Del Regato Gold Medal 2002
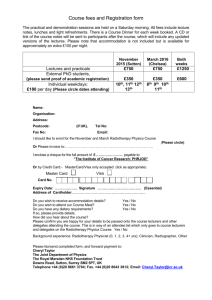
advertisement

Del Regato Gold Medal 2002, Baltimore, May 6 2002 Radiation Therapy, a young centenarian: a diagnosis based upon research achievements Jean-Claude Horiot, M.D., Ph. D.; Centre de Lutte contre le Cancer de Dijon, Université de Bourgogne, Dijon, France. Too much to say… May be I should have selected a simpler topic…. • Juan A. del Regato. • Other credits. • Lessons from (half) a century. –From infancy to maturity –Missed opportunities • A few guesses for the near future Juan A. del Regato. • Forty-four dollars and 50 cents…. • The French connection • The Cuban connection • The ICR 89 farewell… Forty-four dollars and 50 cents…. • A good investment… • Cancer, Diagnosis, Treatment and Prognosis. Lauren V Ackerman and Juan A. del Regato, • 1947, 1954, 1962, 1970 editions. • One of my four best friends for many years with: – Therapeutic radiology, Moss and Brand – Textbook of Radiotherapy, G.H. Fletcher – The Physics of Radiology, Johns & Cunningham • A model I had in mind for the second edition of the Oxford textbook of Oncology. The French connection • The Del Regato heritage at the « Fondation Curie »: • Part of a glorious lineage: Coutard, Regaud, Baclesse, Fletcher, Ennuyer, Bataini and so many pupils all over the world. • A deep bilateral sympathy which seems transmitted to Juan del Regato’s US-trained radiation oncologists and Foundation: – At least 5/26 of the previous del Regato’s medallists were either French or had an educational French touch… – G.H. Fletcher, M. Tubiana, F. Eschwège, A. Dutreix and myself. The Cuban connection • His name was Augusto Guttierrez • St Joseph Hospital, Houston Texas. • 1970, 1971, 1972 • With Gilbert Fletcher, Vera Peters, Luis Delclos and many Spanish speaking friends… The ICR 89 farewell… Other Credits. • Jean Papillon, • Gilbert Fletcher and his team, • Emmanuel van der Schueren, • Members of the EORTC group…. Jean Papillon 1914-1993 He was responsible of my RT vocation (1962) the President of my MD thesis (1965) the Director of my french RT training (65-69) an intuitive clinician and researcher capable even beyond retirement of transmitting his enthusisasm for what he believed in his achievements in rectal cancers (among many others..) Gilbert H. Fletcher 1911-1992 We met in 1965 in Paris, I had my US training with him from 1969 to 1972, could have worked with him much longer... a genius for synthesis, RT of subclinical disease Multidisciplinary approach for strategies Physics, Biology and Radiation therapy Emmanuel van der Schueren 1942-1999 •One of the most effective builders of European Oncology during the last three decades of the XX century. •The companion of so many research, education and organisational ventures. •My lost best friend. Lessons from (half a) century. From childhood to maturity • • • • Fractionation trials (H&N ca, RT alone) Breast cancer (optimisation RT/Surgery) Radio-chemotherapy (H&N, Anus) RT + hormonal treatment: Prostatic Ca Altered fractionation schemes. 20 years of efforts and a beautiful example of translational research before the definition was invented. • Hyperfractionation – 22791 • Accelerated radiotherapy – 22851 • Outside the RT group: – Dahanca 7 – German radiotherapy research group – a meta-analysis to come soon EORTC trials of hyperfractionated and/or accelerated radiotherapy From 1978 to March 1998: • 2398 patients accrued in phase II and III trials on: – Head and neck cancers – Malignant Gliomas – Lung – Bladder, Cervix, Endometrium Conventional vs. Hyperfractionated RT in oropharyngeal carcinoma T2 T3 (excluding base of tongue) N0 or N1 (less than 3 cm) random 70 Gy 35 fr 7 wks 80.5 Gy 70 fr 7wks EORTC 22791, 366 patients entered. Updated analysis, April 1998 April 98 Time