File - Gail McIlvain Simpson Teaching Portfolio
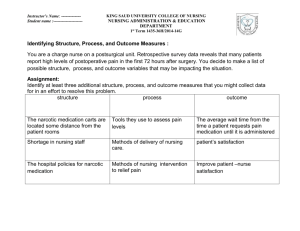
advertisement

1 Elizabeth Chance ED.D, MSN, RN Michelle Malloy BSN, RN Gail McIlvain-Simpson, MSN, PNP-BC A.I. DUPONT HOSPITAL FOR CHILDREN CLINICAL ORIENTATION 2 Instructors for Childbearing 3E and 3F A.I.duPont Hospital for Children Elizabeth Chance, W: (302) 292-3882, C: (302) 690- 5374, E-mail: echance1@dtcc.edu Michelle Maloy, H: (302) 395-2922, C: (302) 379-3478. E-mail:mmaloy1@dtcc.edu Gail McIlvain-Simpson, W: (302) 453-3040; C: (302) 690- 2744 E-mail: gsimpso7@dtcc.edu Pager #: 2476357 3 4 5 6 What type of reaction do you have when you think of your pediatric rotation here? 7 8 9 General Information (pg.1) Clinical Hours: You need to be on time to receive clinical assignment Monday, 0630-1300 or Monday, 1400-2030 Tuesday, 0630-1400 or Tuesday, 1400-2130 Uniform: Student Uniform with Delaware Tech Picture ID and patch. Bring stethoscope, black ink pen, pen light, highlighter, scissors and clinical notebook. Lunch: Meals are available in the employee cafeteria. You must have a student ID to get a discount. You may bring a snack or lunch with you. Storage: Limited space. Leave valuables at home. 10 Clinical Absence Call clinical instructor at home by 0530 (AM clinical) or 1230 pm (PM clinical) if you are going to be late or absent. If you are in the community the day you are absent or late, call the community instructor by 0700. 11 HIPAA Written Verbal 12 Safety Guidelines for Hospitalized Children ( pg. 17) Make sure the child has an ID band and security alarm on wrist or ankle ( at beginning of shift). Keep the environment safe by keeping: Keep side rails up at all times Beds of ambulatory children locked in place and at the lowest possible height. The room neat, clean and organized. Keep bedside table away from crib/bed. Floor clear of fluids or objects that could contribute to a fall. Directly supervise infant and preschool children when OOB. & older children if needed Check all children at least every hour. Check bath water carefully before placing a child in a bath. Strap infants and small children into infant seats, feeding chairs and stroller securely. Do not leave infants or children unattended in treatment rooms or on scales. Assess toys brought to the hospital by parents or visitors for: Appropriateness for age and condition. Washable and unbreakable. Absence of small, removable parts that can be aspirated or swallowed. Set limits for the child’s safety: Make sure the child understands where he/she is permitted to go and what he/she is permitted to do in the hospital. Enforce limitations consistently 13 Cribs come in all shapes and sizes 14 Identification Bands (pg.4) It is your responsibility to check that the child has an ID band. Each child will have both an ID band and an electronic alarm. If “Tag Alert” is announced make sure you check on your patient. 15 What is your scope of practice for Pediatric Clinical? What you can do What you cannot do Bath Intravenous therapy Linen changes TPN (Total parenteral nutrition) Assessments Document in EPIC Vital signs Weights, heights, head circumference Intake and output measurements Developmental stimulation Required nursing skills with instructor (i.e. medications) Point of care testing: blood sugars, N-G ph testing, guiac Respiratory medications Intravenous medications 16 Required Nursing Skills Instructor needed (pg.5) 1. Procedures related to alternative feeding techniques: (Wong’s Textbook: p. 745-750). Gavage feeding: NG, NJ, ND Gastrostomy feeding Students should be ready to perform tube feedings and should be prepared on how to use the “flexiflow feeding pump” equipment. (Pump available in the lab). 2. Pediatric Administration of Medications: (Wong’s Textbook: p. 717-732). All medications, even topical a. Generic and trade name. b. Classification c. Mechanism of Action d. Dosage: compare to calculation of min/max per dose e. Side effects and possible adverse reactions f. Nursing Considerations 3. Dressing Changes: (Wong’s Textbook: p. 1065-1069; 750-751). Dry dressings Wet compresses or dressings Soaks Baths Ostomies Catheterization, suctioning, and enemas: (Wong’s Textbook: p. 713-714; 741-745; 750). *Reminder: Any omission of the required nursing skills or procedures may be reflected on a Clinical Advisement Form. 17 Are you ready for the day? Clinical notebook (reference items) Stethoscope, penlight, scissors