Newborn Complications Definition Flow Diagrams

Specifications for Unexpected Newborn
Complications (UNC) v2.3
• Introduction/ Overview
• Figures 1-4: Flow Charts for Denominator and Numerator calculations
• Table 1: Total, Severe and Moderate UNC rates;
Statewide, California 2011
• Figure 5: Frequency Distribution of UNC (Total), for all California Hospitals 2011
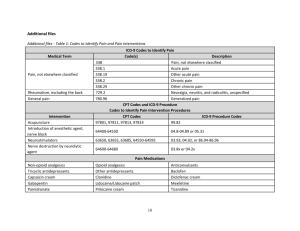
• Table 2: UNC Sub-measures to help interpretation and drive quality improvement activities
• Appendices 1-6 (ICD-9 Code tables, see Excel file) v2.3 July 2013
Unexpected Newborn Complications (UNC): Overview (1)
aka NQF 716: Healthy Term Newborn
• Key maternity outcome measure
– The most important childbirth outcome for families is a healthy baby. UNC is the first well-balanced and validated measure to address this gap.
– Also serves as a balancing metric for maternal measures such as NTSV CS,
3 rd /4 th degree lacerations, episiotomy and early elective delivery rates
• Denominator: Term infants without “pre-existing conditions”:
– Exclusions: preterm, <2500gm BWt, multiple gestations, all congenital anomalies (“big or small”), other fetal conditions, and exposures to maternal drug use
• Numerator: a set of either short or long term complications that would significantly concern for the mother/family.
– Identified by focus groups of neonatologists and families
– Grouped into severe and moderate levels
– An additional principle is the identification of cases of family separation
/disruption: term babies that require neonatal transport to another facility or baby complications that require a stay longer than their mother v2.3 July 2013
Unexpected Newborn Complications: Overview (2)
• Utilizes administrative data sets with unique safeguard strategies for both under- and over-coding
– Combines diagnosis codes and procedure codes and Length of Stay
• Under-coding:
– If a baby is missing a diagnosis code (e.g. HIE/asphxia), the case is still likely to be identified using procedure codes (head cooling, intubation, resuscitation) or a neonatal LOS > mother LOS
– A baby would also be included if it has a very long LOS without any diagnosis codes to explain it after excluding drug withdrawal, jaundice, social reasons (adoption, placement, homeless)
• Over-coding:
– Certain codes may not truly represent serious morbidity such as Sepsis with an under 4 day LOS (most likely represents “r/o sepsis” rather than true sepsis), or “other birth injuries” that do not keep the baby longer than the mother v2.3 July 2013
Unexpected Newborn Complications: Overview (3)
Advantages (over other approaches to neonatal morbidity)
• No administrative data source for term baby NICU admissions
– In any case, term NICU admissions can include observation cases and those with minor issues and local protocols vary for many conditions
• Composite Measures that use ICD-9 codes alone are subject to over or under stating the true morbidity
– For the AHRQ Birth Injury measure (PS-17), more than 2/3 of the cases identified belong to the non-specific birth injury codes (767.8, 767.9)
– Many California hospitals have no reporting of codes 768.5 or 768.6, birth asphyxia, presumably for medical-legal reasons
• Can be calculated with administrative data alone
Disadvantage
• Requires a linked set (that provides the proper checks and balances)
– Baby Discharge Diagnosis file (ICD-9 codes, LOS and Disposition)
– Birth Certificate (Birth Weight, Gestational Age, Method of delivery)
– Linkage algorithms well established by CMQCC v2.3 July 2013
Hospital Discharge
Diagnosis File
Revised Specifications v2.3
NQF #716: Unexpected Newborn Complications
(aka Healthy Term Newborn)
Figure 1: Denominator Inclusions n
No n
No
BWt ≥2.5kg?
Yes
No
Yes
GA ≥37wks?
