UNDERSTANDING DRUG ALLERGIES: An Oxymoron?
advertisement
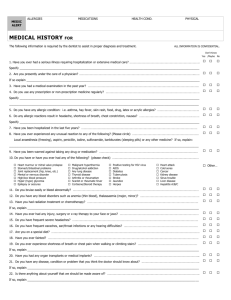
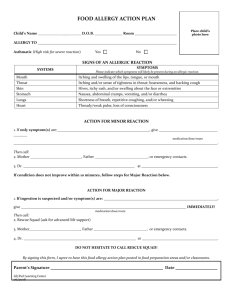
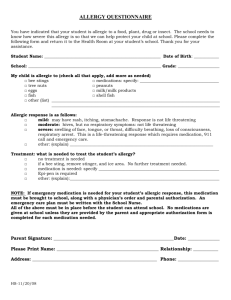
Allergic Reactions to Drugs and Diagnostic Agents Rebecca S. Gruchalla, M.D., Ph.D UT Southwestern Medical Center Dallas, Texas CASE HISTORY Mr. S is a 53 y/o WM who was admitted to the day surgery unit for a RUE contracture release procedure. His PMH is remarkable for a hx of swelling after taking penicillin several years ago. The patient did well during induction, but within minutes after receiving a “test” dose of cefazolin he developed urticaria and marked hypotension that required an epinephrine infusion. The pt’s BP stabilized and the pt recovered w/o sequelae. SCOPE OF THE PROBLEM WHO ADR Definition: “Any noxious, unintended, and undesired effect of a drug that occurs at doses used in humans for prevention, diagnosis or treatment” CLASSIFICATION OF ADRs Type A Reactions Predictable, common and related to the pharmacologic actions of the drug; may occur in any individual CLASSIFICATION OF ADRs Type A Reactions • Toxicity - hepatic failure with high-dose acetaminophen • Side effect - sedation with antihistamines • Secondary effect - development of diarrhea with antibiotic tx • Drug interaction - theophylline toxicity in the presence of erythromycin therapy CLASSIFICATION OF ADRs Type B Reactions Unpredictable, uncommon and usually not related to the pharmacologic actions of the drug; occur only in susceptible individuals CLASSIFICATION OF ADRs Type B Reactions • Intolerance - tinnitus with aspirin use • Idiosyncratic reaction - development of anemia with the use of oxidant drugs in the presence of G6PD deficiency • Hypersensitivity (immunologic) reaction anaphylaxis with penicillin administration • Pseudoallergic (nonimmunologic) reaction radiocontrast dye reaction FEATURES OF ALLERGIC DRUG REACTIONS • Immunologic drug reactions are preceded by a period of sensitization • First dose reactions imply that the patient either was previously sensitized to the drug or that the reaction was not allergic in nature FEATURES OF ALLERGIC DRUG REACTIONS • Allergic drug reactions are restricted to a limited number of syndromes that have a known or a presumed immunopathologic basis • Allergic drug reactions are temporally related to drug exposure FEATURES OF ALLERGIC DRUG REACTIONS • Immediate drug reactions may be triggered by a drug amount that is far below the therapeutic range! CLASSIFICATION OF ALLERGIC REACTIONS TO DRUGS • • • • Gell and Coombs Classification Immediate hypersensitivity reactions Cytotoxic antibody reactions Immune complex reactions Delayed-type hypersensitivity reactions CLASSIFICATION PROBLEMS • In some instances, classification is easy • In most instances, classification is difficult since the mechanism responsible for the reaction is not known • Hypersensitivity reactions are uncommon, unpredictable and can not be reproduced in animal models CLASSIFICATION PROBLEMS • Most drug-induced allergic reactions can not be classified into one of the Gell and Coombs classification categories because the mechanisms responsible are not known • We need to begin thinking “out of the box” • Both immune and nonimmune mechanisms may be operative EVALUATION OF THE DRUGALLERGIC PATIENT • History!! • History!! • History!! EVALUATION OF THE DRUGALLERGIC PATIENT • Identify all medication usage and dosages • Determine when a medication was initiated and establish a temporal relationship • Determine if there was a prior hx of drug exposure • Characterize the reaction type EVALUATION OF THE DRUGALLERGIC PATIENT • Determine if the patient has renal or hepatic disease • Determine the propensity a drug has for causing a particular type of