Inquiry into Life Twelfth Edition
advertisement
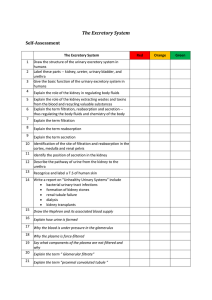
Lecture PowerPoint to accompany Inquiry into Life Twelfth Edition Sylvia S. Mader Chapter 16 Urinary System and Excretion Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Organs of excetion • EXCRETION: is the process that rids body of METABOLIC WASTES. • Excretion is performed by: KIDNEYS: excrete Nitrogenous Wastes (Ammonia, Urea, Uric Acid, Creatinine) LIVER: excrete Bile Pigments LUNGS: excrete CO2 SKIN: water, urea in sweat • Excretion is not the same as DEFECATION, which is the process which rids the body of UNDIGESTED, UNABSORBED food remains, plus bacteria -- NOT metabolic end products. 16.1 Urinary System • Functions of the Urinary System – Excretion of Metabolic Wastes • Urea, Creatinine, Uric acid, ammonia – Maintenance of Water-Salt Balance • NaCl, K+, HCO3-, Ca2+ – Maintenance of Acid-Base Balance • Excretion of H+, reabsorption of HCO3- – Secretion of Hormones • Renin, Erythropoietin The Urinary System Organs of the Urinary System – Kidneys • Located in lumbar region • Produce about 1ml of urine every minute • Covered by tough capsule of fibrous connective tissue • Concave side has a depression called a hilum – Location of renal artery and vein Organs of the Urinary System – Ureters • Conduct urine from kidney to bladder • Three-layered wall – Mucosa, smooth muscle, outer connective tissue • Conveys urine by peristalsis 16.1 Urinary System • Organs of the Urinary System – Urinary Bladder • Stores urine • Has three openings – Two for the ureters, one for the urethra • The bladder wall is expandable • Two sphincter muscles control the release of urine into the urethra (internal and external sphincter) 16.1 Urinary System • Organs of the Urinary System – Urethra • A small tube that leads from the urinary bladder to an external opening • It’s function is to remove urine from the body • The urethra is longer males than females • The urethra also transports semen in males 16.1 Urinary System • Urination – Stretch receptors in wall of bladder • Send impulses when bladder fills to 250 ml • Motor impulses from spinal cord – Bladder contraction – Micturition occurs 16.2 Anatomy of the Kidney and Excretion • There are three regions to a kidney – The renal cortex – The renal medulla – The renal pelvis • Nephrons are the functional units of the kidney – Each kidney has over one million nephrons Gross Anatomy of the Kidney 16.2 Anatomy of the Kidney • Anatomy of a Nephron – A nephron is composed of a system of tubules – Each nephron has its own blood supply • From renal artery, afferent arteriole leads into the glomerulus • Blood leaves the glomerulus via an efferent arteriole • Efferent arteriole takes blood to peritubular capillaries – These surround rest of the nephron – Blood then goes to renal vein Nephron Anatomy 16.2 Anatomy of the Kidney • Parts of a Nephron – Glomerular capsule (Bowman’s capsule) • Cuplike structure • Inner layer has podocytes – Form pores for passage of small molecules – Proximal convoluted tubule (PCT) • Cuboidal epithelial cells with microvilli – Increased surface area for absorption 16.2 Anatomy of the Kidney • Parts of a Nephron – Loop of Henle • U-shaped tube – Distal Convoluted tubule (DCT) • Lack microvilli • Designed for tubular excretion rather than reabsorption – Collecting Ducts Processes in Urine Formation Glomerular Filtration – Glomerular Filtration • Blood enters the afferent arteriole and glomerulus • Blood pressure forces water and small molecules into the glomerular capsule (filtration) • Large molecules and formed elements cannot leave the capillaries • Remaining processes must reabsorb desirable substances and allow wastes to pass Glomerular Filtration – Glomerular Filtration Filterable Blood Components Nonfilterable Blood Components Water Formed elements Nitrogenous wastes Blood cells and platelets Nutrients Plasma proteins Salts Tubular Reabsorption • Tubular Reabsorption(PCT) • Molecules are reabsorbed both actively and passively –Sodium reabsorbed by active transport –Chloride follows passively –Water absorbed by osmosis Tubular Reabsorption Only molecules recognized by carrier proteins are actively reabsorbed –Glucose is an example –There is a