Paeds Revision Notes
advertisement
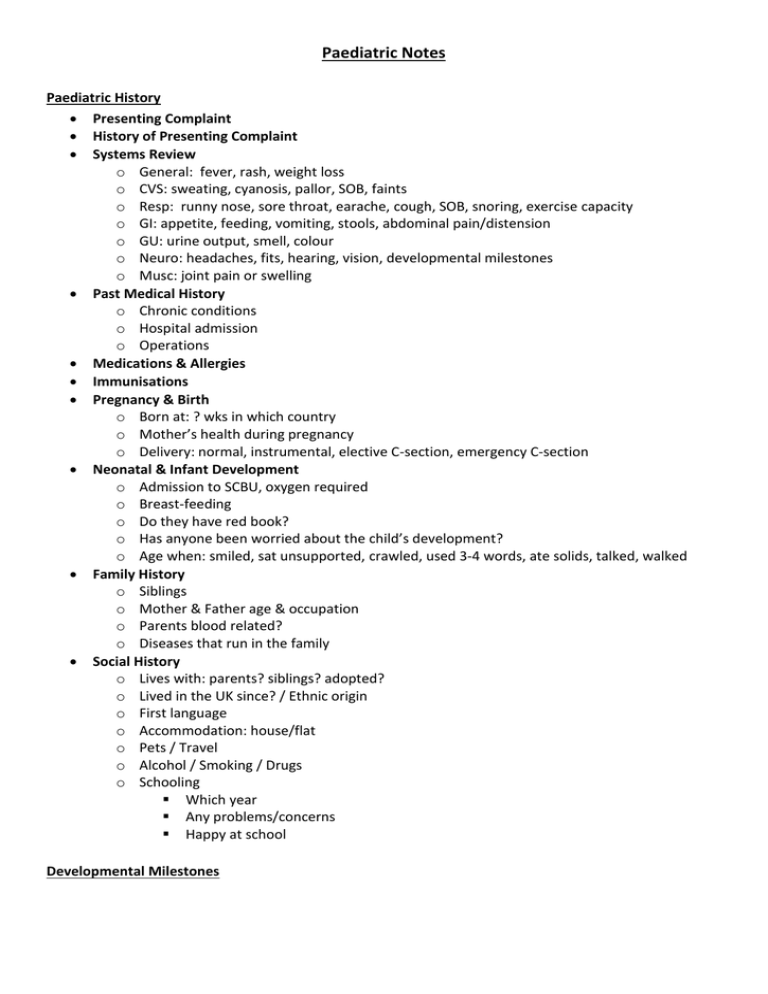
Paediatric Notes Paediatric History Presenting Complaint History of Presenting Complaint Systems Review o General: fever, rash, weight loss o CVS: sweating, cyanosis, pallor, SOB, faints o Resp: runny nose, sore throat, earache, cough, SOB, snoring, exercise capacity o GI: appetite, feeding, vomiting, stools, abdominal pain/distension o GU: urine output, smell, colour o Neuro: headaches, fits, hearing, vision, developmental milestones o Musc: joint pain or swelling Past Medical History o Chronic conditions o Hospital admission o Operations Medications & Allergies Immunisations Pregnancy & Birth o Born at: ? wks in which country o Mother’s health during pregnancy o Delivery: normal, instrumental, elective C-section, emergency C-section Neonatal & Infant Development o Admission to SCBU, oxygen required o Breast-feeding o Do they have red book? o Has anyone been worried about the child’s development? o Age when: smiled, sat unsupported, crawled, used 3-4 words, ate solids, talked, walked Family History o Siblings o Mother & Father age & occupation o Parents blood related? o Diseases that run in the family Social History o Lives with: parents? siblings? adopted? o Lived in the UK since? / Ethnic origin o First language o Accommodation: house/flat o Pets / Travel o Alcohol / Smoking / Drugs o Schooling Which year Any problems/concerns Happy at school Developmental Milestones Gross Motor Newborn 6 weeks Fine Motor & Vision Limbs Flexed Head Lag Primitive reflexes Raise Head (4mths) Primitive reflexes 6 months Sits without support (9mths) 10 months Crawls Cruises 12 months Unsteady braod based gait Steady walking 18 months 2 years Fixes & follows moving object (3mths) Reaches for toys Palmar grasp Transfers (8mths) Pincer Grasp 3 block tower 6 block tower Draws a straight line Hearing, Speech & Language Startles to noise Social Smiles Responsively Vocalises Turns to sounds out of sight Parents can discriminate sounds 2-3 words Puts food in mouth Stranger awareness Waves bye-bye Peek-a-boo Drinks from cup 6-10 words Uses a spoon to eat 2-3 word sentences Symbolic play and potty trained Primitive Reflexes Reflex Moro Eliciting Sudden head extension Description Symmetrical extension then flexion of all 4 limbs Grasp Place object in palm of hand Flexion of the fingers of the hand around object Rooting Stimulus near mouth Turning of head towards stimulus Placing Hold infant vertically and place Child steps with one foot then the the dorsum of feet on a hard other surface Positive Supporting reflex Infant held vertically, feet on a Legs support body weight, may surface push up against gravity Atonic Neck reflex Head turned to one side whilst Fencing posture with arm supine outstretch in the direction of the head N/B - these reflexes should be gone by 6 months Immunisation Schedule Age Birth 2 Months 3 Months 4 Months 12 Months 13 Months Vaccnations BCG & Hep B (to high risk Groups) Diptheria, Tetanus, Pertusis, Polio, Hib, Pneumococcal Diptheria, Tetanus, Pertusis, Polio, Hib, Men C Diptheria, Tetanus, Pertusis, Polio, Hib, Pneumococcal, Men C Hib, Men C MMR, Pneumococcal 4 Years 12 – 13 Years 13 – 18 Years Diptheria, Tetanus, Pertusis, Polio, MMR HPV Diptheria, Tetanus, Polio NEONATES < 28 days old Full term preg is 37-42 weeks Pre-term preg is < 37wks. Post term > 42 wks. Low BW <2.5kg, V .low BW <1.5kg, extremely low BW <1kg Infections of the newborn ↑ risk if PROM (>24h), chorioamnionitis, preterm Organisms: Group B Strep, Listeria Monocytogenes, Candida Albinans, HSV Neonatal sepsis Temp instability - fever, hypothermia Poor feeding Abdo distension Vomiting Apnoea BC Resp distress Pallor/mottled skin Jaundice Neutropenia Hypo-perglycaemia Shock Irritability Seizures Ix/Rx: septic screen: FBC, blood culture, CRP, urine/CSF M,C,S + CXR IVABs: o Penicillin/amoxicillin for group B strep, listeria o Ceph for gram -ve bacteria. Rubella Routine antenatal screening for rubella IgM. Live Vacine before birth if neg. Complications: o <8/40: sensorineural deafness, congenital HD, cataracts/glaucoma, hepatosplenomegaly, dev delay/IUGR. o 13-16/40: impaired hearing (30%) o >18/40: minimal risk CMV Most common 40% of infants infected in maternal infection o 90%: normal at birth and development o 5%: clinical features of infection at birth: IUGR HSmegaly Petechiae Pneumonitis Jaundice Deafness Encephalitis/micro encephaly/IC calcification IQ Malformations of the Neonate Down’s syndrome (trisomy 21) 1 in 1000 LBs Sx: o Newborn: ++nuchal skin, hypotonia, sleepy o Facial appearance: round face, epicanthic folds, protruding tongue, upslanting palpebral fissures, small low set ears o Other anomalies: flat occipital, single palmar creases, incurving 5th digit, saddle gap Complications: o Learning diff o Vision/hearing impairment o Congenital HD o Hypthyroid o Duodenal atresia o Leukaemia o Recurrent resp inf o Alzeheimers Patau’s Syndrome (trisomy 13) 1 in 14000 LBs Sx: o Small head and eyes o Absent corpus calloscum with single ventricle o Heart lesion o Polycystic kidneys o Cleft lip/palate o Hands show flexion contractures +/polydactyl Edward’s syndrome (trisomy 18) 2nd commonest trisomy Female 2:1 male Sx: o Rigid baby + limb flexion o Odd low set ears o Receding chin o Proptosis (forward displacement of eyes) o Rocker bottom feet o Cleft lip/palate o Umbilical/inguinal hernia o Short sternum (therefore widely spaced nipples) o Mean survival 10/12 Turner’s syndrome (45X) >95% result in early miscarriage 1 in 2500 LBs Females only Sx: o Lymphoedema of hands and feet (neonate) o Short stature; webbed neck o Wide carrying