reaction • Perform a thorough skin exam - urticaria?, petechia? mucous membrane involvement? • Distinguish between maculopapular eruptions and urticaria DIAGNOSTIC TESTS For Immunologically-Mediated Type B Rxns • General laboratory tests (LFTs, BUN/creatinine, CBC, urinalysis, CXR) • Biochemical/immunological markers that confirm the activation of certain pathways (total hemolytic complement, anti-nuclear antibodies, 24-hour urine for histamine metabolites) TRYPTASE • Selective marker of mast cells • Beta-tryptase is stored in secretory granules and it is actively released when mast cells degranulate • Beta-tryptase levels are elevated after anaphylaxis (>5 ng/ml) • Tryptase levels should be obtained 1-2 hours after the onset of anaphylaxis Tryptase Levels During Intraoperative Anaphylaxis Matsson et al. Agents and Actions 33:218, 1991 30 Units/liter 25 20 15 10 5 0 0.5 2 4 8 16 Time after reaction 32 64 DIAGNOSTIC EVALUATION Is Skin Testing Useful? DIAGNOSIS OF DRUG ALLERGY In Vivo Skin Testing • Large molecular weight compounds (foreign antisera, hormones, enzymes, toxoids) • Penicillin • Other antibiotics? PENICILLIN SKIN TESTING Predictive Value • Positive - Immediate reactions - 67% • Negative - Urticaria 98% - Anaphylaxis >99% Penicillin Resensitization in Patients with a History of Penicillin Allergy Solensky et al, Dallas, Texas, AAAAI 2000 • Up to 10% of the population reports an allergy to PCN • For immediate administration of PCN, the negative predictive value of the skin test is >99% • The predictive value for future courses was evaluated • All 29 patients who completed the study remained PCN skin test negative after 3 courses of PCN Penicillin-Allergic Patients Can They Receive Cephalosporins? • The degree of clinical cross-reactivity between penicillins and cephalosporins is unclear • In the literature, it is quoted that 10%-20% of patients with a history of PCN allergy and who are skin test positive to PCN will develop a reaction if given a cephalosporin • Current reaction rates are much less PENICILLINS AND CEPHALOSPORINS Share a Common Beta-lactam Ring Structure Cephalosporin Allergy General • Cephalosporins and penicillins have a common beta-lactam ring structure and moderate cross-reactivity has been shown in vitro. • Most of the cross-reactions have involved first and second generation cephalosporins. • Reactions to cephalosporins may be directed to the side chain. Cephalosporin Allergy Special problems • Carbapenems should be considered potentially cross-reactive with CS • Aztreonam (monobactam) and ceftazidime share a side chain and thus, may crossreact ADMINISTRATION OF CEPHALOSPORINS TO PATIENTS WITH A HISTORY OF PENICILLIN ALLERGY Bernstein et al. Ann Allergy Asthma Immunol 83:665, 1999 Option 1: Give the cephalosporin directly Although only 1% will have a reaction within 24 hours, their reactions may be anaphylactic!!! ADMINISTRATION OF CEPHALOSPORINS TO PATIENTS WITH A HISTORY OF PENICILLIN ALLERGY Bernstein et al. Ann Allergy Asthma Immunol 83:665, 1999 Negative Option 2: Skin test to penicillin Give cephalosporin; less than 1% will have mild reactions within 24 hrs Positive Options: 1. Give alternate drug 2. Give cephalosporin via graded challenge (2% will react with anaphylaxis) 3. Desensitize Acute Drug Desensitization • Definition – process by which a drug-allergic individual is converted from a highly sensitive state to a state in which the drug is tolerated • Procedure – cautious administration of incremental doses of the drug over hours to days – primarily used in IgE mediated reactions – may be employed in certain non-IgE mediated, immune reactions Drug Desensitization • IgE Sensitivity • Non-IgE Sensitivity – beta-lactam – trimethoprimantibiotics sulfamethoxazole – aminoglycosides – aspirin – clarithromycin – vancomycin – insulin – clindamycin – vaccines – anti-tubercular – quaternary agents ammonium muscle relaxants Candidates for PCN Desensitization • • • • History of IgE mediated reaction Positive PCN skin test No alternative antibiotics available Risk of fatal allergic reaction considered less of a threat than risk of fatal outcome if beta-lactam antibiotics not used Complications During Desensitization • Pruritus • Urticaria/angioedema • Wheezing Management Problems During Desensitization • Doses missed during therapy – omission – loss of IV access – expired orders • Drug suddenly D/C’d – misunderstandings on cross-coverage or new service • Drugs withheld due to new rashes • Full doses administered after long lapses in therapy Stark et al. J Allergy Clin Immunol 1987;79:523-32. Sulfonamide Hypersensitivity Reactions • Very frequent in HIV infected patients (44-70%) • Clinical Features – maculopapular rash – erythroderma – fever – leukopenia – urticaria/angioedema – erythema multiforme (minor or major) – toxic epidermal necrolysis Sulfonamides Hypersensitivity Reactions • Pathophysiology – urticaria/angioedema/anaphylaxis • likely IgE mediated –detected by skin test and RAST (poor sensitivity) – maculopapular/erythroderma rash • mechanism unclear –T cell mediated –IgG, IgM mediated –metabolic abnormality • drug metabolites TMP-SMX “Desensitization” ? • Overall there is a lack of evidence that the morbilliform eruptions and fever due to TMPSMX are due to IgE or non-IgE mediated mechanisms • Terms other than “desensitization” may be more appropriate – graded challenge – test dosing – tolerance induction – incremental dose regimen Vancomycin Adverse Reactions • • • • • • • • local phlebitis nephrotoxicity otic toxicity leukocytosis eosinophilia neutropenia agranulocytosis thrombocytopenia • Red Man syndrome • maculopapular eruption • urticaria • exfoliative dermatitis • fever Red Man Syndrome • Constellation of symptoms – common • pruritus • flushing – uncommon • hypotension • chest discomfort • Occurs in 35-90% of normal volunteers infused 1 gm vancomycin over 1 hr • severity correlates with amount of histamine released into plasma • severity reduced by – reducing rate to < 500 mg/hr – premedication with H1antagonists Vancomycin “Desensitization” • Wong et al. Evaluated the safety and efficacy of a rapid continuous IV “desensitization” in patients with adverse reactions to vancomycin – 7 patients had marked adverse reactions to vancomycin despite reducing rate and antihistamines • • • • • 100% intense pruritus 71% flushing 71% urticaria 29% hypotension 29% anxiety Wong et al. J Allergy Clin Immunol 1994;94189-94. Vancomycin “Desensitization” • Protocol – initial vancomycin infusion rate (VIR) 0.0001 mg/min – increased 3-3.3 fold q 10 min. – after VIR of 2.2-4.4 mg/min reached, infusion kept constant – if unable to be reached, last tolerated VIR used and dose increased over next few days Wong et al. J Allergy Clin Immunol 1994;94189-94. Vancomycin “Desensitization” • Results – 4/7 reached target VIR on 1st day – 3/7 reached a threshold VIR • reaction repeatedly occurred when VIR increased above threshold • symptoms rapidly abated when VIR lowered – above features argue against an IgE mediated mechanism • when narcotics discontinued, VIR able to be increased – Narcotics reduced threshold VIR in 5/7 patients Wong et al. J Allergy Clin Immunol 1994;94189-94. ACE-Inhibitor Induced Angioedema • • • • Can cause angioedema in 0.1-0.2% Predilection for face and upper airway Not drug specific Usually occur within first week of use, but may occur much later • May also occur with ARB’s • Pathophysiology not understood – Not an allergic mechanism SULFONAMIDE ALLERGY • Sulfonamide