limited number of carrier proteins –Excess glucose ends up being excreted Tubular Reabsorption • Tubular Reabsorption Reabsorbed Filtrate Nonreabsorbed Components Filtrate Components Most water Some water Nutrients Much nitrogenous wastes Required salts (ions) Excess salts (ions) Tubular Secretion (DCT) – Tubular Secretion (DCT) • Hydrogen ions, potassium, creatinine, many drugs • Actively transported from the blood • Tubular secretion occurs here – Urine Contains • Filtered substances that have not been reabsorbed • Substances that have been actively secreted Reabsorption of Water • Reabsorption of Water – Excretion of hypertonic urine depends on reabsorption of water from the loops of Henle and the collecting ducts – Reabsorption of water requires • Reabsorption of salt • Establishment of solute gradient • Reabsorption of water Reabsorption of Salt – Reabsorption of Salt • Regulated by the absorption and excretion of ions – Na+, K+, HCO3-, Mg2+ • More than 99% of Na+ filtered at the glomerulus is returned to the blood – 67% is reabsorbed at the proximal tubule – 25% is reabsorbed at the ascending limb of the nephron loop – The rest is reabsorbed from the distal convoluted tubule and the collecting duct Establishment of Solute Gradient in the renal medulla – A LOOP OF HENLE has two parts • Descending limb and ascending limb – Salt diffuses out of lower part of ascending limb – Upper part of ascending limb actively transports more salt out – This creates high osmotic pressure (high solute concentration) within the tissues of the renal medulla Establishment of Solute Gradient – Urea contributes to high solute concentration in medulla – Leaks from lower collecting duct – This results in a concentration gradient favoring reabsorption of water Loop of Henle • Descending limb of loop of Henle – Water is reabsorbed into the capillary network due osmosis (hypertonic nature of the tissue fluid within renal medulla) • Created by urea leaking from the collecting duct Loop of Henle – Ascending limb of loop of Henle • Impermeable to water – As you move up the medulla concentration is decrease (filtrate is hypertonic to the surrounding) • At lower region NaCl moves into blood passively • At upper region NaCl is actively transported into blood (there is less and less salt available for transport out as you move up) Reabsorption of Water • Reabsorption of Water – Water leaves distal convoluted tubule because of the osmotic gradient (responds to aldosterone) – Water also leaves descending limb of loop of the nephron • Countercurrent multiplier – As filtrate enters collecting duct it is isotonic to cells of renal cortex so no net movement of water Collecting duct • Up to this point blood and filtrate has similar tonicity • As the collecting duct moves into the medulla it is subject to the same [gradient] as the loop of henle – Water diffuses out and urine become hypertonic to blood plasma Juxtaglomerular Apparatus Hormonal Regulation at the DCT Occurs when blood pressure at the glomerulus is low »Juxtaglomerular Apparatus secretes renin »Renin is an enzyme that changes angiotensinogen into Angiotensin I »Angiotensin I is then converted into Angiotensin II (vasoconstrictor) via angiotensin-converting enzyme found in the lungs Aldosterone release »Angiotensin II stimulates the adrenal cortex to release aldosterone »Aldosterone promotes the excretion of K+ and the reabsorption of Na+ »The reabsorption of Na+ (in DCT) is followed by the reabsorption of H2O »Blood volume and blood pressure increase BP regulation by Kidney via renin BP regulation by Kidney via renin Hormonal Regulation at the DCT and ANH Atrial naturietic hormone (ANH) » Another hormone regulating sodium » Secreted by right atrium of heart in response to stretching » Indicates increased blood volume » Inhibits renin secretion by juxtaglomerular apparatus » Inhibits aldosterone release » Promotes sodium excretion - natriuresis Antidiuretic Hormone • Anti-pee drug – Permeability of collecting duct is under hormonal control • Antidiuretic hormone (ADH) is produced by the hypothalamus and released by the posterior pituitary gland – In the absence of ADH, a dilute urine is produced – In the presence of ADH, the collecting duct become more permeable