclipsemed.com Version 15-US, 03.01.15