angle (cubitus valgus) o Widely spaced nipples Dx: o Detect on USS - cystic hygroma and oedema Rx: o GH and oestrogens Klinefelter’s syndrome (47, XXY) 1-2 in 1000 LBs Males only o Congenital HD (esp coarctation of the aorta) o Ovarian dygenesis (infertility) o Normal interlectual development Sx: o Infertility (commonest presentation) o Hypogonadism and small testes o Gynaecomastia in adolescence o Tall stature o N intelligence but psychological probs Microdeletion syndromes Cri du chat syndrome: High-pitch mewing cry in infancy, CVS abnorms, Microencephaly, Widely spaced eyes, ‘moon’ face Di George: Congenital HD, cleft palate, thymus William’s: Usually sporadic, face - epicanthic folds, small ears, stellate eyes Angelman’s: Maternal deletion. ataxia, seizures, microencephaly Prader-willi: Hypotonia, obesity, hypogonad, dev delay Preterm infants Respiratory distress syndrome (RDS) Due to surfactant def Most babies <28/40 effected Rare at term Rx: o Antenatal corticosteroids (need 24h to act) o Exogenous surfactant: via ET tube, decreasing mortality by 40% o CPAP: increases end exp press. Intubation + ventilation Pneumothorax In RDS air from overdistended alveoliinterstitium Present in 20% of ventilated infants Sx: o TV o O2 requirement Rx: o Chest drain o breath sounds/exp o Preventable by ventilating with low press Apnoea and bradycardia Temp control Large SA:vol ratio Little subcut fat PDA May need inotrphic support. Rx with fluid restriction + indomethacin (prostaglandin synthase-I) Hypotension Nutrition high nutritional requirement for rapid growth (Suckling reflex develops at 34/40) NG tube, Pref breast milk Consider parentral nutrition Supplement with phosphate, Ca and Vit D (bone mineralization) Anaemia of prems Fe transferred in last trimester Blood loss from blood samples + inadequate erythropoietin Infection Increased risk (esp group B strep and coliforms) Intracranial lesions Interventricular hemorrhage o High risk if: asphyxia, RDS, pneumothorax Post-haemorrhage hydroencephalus o Sutures separate, incraesed HC, bulging fontanelle o Rx: LP/ventricular tap, shunt Periventricular leucomalacia o Due to ischaemia o High risk if: inf, hypoT, MZ twins sharing placenta Renal Low renal flow in fetus. At 28/40 GFR=25% of term. Doubles in 1st 2/52 of life Necrotizing enterocolitis (NEC) Bowel wall ischaemia (gut microorganisms to colonise bowel wall) Sx: o No feeding o Distended abdo o Milk aspirations o Blood in stool o Vomiting (bile stained) Can cause shock if haemorrhagic colitis AXR: shows distended bowel + air in bowel wall/portal tract Rx: stop feeding, IVABs, ventilate/circ support, surgery (if perforated) Complications: strictures, short bowel syndrome (malabs) Retinopathy of prematurity (ROP) Common (50%) Can cause retinal detachment, fibrosis, blindness (in 1%) Screen all v. low BW at 6-7/52 with opthalmoscopy Rx: Cryotherapy/laser Rx GOR Inguinal hernias Metabolic Hypoglycaemia: maintain BM (>2.6mmol/L) to prevent neurodamage Hypocalcaemia Electrolyte imbalance: due to poor renal function and por resorption Osteopenia of prems: therefore give ca, phosphate, Vit D Bronchopulmonary dysplasia/chronic lung disease If infant has prolonged O2 requirements (beyond 36/40) Lung damage is from: press/vol trauma from ventilation, O2 toxicity, inf, ++lung secretion CXR shows: areas of opacification + cystic change Wean infants onto CPAP Complications: inf, cor pulmonale The consequences of traumatic delivery Injury occurs if baby: o Malpositioned o Too large for pelvic outlet o Manual manoeuvres o Forceps o Ventouse Soft tissue injuries Caput succedaneum - presents immediately, oedema of scalp, superficial to periosteum, resolves spontaneously Cephalhaematoma - bleed below periosteum within skull sutures, fluctuant + slower to develop, resolves over wks, may cause/contribute to jaundice Chignon - large caput from ventouse Bruising – face, genitalia/buttocks if breech, Prems bruise easily Abrasions - from scalp electrodes Subaponeurotic heamatoma – rare, ++blood loss between aponeurosis + periosteum Nerve palsies Erb’s palsy - upper N root injury (C5 + C6). Straight arm, limp pronated hand. Lower roots injury - less often. Weak wrsit extensor and intrinsic muscles of hand. Fractures Clavicles - from shoulder dystocia, may hear snap or see lump/callus Humerus/femur - usually mid shaft occurring in breech. Heal quickly if immobilised Neonatal jaundice Yellow pigmentation of skin/whites of eyes, due to a high bilirubin in plasma Clinically jaundiced = >80-120mol/L Jaundice <24h Rhesus haemolytic disease ABO incompatibility G6PD deficiency Jaundice 24h - 2wks of age Physiological - UNCONJUGATED Breast milk jaundice - UNCONJUGATED Infection - UNCONJUGATED Other causes Persistent jaundice (>2weeks) UNCONJUGATED: Breast milk jaundice - 15%, disappears by 3-4/52 Infection - UTI Congenital hypothyroidism CONJUGATED (dark urine, pale stools): Neonatal hepititis syndrome Biliary atresia: Management: Hydration Phototherapy Exchange transfusion Respiratory distress Signs: o Tachypnoea o Laboured breathing o Expiratory grunting o TC o Cyanosis Admit to SCBU Monitor: HR, RR, sats, circ CXR Causes o Transient tachypnoea of the newborn o Meconium aspiration o Pneumonia o Pneumothorax o Milk aspiration o Persistent pulmonary HT of the newborn o Diaphragmatic hernia The childhood exanthems Measles Cause: RNA paramyoxovirus Spread: Droplets Incubation: 7-21 days Sx: Prodrome (catarrh, wretchedness, conjunctivitis, fever) Conjunctiuvae look glassy, then semilunar fold swells (Meyer’s sign). Koplik spots are pathognomonic, often fade as the rash appears (starts behind ears on day 3-5, then