black ink pen, highlighter ( Watch with second hand) DTCC ID Know area where you are to park 18 A. I. DuPont Parking (pg. 2) 19 20 21 Active Orders and MAR (pg.4) Your instructor will print a copy of the active orders and MAR for your child; you should use the information to organize your care. When you arrive on the unit, obtain your assignment from the instructor. Review any information needed to provide morning/evening patient nursing care. What questions do you have for the nurse giving you report? Introduce yourself to nurse. Get report from staff nurse. Most importantly, communicate how long you will be on the unit and the care you will be providing for patient and family After receiving your assignment, you may start your nursing care. Provide verbal report to staff nurse before leaving the unit. All active orders and MAR regarding your child must be returned to the instructor before you leave the unit for the day (HIPPA). 22 We are guests 23 24 Vital signs (pg.3) You are responsible for the vital signs including the pain scale ordered between and including 0800 to 1200 and 1600 to 2000 (Pain scale hourly). Obtain the pulse by the apical route if the child is 3 years of age or younger. Obtain a BP on each child using the space lab. Vital sign frequency is found on the active orders. Check previous vital signs to obtain a baseline before doing your assessment. Report vital signs to instructor and staff nurse. Report the route used for obtaining the temperature (temporal, axillary, oral). 25 26 Weights and Heights (pg.3) Weights are obtained weekly for the child less than 12 months unless otherwise specified in active orders. Check the active orders to review the prior weight for comparison. Weigh the child in the morning before breakfast. Child must be weighed without clothing and diaper. Make sure to use scale assign to the child’s room. 27 28 29 30 Feedings (pg.3) •Verify the type and amount of feeding on active orders. •Have all feeding equipment ready (bottles, nipple, formula, tube feedings). •You may have to order breakfast, lunch, or dinner for your child (meals do not automatically come up). 31 Flexiflow Quantum 32 Intake and Output (pg.3) •Every child is on intake and output. •Document the intake and output on the Childbearing Database, report to clinical instructor & staff nurse. •Intake – be specific when charting the amount in metric system. •Output – If the child is not potty trained, weigh the diapers to obtain the correct amount of urine and/or stool. •To measure outputs in older children utilize commode, hat, or urinal (if child is older or ambulatory explain to child & parents that you are keeping I&O) 33 34 35 36 Medications (pg.4) You will administer medications at the Nemours Hospital with your instructor’s supervision and guidance. You will be responsible for the theory related to the medications on both weeks that you are at Nemours Hospital. You will be responsible for administration of any medication (po, IM, sq, rectal, ophthalmic, otic or topical ) ordered between and including the hours of 0800 to 1200 (inclusive of medication at this time). Section 593 students are responsible for medication administration between the hours of 1600-2000 (inclusive of medication at this time). You are responsible for knowledge related to IV, inhaler and nebulizer medications but will not be administering the medications. Refer to the Pediatric Medication Administration Guidelines for further information. 37 General Guidelines (pg.6) Prior to preparation of medication, verify the medication in the patient’s orders. Assess for client allergies. All administration of medications will include the 3 checks for correct medication including the expiration date. Know child’s weight and any allergies. Follow the 7 rights – medication, dose, route, patient, time, and right to know and right to refuse. Be prepared to discuss medication knowledge (will discuss next). Do not leave any medication unattended. When you are ready to give a medication, let the instructor know. The instructor will be present for preparation and administration of any medication. Scan the patient’s ID band prior to administration of any medication. Scan every medication before given. You must do this each and every time you give the medication. The instructor will document the medication administration on the computer. 