Pathophysiology: COPD power point
advertisement

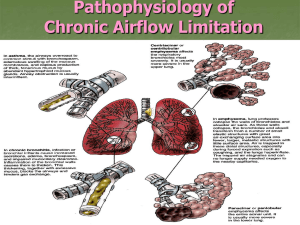
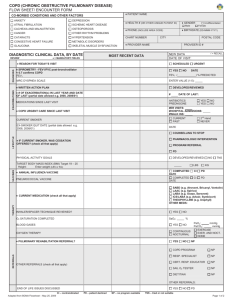
Running head: CHRONIC OBSTRUCTIVE PULMONARY DISEASE Chronic Obstructive Pulmonary Disease Mindy J. Valenti The College at Brockport State University of New York PRO 404: Pathophysiology 1 CHRONIC OBSTRUCTIVE PULMONARY DISEASE 2 Chronic obstructive pulmonary disease (COPD) is a group of progressive obstructive lung diseases including emphysema and chronic bronchitis, characterized by dyspnea and shortness of breath (SOB). Diseases involved in COPD often times over lap and only 10% of individuals with COPD have strictly emphysema (Lewis et al., 2011). COPD is a debilitating disease that affects 12.1 million Americans annually (Lewis et al., 2011). Often times, individuals are not diagnosed until significant lung damage has occurred and treatment is palliative. Background Population, Prevalence, and Cost According to the center of disease control (CDC), COPD is the fourth leading cause of death in the United States and is expected to become that worldly by 2020 (VanMeter & Hubert, 2014). The incidence of female diagnosis is on the rise partially due to the growing evidence that women are more biologically susceptible (American Lung Association, n.d.). An estimated 4.1 million Americans had emphysema and 9.5 million had chronic bronchitis in 2005 (VanMeter & Hubert, 2014). Caucasian women over 65 constitute for the highest rates of COPD (American Lung Association, n.d.). The costs of COPD take a substantial toll on the economy. In 2010, COPD cost the nation $49.9 billion (American Lung Association, n.d.). Emphysema and Chronic Bronchitis Pathophysiology Emphysema is the irreversible enlargement of alveolar due to destruction of alveolar wall elasticity and is categorized by location; panacinar (distal alveoli), paraseptal (alveoli ducts and CHRONIC OBSTRUCTIVE PULMONARY DISEASE 3 sacs), or centroacinar (bronchioles) (Higginson, 2010). The alveolar wall changes associated with emphysema causes loss of lung surface area resulting in impaired gas exchange (VanMeter & Hubert, 2014). Destruction of pulmonary capillary function and alveolar elasticity cause poor recoil thus hyperinflation of alveolar (VanMeter & Hubert, 2014). Bronchial wall damage occurs due to impaired expiration causing collapse and obstruction, thus un-oxygenated air trapping; impairing perfusion and diffusion of gasses (VanMeter & Hubert, 2014). In chronic bronchitis prolonged inflammation of the bronchi mucus membranes resulting in hyperplasia of mucus glands, which increases epithelial goblet cells and decreases cilia causing an increase in mucus production (VanMeter & Hubert, 2014). Over time, the airway narrows and becomes fibrous, causing obstruction and secretion accumulation (VanMeter & Hubert, 2014). Etiology and Risk Factors A small number of emphysema cases result from an inherited genetic deficiency of alpha1 antitrypsin protein. The protein inhibits proteases enzymes, including neutrophil elastase, which can breakdown elastic fibers in alveolar (VanMeter & Hubert, 2014). Smoking and second hand smoke are major causative agents of emphysema and chronic bronchitis. Destruction of elastin and collagen fibers by proteases occurs by reducing the function of alpha-1 antitrypsin, which diminishes elastin repair and synthesis (Lewis et al., 2011). Cilia paralysis occurs and sputum production increases and accumulates (Lewis et al., 2011). Quitting smoking can significantly prevent or delay onset of COPD. Prolonged exposure to irritants such as dust, chemicals, or air pollution can contribute to the development of COPD. Normal age related structural changes lead to loss of elastic fibers in alveolar (Lewis et al., CHRONIC OBSTRUCTIVE PULMONARY DISEASE 4 2011). Severe infections can reduce lung function eventually leading to or worsening COPD (VanMeter & Hubert, 2014). While they can occur separately, emphysema and chronic bronchitis frequently occur together in COPD and can be associated with other conditions such as asthma or cystic fibrosis. Presenting Signs and Symptoms Emphysema and chronic bronchitis have many overlapping signs and symptoms such as dyspnea, anorexia, and extreme fatigue but major differences exist. Emphysema has been coined the term “pink puffer” due to compensatory hyperventilation with pursed lip breathing to relive hypoxemia is early stages, hyperinflation resulting in barrel chest, and diaphragm flattening from hyperinflation causing accessory muscle breathing (Lewis et al., 2011). Tripod positioning optimizes respiratory efforts. Patients with emphysema often have a thin appearance, as heart failure usually does not occur until late stages when hypoxic vasoconstriction occurs (Higginson, 2010). Patients with chronic bronchitis or “blue bloaters” are characterized by hypoxemia, hypercapnea, and productive cough with thick mucus and rhonchorous lung sounds which cause cyanosis (VanMeter & Hubert, 