to local failure 100 90 80 70 60 50 40 30 20 10 EORTC 22791 Logrank P = 0.02 (years) 0 O 2 N 4 6 8 10 12 14 16 18 Number of patients at risk : 79 159 58 33 23 14 7 2 1 0 CF 63 166 80 50 29 19 16 8 1 0 HF February 98 Fibrosis free (grade 3/4) 100 90 80 70 60 50 40 30 20 10 EORTC 22791 Logrank P = 0.90 (years) 0 2 4 6 8 10 12 14 16 O N Number of patients at risk : 4 118 51 20 10 6 5 1 0 CF 6 135 67 33 18 11 11 5 0 HF April 98 Overall survival 100 90 80 70 60 50 40 30 20 10 EORTC 22791 0 O (years) Logrank P = 0.05 N 2 4 6 8 10 12 14 16 18 1 1 0 CF 0 HF Number of patients at risk : 118 159 75 49 28 17 9 4 113 166 93 59 36 22 19 8 Conventional vs. Accelerated RT in Head & Neck carcinoma Advanced (T3/T4 any N, N2/N3 any T, excluding hypopharynx) Amenable to curative RT alone random 70 Gy 35 fr 7 wks 72 Gy 45 fr 5wks EORTC 22851, 511 patients entered 1986-1995. Analysis, August 1995 EORTC 22851 Accelerated RT regimen: 72 GY in 5 wks . • • • • 3 x 1.6 Gy per day, (4hrs interfractions) Ist course: 28.8 Gy in 7 days Stop 2wks 2nd course: 43.2 in 12 days EORTC 22851, Loco-regional control P = 0.019 (logrank test) 1 Conv. RTX Acc. RTX 0.8 0.6 0.4 0.2 0 0 2 4 6 years 8 10 EORTC 22851, Specific Survival p=0.06 1 Conventional Accelerated 0,9 0,8 0,7 0,6 0,5 0,4 0,3 0,2 0,1 0 0 2 4 6 years 8 10 12 Time without severe late toxicity (EORTC 22851) 100 CF 90 80 70 60 50 AF 40 30 20 Logrank P < 0.001 10 (years) 0 1 2 3 4 5 6 7 8 O N Number of patients at risk : 17 182 104 63 44 51 197 111 61 41 9 29 16 13 8 4 CF 29 19 14 4 0 AF Time without severe connective tissue damage P < 0.001 (logrank test) 1 0,8 0,6 0,4 CF 0,2 AF 0 0 2 4 6 years 8 10 FRACTIONATION STUDIES IN HEAD & NECK CANCER Overview of randomized trials with accelerated fractionation in head and neck cancer (local tumor control and morbidity) Conven- AcceleAcute Late tional rated morbidity morbidity Trial Treatment No. pts DAHANCA 6&7 66 Gy/ 33fx/ 6.5 w k vs 66 Gy/ 33fx/ 5.5 w k 1485 65% 75%* same Polish trial 66 Gy/ 33fx/ 6.5 w k vs 66 Gy/ 33fx/ 5.5 w k 385 77% 85%* same RTOG 9003 Conc. boost 70 Gy/ 35fx/ 7 w k vs 72 Gy/ 42fx/ 6 w k 532 45% 54%* 100 40% 86%* 512 46% 59%* 268 34% 58%* ? 350 51% 54% 918 47% 48% 159 31% 32% no data no data CAIR EORTC 22851 GORTEC TROG 9101 CHART V-CHART 66 Gy/ 33fx/ 6.5 w k vs 66 Gy/ 33fx/ 4.5 w k 70 Gy/35 fx/7 w k vs 72 Gy/ 45 fx/ 5 w k 70 Gy/ 48 days vs 63 Gy/ 23 days 70 Gy/ 35fx/ 7 w k vs 59.4 Gy/ 33fx/ 24 days 66 Gy/ 33fx/ 6.5 w k vs 54 Gy/ 36fx/ 12days 70 Gy/ 35fx/ 7 w k vs 55 Gy/ 33fx/ 17days * significant improved control (p<0.05) Conclusions (1) • The radiobiological principles of hyperfractionation and accelerated fractionation are supported by the results of EORTC trials. • A 15-20% gain in loco-regional control is obtained. • Hyperfractionation with moderate acceleration is transferable to standard practice. • The loco-regional control gain now results in a significant improvement of the overall survival in oropharyngeal cancers T2 T3, N0, N1. • HF did not increase late normal tissue damage. Conclusions (2) • Pure acceleration should be used with caution. • Full dose, 3 fractions per day and 5 wks split-course do not allow full repair of sub-lethal damage. • Full dose, 2 fractions per day, a 5 to 6 wks RT single course allows the AF delivery in better conditions. • Acceleration during the last 2 weeks is also feasible and of benefit (MDAH and RTOG 9003). • Working on Saturday (6fr per week) is an alternative… • Acceleration with a decrease of the total dose is feasible (CHART). Benefit seems marginal (except for larynx cancers). • We have not yet good predictors of tumor response. Progress in that direction is needed to select the patients for AF regimes. Chemoradiation is More Effective than Dose Escalation in Locally Advanced H&N-Cancer 3-Years Results of a German Multicenter Randomized Trial V.Budach1, S. Dinges1, I. Lammert2, M.Stuschke3, H. Sack3, K.