38 Pediatric Medication Knowledge (pg.6) Generic and trade name. Classification Mechanism of Action Dosage – compare to calculation of min/max per dose Side effects and possible adverse reactions Nursing considerations including necessary assessment before/after giving the medication. Patient education/preparation Have pertinent Lab data and assessment available (electrolytes, PTT, BP, HR, etc.) The information must be readily available prior to the instructor’s presence (written in your care plan, on individual cards, or on notepaper. Note: An omission at any step in the procedure may be reflected on a Clinical Advisement Form. 39 40 41 42 43 Nurses Notes (pg.3) Should include an assessment pertaining to your child’s condition – If child admitted for fever state whether there is a fever and give details (Tylenol administration & response) Do not include statements such as : AM care performed or bath given, vital signs given 44 Parent Visitation Any responsible adult may stay with the child 24 hours a day. Family Contact by phone or visit should be reported to nursing staff. Family Resource Center 45 Break/Lunch (pg.4) A lunch/dinner break will be provided. You may take a mid-morning or mid-afternoon break if needed. The timing of the break should be based upon your child’s needs and the nursing care needed. Let the staff nurse and the instructor know when you are going to leave the unit. 46 Downtime Make sure you have collected essential information needed for Databases and Concept Maps Are there other services you can provide to your child and their family? Can you assist fellow students with their assignments? Every student needs to complete work before we can leave Is there anything you can do to help the unit? Explore resources Are there other learning opportunities? 47 How to Get and Give Report Getting report – Ask specific questions in regards to your individual patient (what do you need to know to effectively care for that patient during your clinical time on the unit.) Giving report – Be succinct & organized Demographics, assessments (VS, I&O, pain scales, weight, ht, head circumference), tests, alerts, status. Consultations, visitors. You must give report before leaving unit!! 48 Postconference Topics Concept Maps (Nursing Diagnoses) Community experiences Growth & Development Articles & Rubric 49 Resources (Personnel) Advanced Practice Nurses Specialty nurses Social Work Child Life Library Pharmacist Ward/unit clerk ETC………… 50 Resources Non-personnel Lexi Comp – pharmacy issues Info Link – evidence based medicine KIDSHEALTH.org – child/family information Library 51 Policies and Procedures 52 Procedure Room 53 Development, Dissemination and Enculturation The Magnet Model 54 Exemplary Professional Practice Successes: Shared Governance Congress and Councils Nursing Advancement Program AtStaff scheduling system, unit based scheduling committees, unit based staffing guidelines SWAT nurses, Clinical Informatics Nurses EMR documentation Reward programs: Nurses Week, Magnet Awards, DAISY Awards, Service Awards, Nursing Spectrum and Delaware State Nursing Practice awards Comprehensive quality data disseminated to Quality Council unit representatives and Nursing Leadership 55 Announcements Code Blue Code Red Tag alert Delta alert Trauma alert 56 Assignments 57 Assignment for Clinical Weeks at Nemours Hospital You are required to complete and submit the Childrearing Database and Concept Map every week while in the hospital setting. On a full clinical week (Mon & Tues) completed database and concept maps are due on TUESDAY at post conference. Be prepared to discuss the information at post-conference. On a split clinical week (orientation and/or community day) completed database and concept maps are due on WEDNESDAY by 1600. On a split clinical week, section 593 students submit database and concept maps also on WEDNESDAY by 1600 to full time faculty Gail McIlvain-Simpson’s mailbox. Section 501 and 592 students complete the weekly self-evaluation found under the “Assignment Tab” on blackboard by 1000 Wednesday and 593 students by 1400 on Wednesday. 58 Directions: The student is responsible to complete the clinical self-evaluation assignment on Blackboard each week by 10AM, Wednesday. Student Clinical Week Date Client Diagnosis I was able to address the following client problems: HOW? I provided the following basic care, skills and procedures: Did you have any difficulty? I administered medications by the following routes: What medications & what route – any difficulties? My clinical performance was strongest in the following areas: If I could repeat this clinical week, I would do the following things differently: I feel that I could improve in the following areas: My plans for improvement in these areas include the following actions: Please be as detailed as possible – this information is to be utilized on your evaluation. 