2014). Heart failure occurs earlier in chronic bronchitis causing edema. Complications and Prognosis Emphysema and chronic bronchitis often times result in similar complications and prognosis as disease advances into late stages. Prolonged hypoxia causes polycythemia, an increase in red blood cell production, which increases blood viscosity and pulmonary vasoconstriction in attempt to compensate low oxygen (Lewis et al., 2011). Acidosis and hypercapnia cause further vasoconstriction, increasing vascular resistance (Lewis et al., 2011). CHRONIC OBSTRUCTIVE PULMONARY DISEASE 5 Eventually, pulmonary hypertension increases pressure of the right heart chambers resulting in ventricular hypertrophy, cor pulmonale, and right sided heart failure (Lewis et al., 2011). Disease exacerbation can occur due to infection or increased exposure to irritants and is characterized by an acute increase in patients usual symptoms (Lewis et al., 2011). While there is not cure for COPD, management and control is possible but early detection is crucial. Diagnostic Criteria and Testing Spirometer testing along with presenting symptoms can diagnose COPD. Forced expiratory volume in 1 second (FEV1) and forced vital capacity (FVC) ratio decreases and increase in residual volume occurs in COPD (Lewis et al., 2011). FEV1 and FVC ratio 70 percent of less can diagnose COPD. Arterial blood gas (ABG) testing in late stages or in acute exacerbations can indicate severity (Lewis et al., 2011). Carbon dioxide tension (PaCO2) is high, arterial oxygen tension (PaO2) is low, bicarbonate (PaHCO3) is high, and potential hydrogen (pH) is low (Lewis et al., 2011). Chest x-rays, like pulmonary function tests, are used to monitor residual volume, FVC, and FEV 1 and can show bullae or large air spaces if present (Lewis et al., 2011). Treatment Therapies and Limitations One of the best strategies an individual with COPD can take is to avoid irritants such as smoking as doing so will slow the progression of the disease or prevent its occurrence. Avoiding infection by immunizing against influenza and pneumonia can slow progression and prevent exacerbation (VanMeter & Hubert, 2014). Hypoxic drive eventually develops in individuals with COPD in which oxygen (O2) chemoreceptors rather than carbon dioxide (CO2) chemoreceptors trigger respirations (VanMeter & Hubert, 2014). Oxygen may be useful as CHRONIC OBSTRUCTIVE PULMONARY DISEASE 6 COPD advances but oxygen saturation levels should be kept at low-normal levels to maintain hypoxic drive and therefore should be monitored closely (Higginson, 2010). Pulmonary rehabilitation provides techniques to increase endurance in patients with COPD through breathing exercises and workouts (Higginson, 2010). Lung volume reduction surgery (LVRS) can reduce dyspnea by reducing hyperinflation but recovery can be long with a high risk of complication (VanMeter & Hubert, 2014). Bronchodilators assist in opening airways by relaxing smooth muscle. Corticosteroids can decrease inflammation in acute exacerbations but should not be used long term. In chronic bronchitis, use of expectorants or chest physiotherapy may be useful in eliminating excess mucus (VanMeter & Hubert, 2014). Research Use of corticosteroids in the treatment of COPD exacerbation is a standard of care. Global Initiative for Chronic Obstructive Lung Disease (GOLD) criteria recommends a 10 to 14 day glucocorticoid treatment plan of 30 to 40 mg/d (Asher & Monsey, 2014). A recent study revealed that a five-day non-tapered course of 40 mg of prednisone was just as good as a 14-day tapered regimen and time elapse between exacerbations was the same in most patients (Asher & Monsey, 2014). Use of steroids can have poor long-term complications such as increasing infection risk; decreasing usage could have potential long-term benefits for patients with COPD. Conclusion COPD is an elaborate and destructive disease to which there is no known cure. Much information remains unknown about the cause and cure but research suggests genetic biomarkers could eventually help shed light. This writer learned a great deal about the diagnosis of COPD using pulmonary function testing and the differences between emphysema and chronic bronchitis. CHRONIC OBSTRUCTIVE PULMONARY DISEASE 7 References American Lung Association. (n.d.). American Lung Association. Retrieved June 16, 2014, from http://www.lung.org/ Asher, G., & Mounsey, A. (2014). Steroids for acute COPD--but for how long?. The Journal of Family Practice, 63(1), 29. Higginson, R. (2010). COPD: pathophysiology and treatment. Nurse Prescribing, 8(3), 102-110. Lewis, S., Dirksen, S. R., Heitkemper, M., Butcher, L., & Camera, I. (2011). Obstructive Pulmonary Disease. Medical-surgical nursing: assessment and management of clinical problems (8th ed., pp. 610-630). St. Louis, Mo.: Elsevier/Mosby. VanMeter, K & Hubert, R. (2014). Respiratory System Disorders. Gould's Pathophysiology for the Health Professions (Fifth ed., pp. 303-312). St. Louis: Elsevier Saunders.