to water and a concentrated urine is produced X= Pituitary Gland Anterior and Posterior Pituitary (FSH, LH, MSH, ACTH, TSH, Prolactin) ADH and the hormone oxytocin are released by the posterior pituitary. STIMULUS: Hypothalamus detects low blood volume (i.e. it detects concentrated blood) HYPOTHALAMUS ADH made here NEGATIVE FEEDBACK! POSTERIOR PITUITARY ANTERIOR PITUITARY ADH sent here ADH released into blood BLOOD VOLUME RISES (blood becomes more dilute) ADH travels in blood to kidney. There, it acts on collecting ducts and distal tubules, causing them to reabsorb more water from the filtrate back into the blood. STIMULUS: Hypothalamus detects low blood volume (i.e. it detects concentrated blood) HYPOTHALAMUS ADH made here NEGATIVE FEEDBACK! POSTERIOR PITUITARY ANTERIOR PITUITARY ADH sent here ADH released into blood BLOOD VOLUME RISES (blood becomes more dilute) ADH travels in blood to kidney. There, it acts on collecting ducts and distal tubules, causing them to reabsorb more water from the filtrate back into the blood. 1. blood volume drops if not enough water is being consumed 2. this is detected by receptors in the hypothalamus. 3. This stimulates hypothalamus to produce ADH and send it to pituitary gland 4. Pituitary gland releases ADH into blood STIMULUS: Hypothalamus detects low blood volume (i.e. it detects concentrated blood) HYPOTHALAMUS ADH made here NEGATIVE FEEDBACK! POSTERIOR PITUITARY ANTERIOR PITUITARY ADH sent here ADH released into blood BLOOD VOLUME RISES (blood becomes more dilute) ADH travels in blood to kidney. There, it acts on collecting ducts and distal tubules, causing them to reabsorb more water from the filtrate back into the blood. 1. 2. 3. ADH acts on the collecting duct and distal convoluted tubule, causing them to reabsorb more water from the kidney filtrate back into the blood as there is less water in the filtrate, less urine is produced. Blood volume rises. This is detected by the hypothalamus, which will then shut off the release of ADH (negative feedback) 16.3 Regulatory Functions of the Kidneys • Diuretics – Increase flow of urine – Alcohol • Shuts off ADH • Dehydration causes hangover – Caffeine • Increases glomerular filtration rate • Decreases tubular reabsorption of sodium – Diuretic drugs • Many inhibit active transport of sodium at loop of the nephron or the distal convoluted tubule Acid-Base Balance - Normal pH for most body fluids is 7.4 – Alkalosis: pH is greater than 7.4 – Acidosis: pH is less than 7.4 – Several Mechanisms Maintain a pH of ~ 7.4 • Acid-Base buffer system • Respiratory Center • The Kidneys Acid-Base Balance – Acid-Base Buffer Systems • Chemical or combination of chemicals • Can take up excess H+ or OH• Prevents large changes in pH • When H+ added to blood the following occurs H+ + HCO3- H2CO3 • When OH- added to blood the following occurs OH- + H2CO3 HCO3- + H2O Acid-Base Balance – Respiratory Center • Increasing breathing rate removes CO2 – Removes hydrogen ions – Forces reaction to the right H+ + HCO3- H2CO3 H2O + CO2 • Respiratory system adjusts proportion of bicarbonate and carbonic acid Acid-Base Balance – The Kidneys • • • • • • Only kidneys can remove many acids and bases Slower acting than respiratory system but more powerful Reabsorbs bicarbonate ions Excretes hydrogen ions In urine, ammonia can absorb hydrogen ions Phosphate provides another means of buffering hydrogen ions in urine Acid-Base Balance Glucose K+, ions Amino Acids HCO3- Na+ Drugs, Creatinine NaCl Increasing Saltiness H2O NH3 H+ H2O Cortex H2O K+, ions H+ NH3 NaCl H2O H2O H2O H2O NaCl H2O Outer Medulla Urea Inner Medulla Active Transport Passive Transport 16.4 Disorders of the Urinary System • Disorders of the Kidneys – Pyelonephritis: Infections of the kidneys • Kidney infections usually result from bladder infections • Most are curable with antibiotics if diagnosed in time • Some infections can cause severe damage – Kidney Stones • Hard granules that form in the renal pelvis • Composed of substances such as calcium, phosphate, uric acid, and protein • Excess animal protein in the diet, imbalanced urinary pH, and urinary tract infections may be contributing factors • May pass unnoticed in the urine; large stones can be very painful – The