59 Assignment for Community Week (pg.7) Obtain a pediatric nursing evidence-based research article from a valid and reliable source within the last five years. Article must be on anything related to the pediatric population (i.e. any disease entity or lecture material covered in class). Use library Database – see instructions on Blackboard The article should not be a letter to the editor, news letter, medical newsletter, case study, or Kidshealth.org. Highlight the important information and submit to your instructor at postconference. Evaluate the article using the criteria from the Journal Evaluation rubric included in clinical notebook. Write supporting comments and score on the rubric sheet. Complete the self-evaluation for the community experience found under the “Assignment Tab” under the “Childrearing Community Assignment” folder on blackboard. Section 501 & 592 students complete by 1000 on Wednesday and 593 students by 1400 on Wednesday. 60 Department of Associate Degree of Nursing NUR 144 (pg.8) Student Name: _________________________________________ Research Article Rubric Date: _________________ 12/12/07-EC 14 Factor Code/ Description W1 Content Relevance W2 Quality of Expression Total Pts 30 30 W3 References 20 W4 Mechanics 10 W5 Formatting 10 Unacceptable Article misses some of the content specified by the instructor and/or the coverage of the content is superficial (1-23) Article is unclear and/or disorganized; use of vocabulary and/or syntax would be unacceptable for professional publication (1-23) References are not cited and/or the primary sources are from non-peer reviewed sources (1-15) Article has numerous typographical, spelling and/or punctuation errors (1-7) Article is not research-base generated and/or is in substantial non-compliance with APA guidelines (1-7) Acceptable Target Article addresses the content specified by the researcher (24-26) Article fully and thoroughly addresses the content specified by the researcher (27-30) Article is clear; vocabulary and syntax are sometimes less formal than expected for professional publication (24-26) Article has a scholarly quality, express points in a clear, logical and organized manner; contain vocabulary and syntax that reflect standards suitable for professional publications (27-30) Article has cited references from primarily peer reviewed journals (18-20) Article has references many of which are not from peer reviewed journals (16-17) Article has few typographical, grammatical, spelling and/or punctuation errors (8) Article is free of typographical, grammatical, spelling and punctuation errors (9-10) Article is researchbase generated and is in substantial conformance to APA guidelines; minor deviations are noted (8) Article is research-base generated and in conformance to APA guidelines (9-10) Scor e Comments 100 61 Childbearing Community Protocol You will be in the community for your pediatric clinical experience on Monday ______________ Those of you doing Think First for Kids and Tar Wars will meet at Delaware Tech in room C214 at 0730 for a pre-conference with your clinical instructor and clinical group (only those students participating in Think First for Kids& Tar Wars). In blackboard under the “Course Protocols” tab you will find pertinent information regarding your assigned community site. On the course protocol tab in blackboard, select the “Childrearing Community Protocol” then click on the “Community Protocol Information” and then on the “Agency Protocols” where you will find additional objectives that are site specific, agency protocols, and any specific materials related to your community experience. You are responsible for reading/viewing this material prior to pre-conference on Monday morning. Your clinical instructor will be rotating to all of the community clinical sites. However, if you need to communicate with your instructor when she is not on site, you may call/page her. She will return your call as soon as possible. If you do not hear back from the instructor within 15 minutes, please call/page her again. If you are sick and will be absent on a day of your community health experience, Call your clinical instructor to notify her of any absence or lateness by 0700. Section 501 and 592 students submit community evaluation found on blackboard by 1000 Wednesday and 593 students by 1400 on Wednesday. 