spreads down body becoming confluent). Complications: Febrile fits, otitis media, meningitis, D&V, keratoconjunctivitis, immunosuppression, subacute sclerosing panencephalitis. Worst complication is encephalitis (headache, lassitiude, fits coma), 15% may die. Treatment: Isolate in hospital. Ensure adequate nutrition. Treat 2º bacterial inf e.g. Amoxicillin Immunisation: MMR Chickenpox (Varicella Zoster virus) Presentation: Crops of vesicles of diff ages on the skin, typically starting on back. Incubation: 11-21 days Infectivity: 4 days before the rash until all lesions have scabbed (1 wk) Spread: Droplet. Immunity is life-long. Tests: Fluorescent Ab tests and Tzanck smears rarely needed. Course: Treatment: Complications: Immunisation: Fever, rash (2 days later). Macule, papule, vesicle Keep cool, daily antiseptic for spots, trim nails, Flucloxacillin if bacterial inf. Anti-VZV Igs + acyclovir if immunosuppressed or on steroids. If spots blackish (purpura fulminans) or coalescing and bluish (necrotising fasciitis) With live-attenuated vaccine if pre-cytotoxics/steroids. Rubella (german measles) Cause: RNA virus Incubation: 14-21 days Infectivity: 5 days before and 5 days after rash starts Signs: Usually mild, macular rash, suboccipital lymphadenopathy Treatment: Symptomatic Immunization: Live virus Complications: small joint arthritis. Malformations in utero. RESPIRATORY SYSTEM Asthma Reversible airway obstruction with wheeze, dyspnoea or cough. RF: o Male o Atopy o Past bronchopulmonary dysplasia o BW o Passive smoking o Family Hx o Bottle fed Presentation: o Recurrent wheeze o Nocturnal cough o Cough and breathlessness o Eosiniophilia and serum IgE Diagnosis: o Hyperinflation of chest (pectus carinatum and Harrison’s sulcus) o Generalised exp wheeze with prolonged exp phase o Signs of atopy Ix: o Skin tests o PEFR (in over 5yrs) o CXR (hyperinflatio) Management: o High-dose inhaled B2 bronchodialtor (Salbuatmol or Terbutaline) o Ipratropium nebulised o O2 if low sats o IV aminophylline or salbutamol o IV hydrocortisone Cystic fibrosis Autosomal recessive disorder. Mutations in the CF transmenbrane conductance regulator gene (CFTR) o Abnorm ion transport across epithelial cells of exocrine glands of resp tract and pancreas Clinical features: o Malabs + FTT from birth + recurrent/persistent chest inf. o Meconium ileusinspissated meconium causes intestinal obst + vomiting + abdo distension + failure to pass meconium o Malabs and steatorrheoa due to insufficiency of pancreatic Management: o Genetic counselling o Inhaled salbutamol for reversible airway o Abs obst o Good nutrition o Lung transplant? o Pertussis, MMR and pneumococcal o Synthetic Es (pancrex) vaccination o Cimetidine (H2-R antagonist) o Physio 3xday o Vit supplements o High calorie/protein diet Pertussis Specific and highly infectious form of bronchitis, caused by Bordetella pertussis. Signs: o Bouts of coughing ending with vomiting (+/- cyanosis), o Worse at night and after feeding o Whoop (not always present) is caused by inspiration against a closed glottis. Peak age: 3yrs Incubation: 10-14days Complications: o Prolonged illness o Hernias o Petechiae o Bronchiecttasis o Microhaem Rx: o Erythromycin to exposed infants o Live vaccine at 2 months o Admit if <6/12 old Bronchiolitis Typical cause: winter epidemics of RSV Signs: o Coryza (coldlike Sx) o Sharp, dry cough o Low fever o Tachypnoea o Wheeze (high pitched exp>insp) Diagnosis: o Immunoflourescence of nasopharyngeal aspirates o CXR shows hyperinflation of the lungs Management: o Admit if feeding diff Should recover in 2 weeks Prevention: o Monoclonal AB to RSV given to at risk Pneumonia Signs: o Fever o Malaise o Feeding diff o Tachypnoea o o o o Apnoea Intercostal recession +/- cyanosis Hyperinflation of chest Fine end-insp crackles o Supportive care o o o o Cyanosis Grunting on exp. Consolidation CXR changes Management: o Abs (oral or IV penicillin and erythromycin) o May need O2 TB Signs: o Anorexia o Malaise o Prolonged low fever o Cough o Failure to thrive Diagnosis: o Screen with heaf test o CXR: consolidation, cavities, miliary spread o Diagnose with Mantoux test Treatment: o 6/12 of triple therapy (Rifampicin, isoniazid and pyrazinamide) o Dropped to Rifampicin & isoniazid after 2/12. o BCG given to at risks at birth Croup (laryngotracheobronchitis) >95% of laryngotracheal infections Parainfluenza viruses commonest cause, also RSV Peak age 2yrs Sx: start and worse at night. If severe can treat with oral dex, nebulised steroids and adrenaline Acute Epiglottitis Med Emergency Caused by H. influenzae type B (incidence due to Hib vaccine) Secure airway, take bloods for culture, start IV Abs (2nd or 3rd generation cephalosporins) Common cold (coryza) Classsical features: clear or mucopurulent nasal discharge + nasal blackage Commonest pathogens = viruses: rhinoviruses, coronaviruses and RSV. Sore throat (pharyngitis) Usually due to viral inf with respiratory viruses (adenovirus, enterovirus, rhinovirus) Pharynx and soft palate are inflammed + local lymph nodes are enlarged + tender Tonsillitis Form of pharyngitis with intense inflammation and purulent exudate Common pathogens: group A -H. Strep and the EBV Marked constitutional disturbances e.g. headache, apathy, abdo pain ABs (penicillin or erythromycin) Avoid amoxicillin Red Ear Otitis externa (swimmers ear): pain, discharge due to inflammation of the skin of the meatus. Pseudomonas common organism. Aural toilet is the key to treatment. Otitis media: inflammation of the middle ear and classified on timing: acute, subacute and chronic. o Rx: paracetamol and ABs (amoxycillin/augmentin) o Complications: COM, mastoiditis, meningitis, cerebral abscess Foreign bodies. CARDIOVASCULAR SYSTEM Innocent murmur Heard in up to 30% of all children Ejection murmur Generated in ventricles, outflow tracts or great vessels on either side of heart by turbulent blood flow No structural abnormalities Soft blowing syst murmur, localised to L-sternal edge, no diastolic component, no radiation Venous hum Turbulent blood flow in head and neck veins Disappears when lying flat or compressing ipsilateral jug V Acyanotic congenital heart lesions VSD: o Sx: asymptomatic, heart failure, recurrent chest inf, cyanosis, endocarditis o Signs: parasternal thrill, harsh loud pansystolic ‘blowing murmur’, tachyop, tachycardia, enlarged liver o Ix: CXR=heart, pul A, pul vascular markings. ECG=ventricular hypertrophy, upright T wave=pul HT. o Course: 20% close in 9/12. Diuretics and ACE-Is. Surgery if pul HT as can cause pul vascular disease. ABs to prevent bacterial endocarditis. o o o PDA: Common in prem Left to right shunt (aortapul A) Signs: FTT, pneumonias, heart failure, collapsing pulse, thrill, S2, continuous murmur beneath Lclavicle o Ix: CXR: vasc markings, enlarged aorta. ECG: usually N, LVH o Rx: most close over time. Dex in preterm labour. If symptomatic, Rx with fluid restriction, diuretics, indomethacin (a prostaglandin synthetase inhibitor). Surgical ligation or transvenous occlusion with coil device. o o o ASD: Special form of VSD, often seen in kids with Down’s syn. Signs: widely split, fixed S2 and midsystolic murmur (2nd IC space of L sternal edge) Ix: CXR: cardiomegaly, globular heart (primum defects). ECG: RVH +/- incomplete RBBB o o o o o Coarctation Associated with other lesions e.g. bicuspid aortic valve and VSDs. Neonates present with duct-dependent circ Sx: circulatory collapse when duct closes, heart failure, murmur between shoulder blades. Signs: diff in feeling femoral pulses, BP in arms, BP in legs, no foot pulses Ix: CXR: rib notching (late), due to large collateral IC As running under ribs posteriorly to bypass obstruction. ECG: RVH in neonate, LVH in older child o Rx: surgical: resection and end to end anastomosis or balloon dilatation. Cyanotic congenital heart lesions Tetralogy of Fallot o 4 cardinal anatomical features: Large outlet VSD Overriding of the aorta with respect to the ventricular septum RV outflow tract obstruction (pul stenosis) RVH o Signs: cyanosis as ductus closes, hypercyanotic spells, dyspnoea, faints, squatting at play, clubbing, thrills, absent pulmonary part of S2, long, loud ejection systolic murmur at L sternal base. o Ix: FBC: Hb CXR: small heart, uptitling apex (RVH), pulmonary artery ‘bay’. ECG: RVH and RAD (R axis deviation) Transposition of the great arteries o When there are 2 parallel circulations: no mixing is incompatible with life (ass. Anormalities) o Sx: usually present day 1 or 2 of life with cyanosis o Signs: cyanosis, clubbing, CCF +/- systolic murmur. o Ix: CXR: narrow pedicle, ‘egg on side’, pul vasc markings. ECG: RVH. Echo: diagnostic o Rx: prostaglandin infusion to keep ductus arteriosus open. Life-saving balloon atrial septostomy NEUROLOGY Epilepsy Tendency to intermittent, abnormal electrical brain activity Causes: o 70-80% idiopathic, o Cerebral tumour o Neurodegenerative disorders o 2to cerebral dysgenesis o Neurocutaneous syndromes o Cerebral damage Generalised epilepsies: o Status epilepticus: multiple seizures, no recovery of consciousness in between o Absence, tonic or tonic-clonic seizure disorders may remit; identification of the epilepsy syndrome involved allows a more accurate prognosis o Atonic and myoclonic seizures may accompany cerebral dysgenesis or a neurodegenerative disorder and have a poor prognosis Localisation-related epilepsies (focal or partial): o May arise from any of the 4 lobes o Temporal lobe is most common: ‘complex phenomena’: conciousness, automatisms, deja vu, jamais vu o Frontal lobe involves motor cortex, patiel tonic, clonic movements o Occipital lobe gives rise to distorted vision o Parietal lobe contralateral dysaesthesias, vertigo + distorted body image Epilepsy syndromes o Infantile spasms (west syndrome): between 4-6/12, violent flexor spasms of head, trunk, limbs followed by extension of arms (‘salaam spasms’). Rx with vigabatrin or corticosteroids. Later learning disability and/or epilepsy common. o Typical (petit mal) absence seizures: 1-2% of childhood epilepsy. onset 4-12yrs. Induced by hyperventilation. Good prognosis, 95% remission in teens Meningitis Confirmed by inflammatory cells in the CSF Causes: viral are most common and are self-resolving. Bacterial may have severe consequences. Other causes of meningitis inc: malignancy + autoimm diseases. Bacterial Meningitis Usually follows bacteraemia. Host response to infection causes most damage. Inflam mediators, activated leucocytes & endothelial damage cause cerebral oedema, IC press and cerebral blood flow. Organisms: o < 3 Months: group B strep, E.coli, coliforms, Listeria monocytogenes o < 6yrs: Neisseria meningitidis (meningococcus), strep pneumoniae, H. influenzae o >6yrs: Neisseria meningitidis, strep pneumoniae Presentation: o Meningeal signs: stiff neck, photophobia, opisthotonos o IC press: irritable, high-pitch cry, drowsy, vomiting, fontanelle tense (late sign) o Septic signs: fever, arthritis, odd behaviour, purpuric rash (in meningococcus), cyanosis, DIC, ++WCC o Shock: tachycardic, hypotensive, poor capillary refill time, oliguria Ix: CSF (confirms Dx, identifies organism + AB sensitivity). Bloods, throat swab, rash scraping Rx: o 3rd generation cephlosporin (cephotaxime or ceftriaxone). o Ampicillin in <3/12 olds o