Kay_2008_Postop Analgesia
advertisement

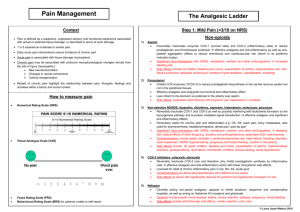
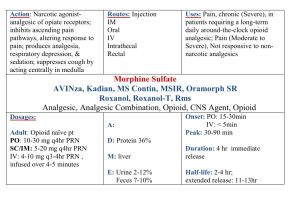
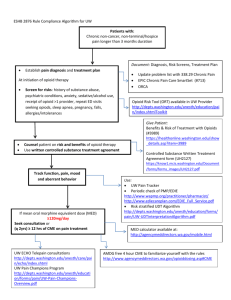
Principles of Surgery PERI-OPERATIVE ANALGESIA Joseph Kay, MD FRCPC Sunnybrook & Women’s College HSC Assistant Professor, University of Toronto Why should we treat peri-operative pain? pain and suffering complications likelihood of chronic pain patient satisfaction speed of recovery LOS cost productivity and quality of life Adverse effects of poor pain management Cardiovascular Respiratory Gastrointestinal\Genitourinary Neuroendocrine\Metabolic Musculoskeletal Immunological Psychological Current pain management Pain can virtually be eliminated with minimal side effects BUT 70% inpatients still have moderate or severe pain 40% outpatients have significant pain in 1st 24 h WARFIELD Anesthesiol 1995 83:1090 BEAUREGARD Can J Anesth 1998 45:304 Barriers to effective pain management I ANESTHESIOLOGIST Inadequate pain education Underestimation analgesic requirements Failure to recognize patient variability Inadequate use local\regional techniques Complications from side effects Barriers to effective pain management II PATIENT Expectation of severe pain Inadequate pain education Analgesic side effects Fear of addiction Barriers to effective pain management III NURSE Expectation of severe pain Inadequate pain education Fear of causing analgesic side effects e.g respiratory depression, addiction Insufficient time for assessment/ treatment Barriers to effective pain management IV SURGEON Belief that pain is ‘normal’ and not harmful Concern that pain may mask injury Inadequate pain education ‘Don’t ask don’t tell’ Complications from side effects\addiction Barriers to effective pain management V HOSPITAL Inadequate funding & resources with pain as low priority Inadequate commitment Lack of accountability Traditional opioid analgesia Parenteral prn Traditional opioid analgesia Sedation Respiratory depression Nausea & Vomiting Urinary retention Ileus Constipation Pruritus Multimodal Analgesia Using more than one drug, acting at a different place or with a different mechanism, each with a lower dose than if used alone, thus providing better analgesia with less side effects. Multimodal Analgesia Opioid NSAID (COXIB) Acetaminophen Local anesthetic block Other adjuncts Multimodal Analgesia Multimodal Analgesia Better analgesia Less side effects Can decrease hospital stay May improve surgical outcome May decrease chronic pain KEHLET Br J Surg 1999 86:227 CAPDEVILLA Anesthesiol 1999 91:8 REUBEN Anesthesiol 2001 95:390 Multimodal Analgesia Opioids Systemic - oral/parenteral/transdermal Neuraxial - spinal/epidural Peripheral - intra-articular, periosteal Multimodal Analgesia Opioids Sites of action Central: dorsal horn spinal cord Peripheral: synovium periosteum Multimodal Analgesia Opioids Systemic Oral contin + b/t Parenteral - iv PCA sc infusion + b/t Multimodal Analgesia Opioids Neuraxial Spinal - single shot Epidural - continuous infusion (+local anesthetic) Multimodal Analgesia Opioids Peripheral Intra-articular Iliac crest bone graft Opioid Intraoperative vs Postoperative THA 40 pts Intra-operative group: achieved VAS<3 42 vs 76 min morphine PACU 7 vs 15 mg respiratory depression