62 Clinical Evaluation Form Student’s Name __ Advisor __ ______ Evaluation - Interim / Final ___ Weeks ______ Total: Absence___ _____ Late_________ To pass this course clinically, the student must meet all clinical objectives. Specific Clinical Performance Criteria for each clinical objective are listed in the course syllabus. Clinical Objective Interim/Final 1. Implement safe nursing care incorporating theoretical knowledge, the nursing process and concepts of critical thinking for the individual client. 2. Implement therapeutic communication techniques when interacting with the client and members of the health care team. 3. Implement caring behaviors respecting the diversity of the individual, family and community. 4. Implement the management concepts of organization and collaboration while caring for the individual client. 63 Implement safe nursing care incorporating theoretical knowledge, the nursing process and concepts of critical thinking for the individual client. NANDA Database Concept Map 64 Implement communication techniques when interacting with the client and members of the health care team. 65 Implement caring behaviors acknowledging the diversity of the individual client. Identify available resources Demonstrate nonjudgmental approach Tactful & respectful approach 66 Implement the management concepts of organization and collaboration while caring for the individual client. 67 Incorporate knowledge of ethical and legal standards of nursing practice when caring for the individual client. d. Follow course protocol for reporting absences and lateness. f. Submit written materials on time. Professionalism Being prepared for clinical Submitting assignments on time 68 Incorporate knowledge of ethical and legal standards of nursing practice when caring for the individual client. d. Follow course protocol for reporting absences and lateness. f. Submit written materials on time. Professionalism Being prepared for clinical Submitting assignments on time 69 Advisements Issues regarding clinical objectives will be sited via advisements For example : Not calling instructor as per protocol for lateness or absence. Not submitting required work on time Inability to perform vital signs Unprofessional behavior 70 0630-0645– Receive client assignment (pg.12) Review active orders, MAR, H&P. Note any scheduled procedures for client. 0645- 0715 Listen to report with staff. Introduce self to staff and inform staff nurse of your duties for the day. Obtain report from staff. Plan and organize your time for the day. 0715-0830- Obtain vital signs, weight, pulse ox, pain assessment - Report vital signs to the staff nurse and instructor - Notify instructor of your child’s medication times by 0745 Obtain physical assessment Assist child with breakfast 0830-113 Report abnormal findings immediately to instructor and staff. Responsible for all patient care including 0800/1200 including VS and assessments. Bathe child and change linen. Continue Data collection (assessments) and therapeutic communication. Perform ordered procedures and skills under instructor supervision. Monitor and report intake and output to instructor/staff Responsible for administration of all medications except IV and respiratory medications ordered between 0800 and 1200. Assist classmates and/or staff when able. Make sure child’s room is clean and orderly Obtain noon vital signs Prepare child for lunch and assist with lunch as necessary. 1000-1230- - Finish care with child and family Complete assessment Complete nursing care with instructor’s guidance as necessary 71 1400-1445 - -Receive client assignment Review active orders, MAR, H&P. -Note any scheduled procedures for client. 