GA Unknown
Use Birth Certificate or Medical Record: Birthweight
Note: ICD9 and DRG codes alone are very poor at identifying term infants. Therefore, the GA from BC is used.
Use Birth Certificate or Medical Record: Best
Obstetric Estimate of Gestational Age
Use Birth Certificate or Medical Record:
LMP-based Gestational Age
No
No
Not in Measure
Population
Singleton
Livebirth?
Yes
GA ≥37wks?
Yes
Screen for ICD-9 Diagnosis Codes V3000 or V3001
GA Unknown
Yes
BWt ≥3kg?
Starting
Denominator
Use Birth Certificate or Medical Record:
Birthweight
These represent backup criteria. Birth
Certificate Obstetric
Estimate of GA usually is present for
>99% of cases, and then these two steps may be omitted v2.3 July 2013
Starting
Denominator
Exclusions
Yes Congenital malformations?
No
Yes Other Fetal
Conditions?
No
Yes Maternal
Drug Use?
No
Final
Denominator
Revised Specifications v2.3
NQF #716: Unexpected Newborn Complications
(aka Healthy Term Newborn)
Figure 2: Denominator Exclusions
Use Patient Discharge Diagnosis Data, examining both
Primary and Other Diagnosis fields for specific ICD-9
Codes defining a wide array of Fetal Malformations and
Genetic Disorders (see Appendix 2, Group A)
Use Patient Discharge Diagnosis Data, examining both
Primary and Other Diagnosis fields for specific ICD-9
Codes defining an array of other Maternal and Fetal
Conditions (see Appendix 2, Group B)
Use Patient Discharge Diagnosis Data, examining both
Primary and Other Diagnosis fields for specific ICD-9
Codes defining an array of Maternal Drug Use Diagnoses
(see Appendix 2, Group C)
In summary, the Final Denominator excludes most serious fetal conditions that are “preexisting” (present before labor), including: prematurity, multiple gestations, poor fetal growth, congenital malformations and genetic disorders, other specified fetal and maternal conditions and maternal drug use.
v2.3 July 2013
Yes
Yes
Yes
Yes
Yes
Numerator:
Severe Complications
Final
Denominator
Neonatal
Death?
No
Revised Specifications v2.3
NQF #716: Unexpected Newborn Complications
(aka Healthy Term Newborn)
Figure 3: Numerator Inclusions: Severe Complications
Use Patient Discharge Diagnosis Data:
Disposition Code for Death
Use Patient Discharge Diagnosis Data:
Disposition Code for Transfer to Higher Level of Care
Neonatal
Transfer?
No
5’ or 10’
Apgar ≤3?
No
Severe ICD-9
Code?
No
Use Birth Certificate or Medical Record: Apgar Score at
5 minutes or 10 minutes ≤3
Use Patient Discharge Diagnosis Data, examining both Primary and Other Diagnosis and Procedure fields for specific ICD-9
Codes defining a array of specific Severe Complications, included selected codes from the categories of: Birth Injuries,
Hypoxia/Asphyxia, Shock/Complications, Respiratory
Complications/Procedures, Infections, Neurologic
Complications. (see Appendix 3, Groups 3A thru 3I)
Use Patient Discharge Diagnosis Data, examining both Primary and Other Diagnosis fields for the specific ICD-9 Code defining sepsis but also requiring a neonatal Length of Stay >4 days.
(see Appendix 3, Group 3J)
Sepsis and
LOS >4 days?
No
Starting Population for
Moderate Complications Analysis v2.3 July 2013
Starting Population for
Moderate Complications Analysis
Revised Specifications v2.3
NQF #716: Unexpected Newborn Complications
(aka Healthy Term Newborn)
Figure 4: Numerator Inclusions: Moderate Complications
Moderate Comps
(No LOS)?
No
Yes
Use Patient Discharge Diagnosis Data, examining both Primary and Other Diagnosis and Procedure fields for specific ICD-9
Code defining a specific Moderate Complication, that do not require a prolonged LOS (see Appendix 4, Groups A thru C)
No LOS >4d CS or
LOS >2d Vag?