drugs are derivative of paraamino-benzoic acid • They have sulfur dioxide and nitrogen groups linked to the benzene ring • There is concern that sulfa allergic individuals may be sensitive to other drugs that contain these components (SO2NH2, benzene ring) • Some meds contain sulfur but are not sulfonamides Absence of Cross-Reactivity between Sulfonamide Antibiotics and Sulfonamide Nonantibiotics Strom et al. NEJM 2003;349:1628 • Of 969 patients with an allergic reaction after a sulfonamide antibiotic, 9.9% had an allergic reaction after receiving a sulfonamide nonantibiotic • Of 19,257 who had no allergic reaction after a sulfonamide antibiotic, 1.6% had an allergic reaction after receiving a sulfonamide nonantibiotic Absence of Cross-Reactivity between Sulfonamide Antibiotics and Sulfonamide Nonantibiotics Strom et al. NEJM 2003;349:1628 • However, the risk of an allergic reaction was even greater after the receipt of a penicillin among patients with a prior reaction to a sulfonamide antibiotic Absence of Cross-Reactivity between Sulfonamide Antibiotics and Sulfonamide Nonantibiotics Strom et al. NEJM 2003;349:1628 Conclusion • Thus, while there appears to be an association between sulfonamide antimicrobial allergy and reactions to sulfonamide nonantimicrobial drugs, this association “appears to be due to a predisposition to allergic reactions rather than to cross-reactivity with sulfonamidebased drugs” CELEBREX • Celebrex is a benzenesulfonamide derivative • Product labeling recommends that it not be given to sulfonamide-allergic patients • Cross-reactivity has not been reported but it is a theoretical concern • A retrospective meta analysis of premarketing trials compared the rate of allergic reactions to celcoxib, placebo, and other NSAIDs in pts with a history of sulfonamide allergy CELEBREX • Although sulfonamide allergy was an exclusion criterion in these studies, 135 out of 11,008 patients were found to be allergic to a sulfonamide antibiotic, furosemide, hydrochlorothiazide or a sulfonylurea • Among these patients, there was no significant difference in the rate of allergic reactions to celecoxib, other NSAIDs and placebo Algorithm For Disease Management Of Drug Hypersensitivity Patient develops a possible ADR Review of hx, records, PE and clinical tests support the occurrence of a drug reaction Algorithm For Disease Management Of Drug Hypersensitivity Immunologic reaction suspected? Yes No Non- immune ADR Management: • Modify dose • Alternative drug • Slow graded challenge • Prophylactic regimen • Patient education Algorithm For Disease Management Of Drug Hypersensitivity Not Available Perform confirmatory tests High negative predictive value? No Test positive? Yes Yes Patient not allergic to drug No Patient may be allergic Algorithm For Disease Management Of Drug Hypersensitivity Test Positive? Yes Patient may be allergic Diagnosis of drug hypersensitivity reaction confirmed MANAGEMENT Algorithm For Disease Management Of Drug Hypersensitivity MANAGEMENT: • Anaphylactic reactions require prompt treatment • Avoid drug if possible • Consider desensitization or graded challenge • Consider prophylactic regimen • Future prudent use of drugs • Future use of TEN/SJS-inducing drug contraindicated • Patient education References • Bernstein, I.L., Gruchalla, R.S., Lee, R.E., Nicklas, R.A., Dykewicz, M.S. Disease Management of drug hypersensitivity: A practice parameter. Ann Allergy Asthma Immunol 83:665-700, 1999. • Gruchalla, R.S. Allergic reactions to drugs. In Frank, M, Austen, KF, Atkinson, J, Cantor, H (eds): Samter’s Immunologic Diseases. Lippincott Williams & Wilkins. 72:921-934, 2001. • Gruchalla, R.S. Drug metabolism, danger signals and drug hypersensitivity. J Allergy Clin Immunol 108:475478, 2001.