Dexamethasone reduces long-term complications Complications: o Hearing loss o Hydroencephalus o Ataxia o Subdural effusions o Brain abscess o Mental retardation o Disseminated disease o Paralysis o Epilepsy Cerebral Palsy Comprises a range of chronic disorders of posture and movement caused by non-progressive CNS lesion sustained before 2 yrs old, resulting in delayed motor development, evolving CNS signs +/- learning disability +/- epilepsy. Causes: o Antenatal (80%): cerebral dysgenesis + malfornation, congen inf -rubella, tox, CMV o Intrapartum (10%): birth asphyxia/trauma o Postnatal: IVH, meningitis, trauma. Clinical presentation: o Abnormal tone and posture o Feeding difficulties o Delayed motor milestones o Abnormal gait once walking o Developmental delay (language and social skills) Spastic (70%) Damage to upper motor neurone (pyramidal or corticospinal) pathway limb tone (spasticity), deep tendon reflexes + extensor plantar response distribution of signs: o Hemiplegia o Diplegia o Quadreplegia Ataxic hypotonic (10%) Signs usually symmetrical Early hypotonia, poor balance, delayed motor development Later incoordination movements and intention tremor (cerebellum dysfunction) Dyskinetic (10%) Leading to constant involuntary movements and poor postural control Intellect may be relatively unimpaired Damage to basal ganglia and associated pathways (extrapyramidal) Intracranial neoplasms IC press with focal signs +/- false localising signs Sx of ICP: o Headache (worse on lying down) o Vomiting o Papilloedema o Squint (due to VIth N palsy) o Nystagmus o Ataxia o Behaviour change Myopathies The muscular dystrophies Duchenne’s muscular dystrophy: o X-linked recessive disorder o Peak age of Dx = 5.5yrs o Waddling gait, climb stairs one by one, ‘Gower’s sign’ + pes cavus o Progressive, in wheel chair at 10-14yrs, death ensues late teens, early 20s. Becker’s muscular dystrophy: o Some functional dystrophin is produced o Slower progression. Dx at 11yrs, wheel chair late 20s, death 40s Congenital muscular dystrophies: o Present with muscle weakness at birth/ early infancy The inflammatory myopathies Benign acute myositis: follows URTI, self-limiting course, pain and weakness. Dermatomyositis: gradual onset, ascending muscle weakness. Heliotrope rash. Post-exercise aches and pains Myotonic disorders Dystrophia myotonia: inherited. Hypotonic baby, but classically presents in school age with learning diff, expressionless face, distal wasting and myotonia. Metabolic myopathies Present as floppy infant or in older child with muscle weakness + cramps on exercise Congenital myopathies Presenting at birth or in infancy with generalised hypotonia and muscle weakness Categorised according to appearance of muscle Bx Headache Causes of acute headache include: o Febrile illness o Head injury o Migraine o Benign intracranial HT o Stress o Drugs inc alcohol o Acute sinusitis o Subarachnoid/intercerebral haemorrhage o Meningitis/encephalitis o Temperomandibular pain Causes of recurrent headaches: o Tension headache: symmetrical, gradual onset, tightness (band), frequent o Migraine: sudden onset, unilateral, visual and GI disturbances o ICP: headache worse when lying down, vomiting in a.m. Ix: CT/MRI if ICP suspected. Rx: advice, reduce stress. Mild analgesics, anti-emetics if vomiting. Prophylaxis for migraine ENDOCRINOLOGY IDDM Genetic predisposition and environmental precipitants AI process which damages -cells in pancreas leading to absolute I def Associated with other AI disease e.g. hypothyroidism Dx: symptomatic child with raised random blood glucose (>11.1mmol/L) or fasting blood glucose of >7.8mmol/L and raised HbA1c Presentation o Most common: polydipsia, polyuria, wt loss o Less common: enuresis, skin sepsis, candida and other infections DKA Insulin def Aetiology: poor control, poor adherence, illness (inf), initial presentation I causes: o Hyperglycaemia: hepatic production, uptake, proetolysis o Osmotic diuresis: loss of water and electrolytes o Dehydration: due to osmotic diuresis. Dehydration causes: CCA,cortisol,GH,AVP o Ketosis: due to lypolysisFFsketone production o Acidosis: due to ketones. Therefore metabolic acidosis +/- resp compensation Presentation o Acetone on the breathe o Hyperventilation (kussmaul breathing) o Vomiting o Hypovolaemic shock o Dehydration o Drowsiness o Abdo pain o Coma Hypothyroidism Congenital hypothyroidism Common and Rxable (i.e. preventable cause of learning diff). Causes: o Maldescent of thyroid and athyrosis o Dyshormonogenesis o Iodine def: o Hypothyroidism due to TSH def: Clinical features: o FTT o Pale, cold, mottled skin o Feeding probs o Coarse facies o Prolonged jaundice o Large tongue o Constipation o Hoarse cry Rx: lifelong oral thyroxine, titrating dose to maintain N growth, TSH and T4 Juvenile hypothyroisism Usually caused by AI thyroiditis More common in girls Clinical features: o Short stature/growth failure o Cold intolerance o Dry skin o Cold peripheries o Bradycardia Rx: thyroxine o o o o o o Thin,dry hair Pale, puffy face Goitre Slow relaxing reflexes Constipation Delayed puberty o Goitre (occasionally) o Umbilical hernia o Developmental delay o Obesity o Slipped upper epiphysis o Deterioration in school work o Learning diff CAH AR disorder. More common in consanguineous marriages Abnormal adrenal steroid biosynthesis. Cortisol defACTHadrenal hyperplasia + androgens Presentation o Female virilisation: clitoral hypertrophy, variable fusion of labia o Male: enlarged penis. If a non-salt loser may present with tall stature, PP o Salt-losing adrenal crisis in males presents in 1-3weeks with vomiting, wt loss, floppiness and circ collapse Dx: o metabolic precursor 17 OH-progesterone o Salt losers (pNa, pK, metabolic acidosis, hypoglycaemia in crisis) Mx: o Corrective Sx o Hydrocortisone, saline + dextrose in salt-losing crisis in males GASTROINTESTINAL SYSTEM Gastroenteritis Infective diarrhoea and vomiting Rotavirus (60%) Bacterial causes are suggested when blood in stools Rx: o Fluid replacement Complications: o Dehydration o Temporary sugar intolerance o Malnutrition Tests: stools Prevention: hygiene, water and food, education, fly control. Secretory diarrhoea Causes: bacteria (campylobacter, staphylococcus, E coli, salmonella, shigella and vibro cholerae), giardiasis, rotavirus, amoebiasis, cryptosporidium. IBD. Constipation Painful passage of hard, infrequent stools Causes: o Infant: organic cause most likely o Older child: non-organic/functional cause most likely Ix: growth, general and anorectal, faeces palpable per abdomen. Bloods (exclude systemic cause). Plain abdo X-ray may show faecal loading +/- megacolon. Rx: o Treat underlying organic cause. o dietary fluids and fibre o Stool softeners (lactulose) and stimulants (senna) o Evacuate overloaded rectum (enema or manual evacuation) o Maintenance: stools should be kept soft for 3-6/12. Encourage daily sits on loo. o Parallel psychological help: encouragement by family and health team Hirchsprung’s disease Absence of ganglionic cells in largenarrow, contracted segment from rectum proximally ending in normally innervated dilated colon. Presentation: usually as neonate with intestinal obstruction (failure to pass meconium in 1st 24habdo distension + bile stained vomitus). Can present in 1st few weeks with Hirshsprung’s enterocolitis (C. diff infection), or in later childhood with chronic, profound constipation + abdo distension - soiling. Ix: DRE: may reveal narrow segment + withdrawing finger causes gush of liquid stool and flatus. Rectal Bx: diagnostic, showing aganglionic cells Management: colostomy then anastamosing normal bowel to anus. FTT Ix: o Hx: mid-parental hts, pregnancy Hx, feeding Hx o Exam: Ht, Wt, head circ, full exam, urinalysis, signs of abuse + neglect o Ix: serial measurements of wt, all bloods, stools, CXR, renal + CNS US, skeletal survey, ECG/echo, endomysial + antigliadin Abs (coeloiac), sweat test Causes: o Inadequate intake o Iatrogenic (corticosteroids) o Psychosocial deprivation o Systemic disease o Familial short stature o Endocrine o Small-for-date o Chromosomal (Down’s) o Malabsorption o Metabolic o Mental retardation Rx: of non-organic cause is multidisciplinary in 1care e.g. HV, dietician Faecal soiling Abnormal after the age of 4yrs With loaded rectum or without loaded rectum Faeces in the rectum is always an abnormal finding Loaded rectum o Poor coodination with anal sphincter relaxation o Following febrile illness o Inhibition for fear of punishment if incontinent o Anxieities about using toilet facilities Rx as you would for constipation + star charts + explain to child and parents about retention and how it leads to incontinence. Empty rectum Urgency of defecation and can’t hold it in Neuropathic bowel Diarrhoea General learning disability Child may defecate intentionally to spite parents Gastro-oesophageal reflux (GOR) Physiological, asymptomatic reflux may occur in any child/adult but is infrequent Measurements of lower oesophageal pH show that acidity for <4% of 24h is normal More than this results from functional immaturity of LOS Common in under 1yrs, then spontaneously resolves A sliding hiatus hernia is present in some symptomatic infants Severe reflux is uncommon but may be in potentially serious complications: o Cerebral palsy o Bronchopulmonary dysplasia (chronic lung disease of prematurity) o Following surgery for oesophageal atresia or diaphragmatic hernia Presentation: o Regurg o Apnoea o FTT + anaemia o Distress after feeds o pneumonia Ix: 24h oesophageal pH monitoring. Barium swallow. Endoscopy and Bx Rx: o Reassurance o Thickening agents to feeds (Carobel) o Avoid over feeding o Antacids (gaviscon) o Lie on front Drugs o Enhance gastric emptying e.g. domperidone o H2-antagonists e.g. ranitidine to reduce oesophagitis Surgery: fundoplication, oesophageal stricture, recurrent aspiration Inflammatory bowel disease (IBD) Crohn’s disease o Present with: abdo pain, diarrhoea + growth failure with pubertal delay o May also present with: oral/perianal ulcers, fever, arthritis, uveitis, erythema nodosum o Diagnosis: barium and colonscopy, ESR and CRP. Ulcerative colitis o Presents with: rectal bleeding, diarrhoea, colicky pain, wt loss o Also: erythema nodosum, pyoderma gangrenosum (acute ulcerating skin), arthritis, spondylitis (inflammation of synovial joint of backbone) Coeliac disease Gliadin fraction of gluten provokes a damaging immune response in proximal small intestine Lymphocytic infiltration and villous atrophy Presents in 1st 2yrs of life following introduction of gluten in cereals with: o FTT o Abnorm stools o General irritability o Abdo distension o Buttock wasting o Presents in later life with anaemia + growth failure Pyloric stenosis Hypertrophy of pylorus causing gastric outflow obstruction 2-7wks of age, boys 4:1 Presents with: o Projectile vomiting after feeds o Hypochloraemic alkalosis o Constant hunger o Wt loss and poor Wt gain Diagnosis: o Visible gastric peristalsis o Pyloric ‘olive’ palpable in RUQ Intussusception Invagination of proximal bowel into distal Commonest cause of intestinal obstruction in infants, usually 2 months to 2 yrs. Presentation: o Acute, severe colicky pain and pallor o Passage of red currant jelly stools o Sausage shaped mass in abdomen o Abdo distension