-D. Jahnke4, M. Baumann5, T. Herrmann5, W. Budach6, M. Bamberg6, G. Grabenbauer7, P. Wust8, W. Hinkelbein9, H. Frommhold10, J. Dunst11, M.-L. Sauter-Bihl12, K.-D. Wernecke13 ARO 95/6 trial, IJROBP 51, 3, Suppl 1, 183-184, 2001 1Strahlenklinik und 2HNO-Klinik, Charité-Campus-Mitte, Berlin; 3Strahlenklinik und HNO-Klinik, UK-Essen; Strahlenkliniken 5UK Dresden; 6UK Tübingen; 7UK Erlangen; 8Charité-Campus-Virchow, Berlin; 9UKBF-Berlin; 10UK Freiburg; 11UC-Halle; GH-Karlsruhe; 13Institut für Medizinische Biometrie, Berlin ARO 95 - 6 Study STRATA (Centers, tumor site, N-stage) Arm A WE 10 Gy/ 2 Gy WE 21,6 Gy/ 2 / 1.4 Gy WE 35,6 Gy/ 2x 1.4 Gy WE 49,6 Gy/ 2x 1.4 Gy WE 63,6 Gy/ 2x 1.4 Gy 77,6 Gy/ 2x 1.4 Gy Arm B WE WE WE WE WE xxxxx 10 Gy/ 2 Gy 20 Gy/ 2 Gy X 5-FU, 600mg/m2 c.i. MMC, 10mg/m2 30 Gy/ 2 Gy 44 Gy/ 2x 1.4 Gy 58 Gy/ 2x 1.4 Gy 70,6 Gy/ 2x 1.4 Gy V. Budach et al., DEGRO 2001 Arm Arm p =0 .0 0 7 (e a p rl = y 0 ) 1 Nu 9 1 0 5 m 1 2 1 b 9 3 e 2 r78 62 46 a t r i s k 19 1 4 3 8 8 8 69 63 43 35 S 2 u 5 m 52 o 6 f 3 69 74 77 ev e n t s 3 5 7 2 87 91 96 97 0 6 12 18 24 30 36 Mont h i .t.t.( 0 Overall Survival [OS] (i.t.t.) Last Update: 13.08/01 Arm A - RT: 36 mos. Cum. Surv. CI 30.6% 24.6 - 38.0% Median 15 mos. Log-Rank: p=0.043*; p=0.057**;p=0.029***; Breslow: p=0.029*; p=0.004**;p=0.012*** Arm B - CRT: 36 mos. Hazard Ratio *stratified per centres Cum. Surv. 36.9% CI 30.4 - 44.8% Median 23 mos. B vs. A: 0.80* (Cl: 0.62 - 1.00) **stratified per sites ***stratified per sites and centres Conclusion - II Courtesy of Prof. Volker Budach, March 2002. Last Update: 12/01 Conclusion Accelerated Chemo-RT with 70.6 Gy + MMC/5-FU is more effective than accelerated radiotherapy alone with 77.6 Gy for (univariate Log-Rank-test): • Loco-regional Tumor Control (p = 0.004) • Overall Survival (p = 0.043) • and Progression-free Survival (p = 0.040) Breast cancer: Conservative management • 1950: Radical mastectomy +/- RT • 1970: Simple mastectomy + RT • 1980: Tumorectomy + RT • 1980-2000: – Role of RT for in situ disease – Role of radiotherapy in more advanced T – Refinements: Quality of surgery & RT, Cosmesis, Boost? 10853 DCIS Trial design DCIS local excision randomisation no further treatment external irradiation 50Gy /25 fractions DCIS : Local recurrence 100 RT 90 80 70 No RT 60 50 40 30 EORTC 10853 20 Overall Logrank test: p<0.001 (HR=0.54) 10 0 0 O 99 56 N 503 507 2 4 6 Number of patients at risk : 451 341 203 477 373 206 8 97 101 10 41 39 12 11 8 (years) 14 TRT LE LE+RT Julien JP, Lancet 2000 Conclusions EORTC trial 10853 At a median follow-up of 6 years, LR rate: LE Overall 20% 15% LE+RT 11% RT allows a the 46% reduction of local recurrence risk (p < 0.001, HR=0.54) Similar reductions of DCIS and invasive recurrence with a 6 yr-follow-up, no survival difference. Courtesy of Harry Bartelink Boost versus no Boost trial. coordinators: H. Bartelink, J.C. Horiot, E. Van der Schueren, data manager: M. Pierart, statistician: L.Collette Invasive breast cancer 0-5 cm, post complete excision no boost External RT 50GY R 16 Gy boost Same with incomplete excision (microscopic) External RT 50 Gy + 10 Gy versus 26 Gy boost EORTC 10881-22881 EORTC BOOST TRIAL (BREAST CANCER) 5,569 patients(1989-1996) Germany 374 NL 2603 UK 146 Belgium 817 Switzerland 306 France 1185 Spain 21 Israel 102 Data Maturity (analysis July 2000) • 5569 patients entered – 5318 with complete resection (CR) • 2657 to ‘No boost’ and 2661 to ‘Boost’ – 251 with incomplete resection (IR) • Median follow-up 5.1 years – 54% of patients with CR followed 5 years or more – 9% of patients with CR followed 10 years or more • 479/5318 have died so far Breast recurrence free 100 90 80 At 5 years: 70 No boost: 