PICO Can J Anesth 2000 47:309 Opioid Oral Controlled Release Oxycontin TKA 59 pts 29 oxycontin vs 30 placebo Oxycodone q4h prn Oxycontin group: pain LOS 2.3 days ROM CHEVILLE J Bone Jt Surg Am 2001 83A6:915 Opioid Iliac Crest Infiltration Spine fusion 60 pts Group I: saline into donor site Group II: 5 mg i.m morphine Group III: 5 mg morphine into donor site Opioid Iliac Crest Infiltration Gp III 50% less morphine 24h lower pain scores > 2h pain at 1 yr 5% vs 33% REUBEN Anesthesiol 2001 95:390 Multimodal Analgesia NSAID / COXIBS potent analgesics for mild-moderate pain adjunct to opioid for moderate-severe pain VAS 2/10 opioid consumption 30-50% opioid related side effects NSAID Spinal fusion Morphine PCA 70 pts ketorolac 0-30 mg iv q6h Ketorolac 7.5-30 mg: morphine use pain VAS sedation nausea REUBEN Anesth Analg 1998 87:98 NSAID side effects GI ulceration mild platelet dysfunction inhibition bone fusion mild Na+ retention / hypertension renal function in low flow states NSAID side effects CAN WE MAKE A BETTER NSAID? Keep analgesic potency Reduce side effects NSAID mechanism of action inhibits cyclo-oxygenases (COX-1&2) which convert arachidonic acid to prostaglandins (PG) PGE2 to sensitize nociceptors PGE2, PGI2, TXA2 for homeostasis COX 2 isoforms COX-1 constitutive – everywhere ‘housekeeping’ PGE2, PGI2, TXA2 COX-2 constitutive in kidney, CNS induced by trauma / pain main source PGE2 for sens. PGE2 production EP receptor BK receptor Tissue Injury Peripheral induction of COX-2 IL-1 Central induction of COX-2 PGE2 sensitization PGE2 EP receptor Bradykinin BK receptor Tissue Injury PGE2 Can we make a selective COX-2 inhibitor with excellent analgesia and less side effects than a conventional NSAID? YES COX-2 COX-1 NSAID NSAID Arachidonic acid Arachidonic acid COX-2 COX-1 PGE2 PGI2 TXA2 COX-2 Inhibitor Arachidonic acid Arachidonic acid COX-2 Inhibitor COX-2 inhibitors Celecoxib Rofecoxib Valdecoxib COXIB analgesic potency similar to or more potent than NSAIDs valdecoxib 40 mg = ketorolac 30 mg = 2 percocets! 24h duration DANIELS J Am Dent Assoc 2002 133:611 MEHLISCH J Oral Maxillofac Surg 2003 61:1030 COXIB pre-emptive effect rofecoxib 50 mg given 1 h pre-incision vs post pain opioid consumption prevents PGE2 sensitization from upregulated COX-2 REUBEN Anesth Analg 2002 94:55 COXIB side effects: GI incidence ulcers or bleeding compared to conventional NSAIDs BOMBARDIER NEJM 2000 343:1520 COXIB side effects: renal function COX-2 constitutive in kidney same effect as conventional NSAID mild Na+ retention, blood pressure renal blood flow in hypovolemia or CO Avoid in hypovolemia, CHF, renal dysfunction, uncontrolled BP ,DM BRATER J Pain Symptom Management 2002 23:S15 COXIB side effects: bone fusion conventional NSAIDs inhibit bone growth & fusion coxibs do not appear to clinically affect bone fusion rofecoxib/celecoxib vs control vs ketorolac in spinal fusion patients 9/132 vs 6/90 vs 23/120 GLASSMAN Spine 1998 23:834 REUBEN ASRA Annual mtg 2002 Abstract PD-16 LEWIS Proc NA Spine mtg 2000 64 COXIB side effects:allergy Can use in asthmatics May use rofecoxib with caution in ASA allergy Avoid celecoxib/valdecoxib with sulfa allergy GLASSER Pharmacotherapy 2003 23:551 STEVENSON J Allergy Clin Immun 2001 108 :47 COXIB side