and shock X-ray shows distended small bowel + absent gas in distal colon and rectum Rx: fluid resus and air enema. Surgical reduction if this fails. GENITOURINARY SYSTEM Nephrotic suyndrome (nephrosis) ++proteinuria albumin + oedema + hypoproteinaemia + hypercholestrolaemia Sx: o Anorexia, o Oedema (periorbital, genital), o GI disturb, o Ascites, o Infections, o Oliguria, o Irritability o Breathlessness Ix: urine (frothy, +++albumin and casts, Na , blood (albumin, urea and creatinine normal). Renal biopsy in older kids. Rx: o Low sodium diet limits oedema o Consider furosamide IV + spironolactone PO o Prednisolone (course of 3-7/12) Complications: o Hypovolaemia o Infection o Thrombosis o Hypercholesterolemia Urinary tract infection Presentation: o Newborn Sx non-specific and may develop rapidly into septicaemia. o Toddlers: present as ‘gastro-enteritis’, FTT, colic, PUO o Older child: dysuria without fever due to vulvitis in girls and balanitis in boys Collection of sample: o ‘clean catch’ in to sterile pot o Adhesive bag applied to perineum, after careful washing o Suprapubic aspiration (SPA) in severely ill child Diagnosis: culture Causes: o Infecting organism: E. Coli, Proteus, Pseudomonas o Incomplete bladder opening: infrequent voiding therefore large bladder, vulvitis, hurried micturition, obstruction from loaded rectum, neuropathic bladder. o Vesicoureteric reflux: developmental anomaly of vesicoureteric junctions therefore urine goes bladderureters. Management: o Oral AB (co-amoxiclav) or IV AB (cefotaxime or ampicillin o Preventative: avoid constipation, oral fluids, encourage full voiding Glomerulonephritis Haematuria + oliguria (+/- HT + ureamia) produced by immune mechanism in kidney Peak age 7yrs Causes: o Malignancies Strep sore throat or skin infection o Infection (viruses, SBE, syphilis) o HSP o Renal vein thrombosis o Toxins (heavy metals) o Berger’s disease Presentation: o Haematuria o Periorbital oedema o Loin pain o Oliguria o Fever o GI dist o BP Ix: o MSU: RBCs, WBCs, red cell casts o Renal US, renal Bx o Bloods: urea, ESR, acidosis, C3 titre Rx: o Restrict protein in oliguric phase o Monitor BP, treat severe HT. o Penicillin IV and then PO for strep infection Wilm’s neuroblastoma Malignant tumour composed of embryonic nerve cells Commonest intra-abdominal tumour in children Originates from embryonic renal tissue Rarely seen after 10yrs Presentation: o Abdo mass o Fever o Flank pain o Haematuria Ix: US or CT show intrinsic renal mass, mixed tissue densities Rx: avoid Bx. Nephrectomy and 4/52 chemo. Radiotherapy may help Enuresis Most children are psychologically and physically normal Different types o 1 nocturnal enuresis: common. FHx of delay in acquiring sphincter competence. o Day time enuresis: nocturnal enuresis usually also present. Common causes are lack of sensation (behavioural prob), detrusor instability (uncoordinated bladder contraction), bladder neck weakness, UTI, constipation, neurogenic o 2 enuresis: is the loss of previously achieved urinary continence, may be due to emotional upset (commonest cause), UTI, polyuria Ix: -MSU, -US, -x-ray (may show vertebral abnorm), MRI (spinal roots) Rx: o Avoid acrimonous blame, and reassurance o Enuresis alarm o Fluid restriction before bed o Desmopressin (Short term relief) o Star chart o Anticholinergic or adrenergic drugs HAEMATOLOGY Anaemia Hb below normal range for child’s age and gender. Clinical features: o Asymptomatic o Tiredness o Pallor Management: o IDA: dietary advice and oral Fe therapy o Aplastic anaemias: stem cell or BM transplant, immunosuppressive therapy, ABs Sickle cell disease Inherited disorders of Hb structure or its production. Sickle cell (HbS), homozygous state (SS) a.a substitution on codon 6 Hb molecule becomes deformed in low O2, dehydration, cold thrombosis and ischaemia Management: o Hydration o Blood and BM transplant o Warmth o Penicillin o Analgesia o Pneumococcal vaccine o Blood transfusion o Folic acid Sickle cell trait (AS) Usually asymptomatic except under v.v.low O2 tensions Sickle cell-Hb C (SC) disease Nearly normal Hb levels, few painful crisis, but may develop proliferative retinopathy Thalassaemia Syndromes are due to inherited defects of globin chain synthesis or absent chain excess of other type precipitates in RBC membrane cell death in BM and premature removal from the circ by the spleen -thalassaemia -thalassaemia major o Severe anaemia and jaundice from 6/12 + FTT + hepatosplenomegaly o Extramedullary haemopoesis BM expansion classical faces (maxillary overgrowth and skull bossing) o Rx: reg blood transfusion and chelating therapy. BM transplant is curative. -thalassaemia intermedia o Clinical manifestations are more variable o Anaemia is moderate o Blood transfusion sometimes required -thalassaemia minor o Asymptomatic o onfused with mild IDA and lead to unnecessary Fe therapy -thalassaemia o More common in Asians o 4 gene del: fetal hydrops and death in utero. o 3 gene del: moderate chronic haemolysis. o 1-2 gene del: no clinical Sx Leukaemia Presentation: o Malaise o Abnormal bruising o Bone pain o Infections o Hepatosplenomegaly o Pallor o Lymphadenopathy Ix: low Hb. leukaemic blast cells on film. BM aspirate needed for diagnosis. CSF Treatment o Remission induction: correct any aneamia, infection, then 4/52 combo chemo o Intensification: blocks of intensive rx given to maintain remission o CNS Rx: by intrathecal chemo, cranial irradiation, high dose methotrexate o Continuing therapy: modest intensity for long time 3 yrs. o Treatment for relapse: high dose chemo with total body irradiation, BM transplant. DERMATOLOGY Eczema Atopic (commonest), allergic (type VI hypersensitivity) or caused by irritants or venous stasis. Diagnosis: clinically + IgE + specific allergens identified with skin prick and (RAST). Clinically: o Itch o Dry skin, o Classic distribution, o Lichenification Management: o Avoid irritants o Antihistamines: H1 histamine antagonists o Emollients o Dietary elimination o Topical corticosteroids o Psychosocial support: National Eczema o Occlusive bandages Society o ABs and antivirals Psoriasis Rare before the age of 2 Guttate type: o Most common in children o Follows strep/viral sore throat or ear infection o Lesions small, rain-drop shaped, round/oval scaly patches on trunk and upper limbs o Resolves in 3-4/12 o Rx: bland ointments. Coal tar preparations. Dithranol for chronic plaques Pityruasis Rosea: o Acute benign, self-limiting of viral origin o single round scaly macule (2-5cm) in a few days numbers of smaller dull pink macules on trunk, upper arms and thighsrash spreads in line with ribs posteriorly ‘fir tree pattern’. o Sometimes itchy o No Rx required resolves in 4-6wks MUSCULOSKELETAL SYSTEM Variations of normal posture Bow legs (genu varum) o Bowing of the tibiae causing knee to be wide apart o Common in 0-3yrs, no need for Rx Knock-knees (genu valgum) o Feet are wide apart when knees held together. Seen in 2-7yrs, usually resolves. Flat feet (pes planus) o Toddlers learning to walk have flat feet, due to flat medial longitudinal arch + fat pad o Marked flat feet can be a presentation of a collagen disorder e.g. Ehlers-Danlos syn o Rx with exercises, arch support in shoes, surgery for symptomatic adolescent In-toeing o 3 main causes: Metatarsus varus: an adduction deformity of a highly mobile forefoot Medial tibial torsion: at lower leg when tibia is laterally rotated less than normal Persitent anteversion of the femoral neck: at the hip when femoral neck is twisted forward more than normal Out-toeing o Uncommon, but may occur in infants between 6-12 months o When bilateral it is due to lateral rotation of the hips and resolves spontaneously Toe walking o Common in 1-3yrs. If persisting: CP, tight Achilles tendons, Duchenne’s Muscular Dystrophy DDH (Developmental Dysplasia of the Hip) At risk babies: o Breech o Caesarean for breech o BW o Older mother Diagnosis: examine hips at day 1 and at 6 wks. o click test of Ortolani: o Barlow manoeuvre US: image of choice. Rx: o Positioning device in abduction (Craig splint) o Restraining device (Pavlik harness) o o o o +ve FHx Postmaturity Other malformations Oligohydramnios Club foot (talipes equinovarus) Positional talipes from intrauterine compression is common. Foot is normal size, deformity is mild and can be corrected to the neutral position with manipulation. Talipes equinovarus is a complex abnormality. 1. Inversion 2. Adduction of forefoot relative to hindfoot 3. Equinus (plantar flexion) o 2x more common in males o Rx: start in 1st wk with foot manipulation, strapping and splinting. If Rx not worked after 3 months operative reduction is carried out. Juvenile chronic arthritis Now called Juvenile idiopathic arthritis = a group of conditions where arthritis for > 6wks in kids under 16yrs. Systemic arthritis (‘Still’s disease’) Affects young children Sx: o Acute illness/malaise o Arthralgia/myalgia o High, spiking fever o Hepatosplenomegaly o Anorexia, wt loss o Hb, neutrophil + platelets + acute o Salmon pink rash when fever high phase reactants Some recover without getting chronic arthritis, others develop polyarthritis Polyarticular All ages. Girls > boys. Usually symmetrical involvement of wrists, hands, knees and ankles Polyarticular disease + rheumatoid factor = ‘juvenile rheumatoid arthritis’ Pauciarticular/oligoarthritis Usually in young children. Usually knees, sometimes ankles and wrists. risk of eye disease, especially girls with antinuclear Abs (ANA) ‘Extended oligoarthritis’ when further larger joints are involved after 6 months Enthesitis-related arthritis Affects older boys. Large lower limb joints affected and a ‘sausage finger’ May have HLA-B27 tissue type and FHx. Acute iritis common. Juvenile psoriatic arthritis Involes interphalangeal jts therefore ‘sausage fingers’ + skin lesions + nail pitting Hip diseases in childhood Transient synovitis (TS, irritable hip) o Most common cause of acute hip pain o Occurs at 2-12yrs. Follows viral in o FBC, blood cultures and x-ray usually normal. Joint effusion on US. No pain at rest o Rx: bed rest and skin traction. Usually better in few days. Perthes disease o Ischaemia of femoral epiphysisavascular necrosisrevascularisation + reossification. o Age 5-10yrs. o Male:female 5:1. Bilateral in 10-15% o Onset insidious, limp, hip pain o Ix: X-ray shows density in femoral heads. Bone scan and MRI o Rx: bed rest and traction. In more severe disease maintain hip in abd with plaster Slipped upper femoral epiphysis o Displacement of epiphysis of femoral head postero-inferiorly. Bilateral in 20% o Most common in 10-15yrs, during adolescent growth esp obese boys o Presentation: may be acute after minor trauma o Sx: limp, hip, groin pain (referred to knee), limited movements. o Ix: diagnosis by X-ray o Rx: surgical (pin fixation in situ) Osteomyelitis Infection in the metaphysis of long bone. Common sites distal femur + prox tibia. Causes: Staph aureus, strep, H. influenzae, TB Presentation: painful, immobile limb, fever, swelling, tenderness, red, warm over affected area Ix: blood culture +ve, WBCs and acute-phase reactants. Bone scan identifies site of infection. Rx: IV ABs for several weeks, then oral. Surgical drainage if not responding quickly to ABs. Limb rested in splint then mobilised.