93.2% (92.2 - 94.3) 60 Boost: 50 95.7% (94.8 - 96.6) 40 30 20 Overall Logrank test: p=0.0001, HR=0.96 99% CI: (0.76 - 1.21) 10 0 (years) 0 O N 2 4 6 8 10 12 Number of patients at risk : 182 2657 2464 1734 748 127 1 CR No Boost 109 2661 2501 1761 749 143 0 CR 15 Gy Local Failures No Boost Primary tumor bed Scar Skin outside scar In breast tissue outside boost area Outside irradiated volume, within glandular tissue Diffuse Unknown site Total 86 16 17 29 (47.3%) ( 8.8%) ( 9.3%) (15.9%) Boost 51 10 7 19 (46.8%) ( 9.2%) ( 6.4%) (17.4%) 3 ( 1.6%) 4 ( 3.7%) 28 (15.4%) 3 ( 1.6%) 182 15 (13.8%) 3 ( 2.7%) 109 Fibrosis in whole breast (worst grade) No Boost None Minor Moderate Severe Unknown 1288 (48.5%) 991 (37.3%) 236 ( 8.9%) 24 ( 0.9%) 118 ( 4.4%) Boost 1339 (50.3%) 908 (34.1%) 261 ( 9.8%) 32 ( 1.2%) 121 ( 4.5%) Time to Severe palpable fibrosis in whole breast 100 90 80 70 60 50 40 30 20 Overall Logrank test: p=0.2790 10 0 (years) 0 O N 2 4 6 8 10 12 Number of patients at risk : 24 2657 2502 1802 789 136 1 CR No Boost 32 2661 2506 1785 767 154 0 CR 15 Gy Time to severe palpable fibrosis (WB or boost) 100 90 80 70 60 50 40 30 20 Overall Logrank test: p=0.0001 10 0 (years) 0 O N 2 4 6 8 10 12 Number of patients at risk : 37 2657 2498 1795 785 136 1 CR No Boost 92 2661 2485 1752 749 151 0 CR 15 Gy EORTC 22881, Local failure by age 100 90 80 70 60 50 40 30 20 10 0 100 90 80 70 60 50 40 30 20 10 0 Age <= 40 p<0.01 years 0 1 2 3 4 5 6 7 8 + Age 51-60 p=0.07 No boost Boost years 0 1 2 3 4 5 6 7 8 + 100 90 80 70 60 50 40 30 20 10 0 100 90 80 70 60 50 40 30 20 10 0 Age 41-50 p=0.02 years 0 1 2 3 4 5 6 7 8 + Age >60 p>0.1 years 0 1 2 3 4 5 6 7 8 + Local control No adjuvant treatment 100 90 80 70 60 50 40 30 20 Overall Logrank test: p=0.0021 10 0 (years) 0 O N 2 4 6 8 10 12 Number of patients at risk : 138 1911 1783 1293 597 105 1 CR No Boost 90 1870 1772 1290 590 108 0 CR 15 Gy Local control Adjuvant treatment 100 90 80 70 60 50 40 30 20 Overall Logrank test: p=0.0008 10 0 (years) 0 2 4 6 8 10 O N Number of patients at risk : 44 746 681 441 151 22 CR No Boost 19 791 729 471 159 35 CR 15 Gy Conclusions • A 16 Gy boost results in a 41% reduction (P<0.001) of the risk of local failure. • Young patients have the largest benefit : The 5-year local failure rate drops from 19.5% to 10.2% • The risk reduction ranges from 54% in the younger patients to 32% in the older patients • For patients older than 50, a boost may not be necessary • This benefit is associated with a slight impairment of the cosmetic outcome. • Chemotherapy does not spare the need for the boost. 22881: unexpected outcomes. • Continuous quality assurance resulted in: – Harmonisation of dose prescription and reporting. – Improved treatment planning. – National recommendations for Surgery/RT techniques and boost indications upon first publication. 22881: unexpected outcomes. • the huge size and quality of the data base will allow: – An unmatched long-term evaluation of late effects and cosmesis. – The retrospective analysis of individual genomic abnormalities in specific groups (< 40 year-old, negative nodes and poor prognosis…) Radio-Chemotherapy • Demonstration made one or several decades ago in some cancer types (e.g. lymphoma, breast, paediatric oncology…) • Was much longer to show up in most solid tumors (Head and neck, cervix, lung, anus, oesophageal cancers) • Evidence still missing or questionable in other cancers EORTC 22931 A phase III randomized study on post-operative radio-chemotherapy in patients with locally advanced head and neck carcinoma Jacques Bernier, (Bellinzona, Switzerland) Study coordinator A phase III randomized trial on post-operative concomitant radio-chemotherapy in patients with locally advanced head and neck Ca (EORTC 22931) • Joint Protocol: Head & Neck, Radiotherapy Groups • Activation:February 1994 • Closure: • Accrual: October 2000 334 patients • Median follow-up: 34 months ( actuarial estimate ) Treatment scheme Primary surgery Randomise Post-op XRT 66 Gy / 33 f / 6.5 wks Post-op XRT 66 Gy / 33 f / 6.5 wks DDP 100 mg/m2 d 1, 22, 43 Primary endpoint: Disease free survival Secondary endpoints: Acute tolerance, local control, overall survival, late complications Loco-regional control 100 90 80 70 60 50 40 30 20 10 0 23 Mar 2001 15:28 Overall Logrank test: p=0.0014 0 O N 47 167 23 167 (years) 2 4 6 Number of patients at risk : 55 74 22 23 1 3 8 XRT XRT+DDP Overall survival 100 90 80 70 60 50 40 30 20 10 0 Overall Logrank test: p=0.0057 0 O N 69 167 46 167 (years) 2 4 6 Number of patients at risk : 61 77 22 24 1 3 8 XRT XRT+DDP EORTC study 22931: Conclusions • Patient selection: – high risk Head and Neck carcinoma – post-operative setting • Compared to RT alone, CT-RT yields significantly higher local control and disease-free/overall survival rates, with no undue objective acute toxicity. • At a median follow-up of 34 months, it is too early to draw conclusions regarding: – time to metastasis and second primary – incidence of late effects in normal tissues MACH-NC, Bourhis et al. 1998: data based meta-analysis of randomized trials with chemotherapy in HNSCC # absol. 5 yr-benef. adjuvant CT induction CT concurrent CT total P. 1 854 5 269 3 727 1% 2% 8% .74 .10 <.0001 10 850 4% <.0001 MACH-NC, Institut Gustave Roussy Pending issues: Prognostic factors • Biological predictors of tumor response – proliferation – resistance to drugs • H&N sub-sites and stages • Appropriate assessment of T response • Frail patients • Elderly patients Pending issues: optimal management and follow-up of H&N cancers •Surgery (mutilating, non-mutilating)? •RT alone (including HF, AF, conformal,BT). •Concomitant CT-XRT: always better? •Optimal strategy per tumor site & sub site? •New (chemotherapy?) agents? •Reliability of salvage surgery after HF/AF XRT or after concurrent CT-XRT? •Quality of life during and after Trt? •Cost-effectiveness? Radio-chemotherapy versus Radiotherapy in T3 T4 anal Ca (EORTC 22861), H. Bartelink, study coordinator Eligibility criteria T3-T4 N0 or any T, N1-N3 proven anal S.C.Carcinoma PS < 2 (WHO) - age < 75 years no prior cancer or treatment Randomization RT: Radiotherapy 45 Gy (1.8 Gy/day, 5 weeks) RT+CX: Same radiotherapy + 5FU 750 mg/m2, d.1-5+29-33 + MMC 15 mg/m2 iv, d.1 Patients 110 recruited - 103 eligible (RT: 52, RT+CX: 51) Radio-chemotherapy in locally advanced anal cancer (22861) RESULTS: Colostomy free survival (P = 0.002) 1 0,9 RT RT+CX 110 patients 0,8 0,7 0,6 0,5 0,4 0,3 0,2 0,1 0 0 1 2 3 4 years 5 6 7 8 JCO,1997 Radio-chemotherapy in locally advanced anal cancer (22861) Radiotherapy with concomitant chemotherapy allows: • Better local control • Improved colostomy free survival • no difference in overall survival • no difference in acute and late toxicity in a randomized comparison with radiotherapy alone JCO, Vol 15, No 5, 1997 New study: Anal Cancer EORTC 22011-40014. (T3T4 or N+ any T) Phase II-III A 36 Gy - 4 weeks 23.4 Gy - 2.5 weeks 5FU 200 mg/m²/d1-26 5FU 200 mg/m²/d1-17 MMC 10 mg/m²/d1 MMC 10 mg/m²/d1 Gap 2 weeks R B 36 Gy - 4 weeks 23.4 Gy - 2.5 weeks CDDP 25 mg/m²/w CDDP 25 mg/m²/w d1 - d8 - d15 - d22 d1 - d8 - d15 MMC 10 mg/m²/d1 MMC 10 mg/m²/d1 RT + hormonal treatment: Prostatic ca EORTC RT AND GU GROUPS (22863) (M. Bolla et al., N Engl J Med, 337 (5), 1997: 295-300) T1-T2 G3 or T3-T4 any G Prostatic Adeno Ca Pelvic RT alone (50 Gy/ 5 weeks +20 Gy boost / 2 weeks) R Same Pelvic RT + 3-year adjuvant LHRH (3.6 mg Zoladex s.c. monthly, starting Dl of RT) • 415 patients entered between 1987 and 1995 • Median duration of follow-up 45 months • Adjuvant hormonal treatment improves