presence of albumin or blood cells in the urine are early signs of kidney damage 16.4 Disorders of the Urinary System • Disorders of the Kidneys – Hemodialysis • Artificial kidney machine or continuous ambulatory peritoneal dialysis (CAPD) • Dialysis – – – – – Diffusion of dissolved molecules through a membrane Selective permeability Blood is cleansed pH is adjusted Water and salt balance maintained • In CAPD the peritoneum is the dialysis membrane An Artificial Kidney Machine 16.4 Disorders of the Urinary System • Disorders of the Bladder and Urethra – Bladder Infections • Urine leaving the bladder is usually bacteria-free • The urethra is normally colonized with bacteria • Sometimes bacteria make their way to the bladder – Usually treatable with antibiotics – Bladder Stones • Occur as a result of bladder infections or prostate enlargement • May actually be kidney stones that were carried to the bladder • Can be removed surgically or broken apart by lithotripsy – Bladder Cancer • Smoking greatly increases the risk • Some types are very malignant necessitating removal of the bladder. a) Label the parts indicated above and give one function for structures Y and Z b) Which of the following is not a function of the organ shown? A. to produce urea B. to excrete metabolic wastes C. to regulate the acidity of the blood D. to maintain a constant blood volume a) Identify the parts of the nephron in the following diagram. b) Compare and contrast the composition of blood in V with Z c) In a healthy person, the sequence of structures through which most glucose molecules pass is a) U, X, Y b) U, W, Z c) W, Z, X d) W, X, Y 1. The process that occurs at W is A. tubular excretion. B. pressure filtration. C. reabsorption of water. D. selective reabsorption. 2. The permeability of which structure is altered by secretions from the adrenal cortex? A. W B. X C. Y D. Z • Demonstrate your understanding of negative feedback by describing how the kidneys and the hypothalamus work together to regulate blood volume. (5 marks) 1. Describe the process by which each of the following affects the composition of filtrate in the nephron. (4 marks: 2 marks each) a) Proximal Tubule b) Loop of Henle a) Name the parts X and Y in the diagram b) List three ways that the blood in vessel Y differs from the blood in vessel X COMPONENT glucose amino acids proteins inorganic salts urea uric acid 1. PLASMA 0.10 1.05 8.00 0.72 0.03 0.004 FILTRATE 0.10 1.05 0.01 0.72 0.03 0.004 URINE nil nil 0.01 1.50 2.00 0.05 The table shows the amounts of substances present in human blood plasma, glomerula filtrate and urine. All are measured in grams per 100 cm3 of fluid. a) Account for the differences in the levels of proteins in the plasma and filtrate. ( 1 mark) b) The concentration of inorganic salts in urine is approximately double that present in the filtrate. Explain this difference. (3 marks) 1. Alcohol appears to inhibit the secretion of anti-diuretic hormone (ADH). Predict the results of alcohol intake on the following. Include in your answer a description of the mechanism responsible for the resulting concentration. a) solute concentration of the blood plasma (3 marks) b) urine production (2 marks) 1. Assume that a bacterial infection results in large perforations in the glomerulus and the Bowman’s capsule of a patient. a) How will the glomerular filtrate in the diseased person compare to the glomerular filtrate of a healthy person? (2 marks) b) What effect will this have on the level of antidiuretic hormone (ADH) circulating in the bloodstream? (1 mark) c) A person with this disease would experience swelling of the body tissues. Using your knowledge of kidney function and the blood tonicity, explain the mechanism that accounts for this swelling. (3 marks) SUBSTANCE a. Glucose b. Protein c. Ammonia CONCENTRATION IN PLASMA g/100 mL 0.100 8.00 0.004 CONCENTRATION IN FILTRATE g/100 mL 0.100 0.000 0.004 CONCENTRATION IN URINE g/100 mL 0.000 0.000 0.07 a) Account for the filtrate and urine concentrations in each of the above substances by stating the part of the nephron and the process or processes responsible for producing each of the concentration values. (9 marks) b) Explain what could cause high levels of glucose in the urine. (2 marks)