1445-1515 -Listen to report with staff -Introduce self to staff and inform staff nurse of your duties for the day 1515-1630,- Obtain vital signs, weight, pulse ox, pain assessment -Report vital signs to the staff nurse and instructor. -Notify instructor of your child's medication times by 1545 -Obtain physical assessment -Assist child with dinner (1700) 1630-1730 Report abnormal findings immediately to instructor and staff. -Responsible for all patient care including 1600/2000 including VS and assessments. -Bathe child and change linen, if not already done for the day -Continue data collection (assessments) and therapeutic communication -Perform ordered procedures and skills -Monitor and report intake and output to instructor/staff -Responsible for administration of all medications except IV and -Respiratory medications ordered between 1600 and 2000 -Assist classmates and/or staff when able -Make sure child's room is clean and orderly 1730-1800 Dinner Break 1800-2000 -Obtain and report 2000 vital signs -Finish care with child and family -Verbally report off to staff nurse -Turn in active orders and MAR to instructor 72 73 74 75 Case study for Nurses Note Case Study for Nurses Note – You are assigned to a 4 month old with admitted with pneumonia. Child has history of Down’s syndrome & bronchopulmonary dysplasia. On 2 L of oxygen (nasal cannula). Respiratory rate 40-60. Breath sounds decreased in both lower lobes with scattered rhonchi. Has a gastrostomy tube. NG feeds received at 11 AM & at 1115 had emesis Nasal flaring and substernal retractions around 9 AM. Respiratory rate 60. PO2 90 at 09, 98 10, 92 @11 . Mid morning a respiratory treatment (nebulizer) performed at 0950. What might your nurses note look like? __________________________________________________________________________________ __________________________________________________________________________________ __________________________________________________________________________________ __________________________________________________________________________________ __________________________________________________________________________________ ______________________________________________________________ 76 Case Study #1 Pain Assessment 5th vital sign Patient: 2 year old, white, female Admitting Diagnosis: Left Lateral Neck Cellulitis Objective Data: VS- 38.2C, 145, 26, 127/72; left lateral neck swelling, erythematous ulceration Chief Complaint: “Fever, neck red and swollen” (4cm in diameter), warm to touch, small amount of serosanguinous drainage noted, pt. holding head towards the right and guarding neck, pt’s mother reports, “she’s not herself, usually very playful and talkative”, pt. now fussy, with occasional moans, more difficult to console, increased tone in b/l legs, and a worried facial expression. Subjective Data: Pt. reports, “boo boo” as she points to her left lateral neck. Orders: Q4 VS, I & O, IVF’s, IV antibiotics, Regular diet as tolerated, Bid dressing changes, I&D of wound, blood cultures, and patient isolation Medications: IV Clindamycin, PO Tylenol 77 As a group please answer the following questions: What type of pain is the patient experiencing? Chronic or Acute List at least 4 questions that should be included in your pain assessment What tools are available to assist you with your pain assessment? Which tool would you choose in this scenario? Why? What pain scale rating would you give the patient? List 2 possible nursing diagnosis for this patient? What interventions would be appropriate for this scenario? What type of precautions should this patient be on? What does that mean? 78 Case Study #2 Growth Assessment/ Immunizations Patient: 18 month old, white, male Chief Complaint: “Refuses to eat anything, only wants his bottles of milk” Assessment: VS- 36.5C, 125, 28, 90/60; HC-44.8cm, Wt-9.1kg, Ht-74.1cm skin pale, dry, and scaly; hair dull, dry, and sparse; pale conjunctivae, red cracks at sides of mouth, and a pale tongue, delayed in reaching milestones, sits without support and crawls some, however, does not walk; mother reports pt’s intake of milk is 40 or more ounces per day H/H-7.6/23, albumin-2.9g/dl Orders: Q4 VS, I & O, daily weights, IVF’s, CBC, glucose, cholesterol, triglycerides, and serum albumin; Regular diet as tolerated, limit milk intake to 16 ounces per day. Medications: PO Zantac ? 79 As a group please answer the following questions: What is the patient’s likely diagnosis? Please plot patients head circumference on the appropriate graph, what percentile is the patient? Please plot the patient’s height on the appropriate graph, what percentile is the patient? Please plot the patient’s weight on the appropriate graph, what percentile is the patient? Using the provided immunization chart and blank immunization record from the childrearing database, please indicate what immunizations the child should have received until now, and when the child should have received them (ages). List 2 possible nursing diagnosis for this patient? 