pelvic control & survival (P=0.001) EORTC RT & GU GROUPS 22863 LOCAL CONTROL 97% (93-100%) 100 RTX + LHRH 90 80 RTX alone 77% (68-86%) 70 60 50 40 30 P=0.001 20 10 (years) 0 1 O N Number of patients at risk : 3 50 208 207 180 190 2 127 142 3 82 111 4 55 82 5 31 54 6 19 38 7 10 18 8 6 7 9 1 0 10 Treatment RTX RTX+LHRH EORTC RT & GU GROUPS 22863 OVERALL SURVIVAL 100 79% (72-86%) 90 80 70 RTX + LHRH 60 50 62% (52-72%) 40 RTX alone 30 20 P=0.001 10 (years) 0 1 O N Number of patients at risk : 58 35 208 207 183 190 2 139 144 3 96 111 4 67 82 5 6 7 8 9 10 Treatment 39 55 23 39 10 19 6 7 1 0 RTX RTX+LHRH Radiotherapy and prostatic cancer coming soon …. • In high risk locally curable prostatic cancers • EORTC trial : positive margins in resected T3 prostatic Ca: Rt versus observation. Another pivotal trial on hormonal treatment: • 22961: 3yr vs. 0.5 yr hormonal trt in LA Prostatic Ca as of 9/01: 1110 registered/1100 required Lessons from (half a) century. Missed opportunities • Fractionation trials • Rectal cancers • Developing countries A critical look at the practices Has Hyperfractionation become a standard? Yes, however seldom implemented …. A critical look at the practices (hyperfractionation and accelerated radiotherapy) Is there an active on-going research? • Not really… • Other priorities in laboratory and clinical research…. • Not much demand from the radiotherapy community…... Why did hyperfractionation (either pure or with AF), fail to be implemented? • Most RT departments cannot treat twice a day –shortage of equipment and staff –problems of transportation and/or day hospital admission –problems of expense refunding (health care insurance coverage for a single fraction/day) Why did hyperfractionation fail to be implemented? • Some oncologists said they were waiting for duplication of results…. • but did not change their behaviour when consistent results were published. Why did hyperfractionation failed to become implemented? • The major reason however is the challenge of medical oncology trials and the widespread prescription of miscellaneous (often) unproven chemo-radiotherapy regimes • The huge disproportion between the lack of support of a small group of RT equipment manufacturers and the powerful lobby of pharmaceutical industries. We did not loose our time… • The combination of radiobiology and clinical experience led to significant progress in our understanding of normal tissues and tumor radiation response. • Poor curative radiotherapy is almost eradicated: – large fraction size – insufficient or too long overall treatment time – inadequate target volumes – absence of quality assurance Lessons • Slowly responding normal tissues will express a lower late radiation damage when treated with hyperfractionation . • There is a steep dose response curve beyond 70 Gy • Optimised biological and high precision delivery of radiotherapy are achieved by combining: – Hyperfractionation, – Reduction of the overall treatment time, – Brachytherapy whenever applicable – Better treatment planning (conformal, IMRT) Missed opportunities Rectal cancers….. Three dogmas survived a long time (and are not yet dead.…) • Upfront surgery is the standard curative management of rectal cancers. • The Dukes (or modified Dukes) staging system only allows a realistic estimate of tumor extension. • Rectal cancers cannot be cured without surgery EORTC Pre-op trial 40761 • Surgery vs. pre-operative RT. 1976-1981. 