Use Patient Discharge Diagnosis Data for LOS and for ICD-9
Diagnosis Codes V3000 (vaginal birth) or V3001 (Cesarean birth)
Yes
Moderate Comps
(with LOS)?
No
Yes
Use Patient Discharge Diagnosis Data, examining both Primary and Other Diagnosis and Procedure fields for specific ICD-9
Codes defining a array of specific Moderate Complications, included selected codes from the categories of: Birth Injuries,
Hypoxia/Asphyxia, Shock/Resuscitation, Respiratory
Complications/Procedures, Infections, Neurologic
Complications. (see Appendix 4, Groups D thru H)
No
Yes
LOS>5d?
Yes
Jaundice or
Social codes?
No
Use Patient Discharge Diagnosis Data to determine LOS
Use Patient Discharge Diagnosis Data, examining both Primary and Other Diagnosis and Procedure fields for the specific ICD-9
Code defining Neonatal Jaundice or Social Indications for prolonged hospitalization. (see Appendix 5, Groups A thru C)
Not in
Numerator
Numerator:
Moderate Complications v2.3 July 2013
NQF #716: Unexpected Newborn Complications
(aka Healthy Term Newborn, Revised Specifications)
Table 1: Final Measure Calculations
Unexpected Newborn Complications (Total): (rate per 1,000 livebirths)
(Severe Complications Numerator + Moderate Complications Numerator) x 1,000
Final Denominator
California state-wide rate in 2011: 39.3 per 1,000 births
Unexpected Newborn Complications (Severe): (rate per 1,000 livebirths)
(Severe Complications Numerator) x 1,000
Final Denominator
California state-wide rate in 2011: 23.1 per 1,000 births
Unexpected Newborn Complications (Moderate): (rate per 1,000 livebirths)
(Moderate Complications Numerator) x 1,000
Final Denominator
California state-wide rate in 2011: 16.2 per 1,000 births v2.3 July 2013
Fig. 5: Frequency Distribution of UNC Measure
In California Hospitals (2011-2012)
70
60
50
40
30
20
10
0
Total Unexpected Newborn Complications
California Mean = 36.0/1,000 (3.6%)
Rate (per thousand)
Significant variation noted in both large and small hospitals v2.3 July 2013
Revised Specifications
NQF #716: Unexpected Newborn Complications
(aka Healthy Term Newborn)
Table 2: Sub-Measure Calculations
An additional feature is the ability to calculate several sub-measures to direct Quality
Improvement efforts. These “buckets” include like-diagnoses from both severe and moderate categories. Hospital level comparisons show significant variation in these categories. This Sub-measure analysis allows hospitals to focus on specific care practices to drive QI. See Appendix 6 for details on the Sub-Category groupings.
Neonatal Complication
Sub-Categories
Respiratory
Infection
Transfer to Higher Level of Care
Neurologic/Birth Injury
Shock/Resuscitation
Long LOS (without clear diagnosis)
Proportion of
Total Complications
(California 2011-12)
41.9%
21.1%
16.6%
12.9%
3.1%
3.9%
Rate of each
Complication Category
(per 1,000 births)
14.9
7.5
5.9
4.6
1.1
1.4
v2.3 July 2013
Unexpected Newborn Complications:
Validation Studies
•
Face Validity:
– In a comparison trial for neonatal morbidity by gestational age tracked very closely to NPIC (major East Coast perinatal data set) analysis using NICU admissions and major complications (in press)
•
Formal Reliability Testing
– NQF requirement using RAND statistical tools
– Tests ability to discriminate among hospitals
– Good is 0.8, excellent is 0.9
– Mean Reliability among 220 California hospitals =0.92
•
Stability within a hospital over time
– Tested for 3 6-month periods with minimal variation noted in
>90% of California hospitals v2.3 July 2013