80 81 82 Case Study #3 Patient: 8 year old, African American, male 144- Childrearing Chief Complaint: “I feel likeNUR a fish out ofOrientation water, I can’t hardly breathe” Case Study #3 Nurses Note: Assumed care of pt. at 0700. Pt. receiving continuous Albuterol neb treatment, tolerating well. Temp. 38.1 PO, Resp. 26-28; O2sats 91%-94% on 7L O2 via face mask; Moderate substernal retractions noted; no nasal flaring or grunting; b/l lungs coarse with scattered wheezes on expiration; neuro intact, PERRLA, pt. appropriate for age; pt. NPO per order, abdomen soft, non distended BS+; IVF via Left hand, infusing without difficulties, site benign; pt. voiding via bedside commode without difficulties; pt. mother at bedside active in pt care. Concept Mapping Patient: 8 year old, African American, male Chief Complaint: “I feel like a fish out of water, I can’t hardly breathe” Nurses Note: Assumed care of pt. at 0700. Pt. receiving continuous Albuterol neb treatment, tolerating well. Temp. 38.1 PO, Resp. 26-28; O2sats 91%-94% on 7L O2 via face mask; Moderate substernal retractions noted; no nasal flaring or grunting; b/l lungs coarse with scattered wheezes on expiration; neuro intact, PERRLA, pt. appropriate for age; pt. NPO per order, abdomen soft, non distended BS+; IVF via Left hand, infusing without difficulties, site benign; pt. voiding via bedside commode without difficulties; pt. mother at bedside active in pt care. Orders: Q1 hour VS, I &O’s, IVF’s(D5.45NACL @60ml/hr), NPO, Continuous pulse ox Medications: Continuous Albuterol, Tylenol, IV zofran As a group please answer the following questions: Orders: Q1 hour VS, I &O’s, IVF’s(D5.45NACL @60ml/hr), NPO, Continuous pulse ox Medications: Continuous Albuterol, Tylenol, IV zofran 1. What is the likely diagnose in this case study? 2. List 2 possible nursing diagnosis for this patient? 3. Using this case study, Please complete the provide concept map (Remember to include important assessment data, potential lab values, orders, medications, nursing interventions, and teaching points). 83 As a group please answer the following questions: What is the likely diagnose in this case study? List 2 possible nursing diagnosis for this patient? Using this case study, Please complete the provide concept map (Remember to include important assessment data, potential lab values, orders, medications, nursing interventions, and teaching points). 84 Case study #4 Concept Mapping Patient: 8 year old, African American, male Chief Complaint: “I feel like a fish out of water, I can’t hardly breathe” Nurses Note: Assumed care of pt. at 0700. Pt. receiving continuous Albuterol neb treatment, tolerating well. Temp. 38.1 PO, Resp. 26-28; O2sats 91%-94% on 7L O2 via face mask; Moderate substernal retractions noted; no nasal flaring or grunting; b/l lungs coarse with scattered wheezes on expiration; neuro intact, PERRLA, pt. appropriate for age; pt. NPO per order, abdomen soft, non distended BS+; IVF via Left hand, infusing without difficulties, site benign; pt. voiding via bedside commode without difficulties; pt. mother at bedside active in pt care. Orders: Q1 hour VS, I &O’s, IVF’s(D5.45NACL @60ml/hr), NPO, Continuous pulse ox Medications: Continuous Albuterol, Tylenol, IV zofran 85 As a group please answer the following questions: What is the likely diagnose in this case study? List 2 possible nursing diagnosis for this patient? Using this case study, Please complete the provide concept map (Remember to include important assessment data, potential lab values, orders, medications, nursing interventions, and teaching points). 86 Summary Questions What are 3 pieces of information you need from the active orders and report? Which procedures require an instructor to be present? Prior to giving an oral medication list 3 things you need to be prepared? If you are going to be late or sick and cannot attend clinical what should you do? Name 3 key items you are to review when giving report 87 Summary Questions Name 2 key items you need to obtain when receiving report? The infant assigned to you is an 8 month old. Parent is not present. Name 2 key nursing interventions. What is a good source form parent and child educational materials? What assignment is due on Wednesday each week and how is it to be submitted? 88 Any Questions? 89 90