466 pts. • T2 T3 T4 Nx M0 • 34,5 Gy/15 fr/18 d, L3, AP/PA. 5 yr local relapse: Surgery alone Pre-op 15% p=0.003 Surgery alone 30%30% vs. vs. Pre-op 15% p=0.003 • Conservative surgery: 77 % vs. 86 % • Survival benefit in favour of Pre-op in pts with curative resection (69% vs. 59%). Gérard A et al: Ann Surg 208: 606-614, 1984 Pre-operative RT in rectal cancers or a missed opportunity to be at least 10 years ahead of time… • Next step was to…investigate post-operative radiotherapy rather than to try to improve pre-operative radiotherapy techniques… • Reasons behind were mainly driven by the reluctance of surgeons to give up surgery first and rely upon clinical staging. • It will take another 13 years before confirmation by Swedish trials of the full benefit (pelvis control + survival) of preoperative RT... The Swedish rectal cancer trial Improved survival with pre-operative radiotherapy in resectable rectal cancer * • The New England Journal of Medicine: (1997; 336:980-7.) April 3, 1997. * Dr Lars Pâhlman & al. The Swedish rectal cancer trial • from March 1987 to Feb 1990 Patients' selection: • Resectable rectal adenocarcinoma (including T1). • Age < 80 • non metastatic Study design: Surgery alone versus pre-operative Radiotherapy (surgery 1week later) The Swedish rectal cancer trial Radiotherapy scheme: • 25 Gy in 5 fractions and 5 days • 4 fields box-technique • PTV: pelvis to L5 included. Accrual: • 1168 patients accrued from the six regional oncological centres of Sweden (in fact 70 hospitals) The Swedish rectal cancer trial Results • At 5 years: Local relapse rate: 27% Surgery alone vs. 11% Pre-operative RT p<0.001 The Swedish rectal cancer trial Results Overall 5 year survival rate: • Surgery alone: 48% • Pre operative Radiotherapy: 58 % ( p<0.004) 9 year cancer specific survival in resectable tumors: • Surgery alone: 65 % • Pre operative Radiotherapy: 74% ( p<0.002) The Swedish rectal cancer trial Results Local recurrence rate per stage and treatment Surgery alone versus pre-operative RT: • Dukes A (154/181): 12 % versus 4 % • Dukes B (173/195): 23 % versus 10 % • Dukes C (230/177): 40 % versus 20 % The Swedish rectal cancer trial Conclusions • Preoperative radiotherapy of resectable rectal cancers improves significantly: – Loco regional control (of at least 50%) – Overall survival – Disease free survival (of about 20%) • Preoperative radiotherapy is now the standard approach for clinically staged resectable T2 T3 T4 TME ± Pre-op XRT % Local Failures, Follow-up > 2 years XRT + TME TME alone Upsalla 2.6 9.3 Stockholm 1.4 10.7 Sweden + Norway (3/213) (18/168) 0-4 8 - 13 Confirmed in 2001 by the Dutch randomised trial. RT in rectal cancers Hopefully trial 22921 should be a landmark for improved strategies. Two major pending questions in T3T4 rectal cancers: • Is concomitant pre-op chemo-radiotherapy better than pre-operative radiotherapy? • Is there a need for post-operative chemotherapy in patients having received pre-operative radiotherapy? EORTC TRIAL 22921: a 4-arm multi-factorial design. Pre-op XRT 45 Gy in 5 wks + 5FU-LV + 5FU-LV SURGERY No further Trt Post-op + 5FU-LV Cooperative Group of Radiotherapy:J.F. BOSSET Study coordinator Post-op + 5FU-LV EORTC TRIAL 22921 • • • • • • Inclusion Criteria Rectal adeno Ca T3 T4 Nx M0 UICC 87 TR Ultrasound Clin. resectable WHO 0-1 Age < 75 • • • • • • • Stratification: Institution Sex Tumor location Stage Exclusion: Unfit for post-op. Trt Metastases Unresectable or incomplete surgery EORTC TRIAL 22921 Status as of April 8, 2002. • Entered: 932 • Required: 992 • Projected completion: early 2003 Lessons from (half a) century. Missed opportunities • Developing countries (what a poor name for!) – Cervix cancers: expertise and tools are present where disease is vanishing. – ISRO: A complex venture. – Needs, training, transfer of know-how. – Also a main political issue. • Their (our?) future lies in our ability to integrate their (research?) priorities with ours (e.g. HPV vaccines for cervix cancer prevention) A few guesses for the near future… A few guesses for the near future (1) • High precision radiotherapy • Resulted from a very successful