effects: platelet function NO effect on platelets NO effect on bleeding Patients on warfarin may have INR (need to adjust dose for cel/rof) LEESE Am J Emerg Med 2002 20:275 HOMONCIK Clin Exp Rheumatol 2003 21 :229 Summary COXIBS compared to NSAIDs more potent analgesic longer duration pre-emptive effect no effect on platelets less or no GI S/E no effect on bone fusion avoid opioid once a day use pre-op use pre-op use in risk use in ortho Multimodal Analgesia Acetaminophen Central COX 3 inhibitor opioid use by 30% opioid related side effects SHUG Anesth Analg 1998 Multimodal Analgesia Acetaminophen Avoid with: hepatic insufficiency alcoholism malnutrition P450 inducers Multimodal Analgesia Acetaminophen + NSAID usual adjunct for PCA opioid combination better than either alone VAS rest & dynamic FLETCHER Can J Anesth 1997 44:479 Multimodal Analgesia Local anesthetic Infiltration Intraperitoneal Nerve block Neuraxial Local anesthetic Movement assoc pain reduces function Local anesthetic blocks A & c fibres Incisional local infiltration Lap chole 157 pts periportal & intraperitoneal bupivacaine pre-incision or at end pain first three hours with pre-incisional periportal bupivacaine (+/- intraperitoneal) LEE Can J Anesth 2001 48:545 Peritoneal local infiltration Appendectomy Peritoneal infiltration 0.5% bupivacaine pain scores analgesic consumption COLBERT Can J Anesth 1998 45:734 Local infiltration Bupivacaine is BACTERICIDAL AYDIN Eur J Anesth 2001 18:687 Nerve Block Single shot ankle block interscalene 0.5% bupivacaine 6-24h postop analgesia Nerve Block Continuous Continuous Femoral Nerve Blk post total knee arthroplasty compared to PCA or epidural Nerve Block Continuous femoral Better analgesia Less morphine use Less opioid related side effects Better ambulation & hemodynamic stability CAPDEVILLA Anesthesiol 1999 91:8 SINGELYN Anesth Analg 1998 87:88 CHELLY J Arthroplasty 2001 16:436 Nerve Block Continuous femoral Better surgical outcome Less perioperative bleeding Increased flexion with CPM Earlier hospital discharge Less time in rehabilitation CAPDEVILLA Anesthesiol 1999 91:8 SINGELYN Anesth Analg 1998 87:88 CHELLY J Arthroplasty 2001 16:436 Nerve Block Single shot femoral 40 ml 0.25% bupivacaine vs saline post TKA pain VAS 1-2 50% morphine use 50% morphine related side effects Better ambulation LOS 3 vs 4 days WANG Reg Anesth Pain Med 2002 27:139 Nerve Block Continuous interscalene /popliteal Disposable pumps Major shoulder /leg surgery can be done as an outpatient $ Nerve Block Continuous popliteal nerve block at home 30 pts randomized to local anesthetic or saline Rescue oral opioids VRS 0 vs 4/10 Sleep disturbances 10x less O opioid pills vs 8 ILFIELD Anesthesiology 2002 97:208 Epidural Analgesia Epidural Analgesia LOCAL /OPIOID superior analgesia better cardiopulmonary function earlier return bowel function Epidural Analgesia LOCAL /OPIOID better ambulation decreased hospital stay safe to use on wards Epidural Analgesia Sigmoidectomy Early ambulation & feeding 2 day median hospital stay KEHLET Br J Surg 1999 86:227 Summary Pre-op Coxib Local infiltration / block Acetaminophen / Coxib post-op Controlled release opioid Thoracic epidural for major abdominal & thoracic surgery Continuous nerve blocks for extremity surgery