cooperation between radiation oncologists, physicists diagnostic radiologists and industry. • Brachytherapy, conformal RT, IMRT are the best chance for the evolution of RT in a fast moving scientific environment The present … which CTV for the neck ? Cervical lymph node groups (MSKCC classification) Adopted by the Academy’s Committee for Head & Neck Surgery and Oncology Robbins et al, 1991 Which CTV for the neck? Oropharyngeal Carcinoma Stage Ipsilateral neck Contralateral neck N0-N1 II-III-IV + RP for post. pharyngeal wall tumor II-III-IV + RP for post. pharyngeal wall tumor N2a-N2b I1-II-III-IV-V +RP II-III-IV + RP for post. pharyngeal wall tumor N2c According to N stage on each side of the neck According to N stage on each side of the neck N3 I-II-III-IV-V +RP ± adjacent structures according to clinical judgment II-III-IV + RP for post. pharyngeal wall tumor 1Ib only for N2a Courtesy of V. Grégoire (Brussels) CT-based delineation of lymph node levels in the neck: Brussels-Rotterdam consensus guidelines Level Ia and Ib LIa LIb RP LII Ant. Post. symphysis menti / platysma hyoid bone / submandibular gland Lat. ant. belly of digastric m. (Ia) mandible / platysma (Ib) Med. ant. belly of digastric m. (Ib) Cra. geniohyoid m./mandible (Ia) mylohyoid m, submandibular gland (Ib) Cau. hyoid bone Courtesy of V. Grégoire (Brussels) CT-based delineation of lymph node levels in the neck: Brussels-Rotterdam consensus guidelines Level II LIb LII LV Ant. submandibular gland post. belly of digastric m. Post. sternocleidomastoid m. Lat. sternocleidomastoid m. Med. paraspinal m. int. carotid artery Cra. lateral process of C1 Cau. hyoid bone Courtesy of V. Grégoire (Brussels) CT-based delineation of lymph node levels in the neck: Brussels-Rotterdam consensus guidelines Level III LIII LV Ant. sternohyoid m./ sternocleidomastoid m. Post. sternocleidomastoid m. Lat. sternocleidomastoid m. Med. paraspinal m. int. carotid artery Cra. hyoid bone Cau. cricoid cartilage Courtesy of V. Grégoire (Brussels) CT-based delineation of lymph node levels in the neck: Brussels-Rotterdam consensus guidelines Level IV LVI LIV Ant. Post. Lat. Med. sternocleidomastoid m. sternocleidomastoid m. sternocleidomastoid m. paraspinal m. int. carotid artery Cra. cricoid cartilage Cau. 2 cm cranial to sternoclavicular joint Courtesy of V. Grégoire (Brussels) CT-based delineation of lymph node levels in the neck: Brussels-Rotterdam consensus guidelines Level V LVI LIII LV Ant. Post. Lat. Med. Cra. Cau. sternocleidomastoid m. trapezius m. platysma / skin paraspinal m. hyoid bone transverse cervical vessels Courtesy of V. Grégoire (Brussels) A few guesses for the near future (2) • Treatment individualisation will replace « standard strategies »: • 3D Imaging linked to high precision RT is one already • • • • effective example of that trend. molecular targets involved in radiation damage and repair, the understanding of the intimate mechanisms involved in normal to cancer cell biology, Molecular imaging, Should soon interfere with optimised cancer treatment planning. A few guesses for the near future (3) • Two main avenues: • Selection of choice of treatment will be influenced by the individual genomic pattern, • Novel therapies (e.g. Tyrosine Kinase inhibitors, Cyclin Dependent Kinases, Farnesyl Protein Transferase Inhibitors, anti angiogenesis factors) inactivate proliferation rather than destroy tumors, thus opening a new era for Surgery and Radiotherapy. Guesses for the near future (4) • An increasing gap between wealthy countries and the rest of the world… A last word of advice to younger oncologists • Remain first a clinician, • Never loose track of progress in a faster than ever changing world, • Translational research also applies to to radiation oncology. A truly last word… Thank you…