File - Ms. Sweeney's Science
advertisement

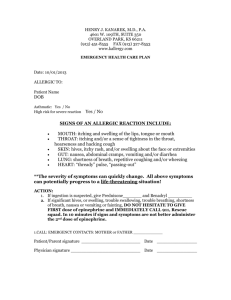
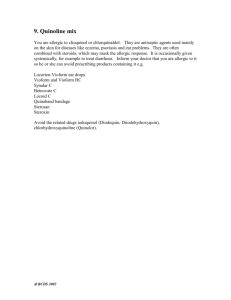
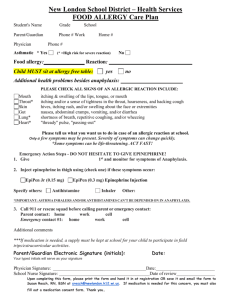
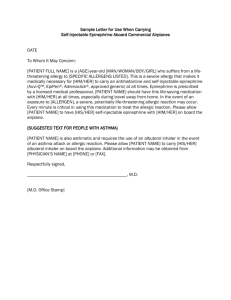
Chapter 18 Immunologic Emergencies National EMS Education Standard Competencies (1 of 2) Medicine Applies fundamental knowledge to provide basic emergency care and transportation based on assessment findings for an acutely ill patient. National EMS Education Standard Competencies (2 of 2) Immunology • Recognition and management of shock and difficulty breathing related to: – Anaphylactic reactions • Anatomy, physiology, pathophysiology, assessment, and management of: – Hypersensitivity disorders and/or emergencies – Anaphylactic reactions Introduction (1 of 2) • At least 1,000 Americans per year die of allergic reactions. • Allergy-related emergencies may involve: – Acute airway obstruction – Cardiovascular collapse Introduction (2 of 2) • You must be able to treat these lifethreatening complications. • Immunology is the study of the body’s immune system. Anatomy and Physiology • Immune system protects the body from foreign substances and organisms. • When a foreign substance invades the body: – Body goes on alert. – Body initiates a series of responses to inactivate the invader. Pathophysiology: Allergic Reaction (1 of 2) • An allergic reaction is an exaggerated immune response to any substance. • Not caused directly by an outside stimulus • Caused by the body’s immune system – Releases chemicals to combat stimulus – Include histamines and leukotrienes Pathophysiology: Allergic Reaction (2 of 2) • Caused by the body’s immune system – Releases chemicals to combat stimulus – Include histamines and leukotrienes • Allergic reaction may be mild and local, or severe and systemic. Pathophysiology: Anaphylaxis (1 of 3) • Anaphylaxis is an extreme, lifethreatening allergic reaction. – Involves multiple organ systems – Wheezing is one of the most common signs. Pathophysiology: Anaphylaxis (2 of 3) • Urticaria (hives) is also present. Source: © Chuck Stewart, MD – Consists of small areas of generalized itching or burning that appear as multiple, small, raised areas on the skin Pathophysiology: Anaphylaxis (3 of 3) • You may also note hypotension as a result of hypovolemic shock. Common Allergens (1 of 3) • Insect bites and stings – When an insect bites and injects the bite with its venom, this is called envenomation. – The reaction may be local (swelling and itchiness) or systemic (involving the entire body). Common Allergens (2 of 3) • Medications – Penicillin injection may cause an immediate and severe reaction. Source: Courtesy of Carol B. Guerrero – Oral penicillin may take longer. – A person will typically experience an allergic reaction after becoming sensitized. Common Allergens (3 of 3) • Plants – Dusts, pollens, other plant materials • Food – Reaction can be relatively slow – Shellfish, nuts • Chemicals – Makeup, soap, latex Insect Stings (1 of 11) • Death from stinging insects far outnumber deaths from snakebites. – Stinging organ of most insects is a small hollow spine projecting from the abdomen. – Venom can be injected directly into skin. Insect Stings (2 of 11) • Honeybees cannot withdraw their stinger. – Fly away and die • Wasps, hornets, and fire ants can sting multiple times. Source: A. © manfredxy/ShutterStock, Inc. Source: B. © Heintje Joseph T. Lee/ ShutterStock, Inc. Insect Stings (3 of 11) • Some ants, especially the fire ant, also strike repeatedly. – Often inject a particularly irritating toxin at the bite sites Source: A. Courtesy of Scott Bauer/USDA Source: B. © Chris Harvey/ShutterStock, Inc. Insect Stings (4 of 11) • Signs and symptoms include: – Sudden pain – Swelling – Localized heat – Redness in lightskinned individuals – Itching and possibly a wheal Source: © Simon Krzic/ShutterStock, Inc. Insect Stings (5 of 11) • There is no specific treatment for these injuries. – Applying ice sometimes helps. – Swelling may be dramatic and frightening. – Local manifestations are not serious. Insect Stings (6 of 11) • Stinger of the honeybee can continue to inject venom for up to 20 minutes. • Attempt to remove the stinger by scraping the skin with the edge of a sharp, stiff object such as a credit card. Insect Stings (7 of 11) • Do not use tweezers or forceps. • Wash the area with soap and water. • Remove any jewelry from the area. • Be alert for vomiting or signs of shock. • Give oxygen if needed. • Monitor the patient’s vital signs. Insect Stings (8 of 11) • About 5% of people may have anaphylactic reactions from: – Bees – Hornets – Yellow jackets – Wasps • Account for 200 deaths per year. Insect Stings (9 of 11) Insect Stings (10 of 11) • Patients may experience: – Generalized itching and burning – Widespread urticaria – Wheals – Swelling of the lips and tongue – Bronchospasm and wheezing – Chest tightness and coughing – Dyspnea Insect Stings (11 of 11) • Patients may experience (cont’d): – Anxiety – Abdominal cramps – Hypotension – Occasionally, respiratory failure • If untreated, anaphylactic reaction can proceed rapidly to death. Patient Assessment (1 of 3) • Scene size-up • Scene safety – Identify and address environmental hazards. – Patient’s environment or activity may indicate source of reaction. – Never enter a scene where more than one person is experiencing same symptoms. Patient Assessment (2 of 3) • Scene safety (cont’d) – Follow standard precautions, with a minimum of gloves and eye protection. – Consider the need for additional or specialized resources. – Call for additional resources earlier rather than later. Patient Assessment (3 of 3) • Mechanism of injury/nature of illness – May not be an allergic reaction – Trauma may have occurred. – Determine the MOI/NOI. – Look for bee stingers or chemicals and other indications of a reaction. Primary Assessment (1 of 5) • Perform a rapid scan of the patient. • Form a general impression. – May present as respiratory or cardiovascular distress in the form of shock – Patients will be very anxious. – Call for ALS backup if available. – Try to get information on the chief complaint. Primary Assessment (2 of 5) • Airway and breathing – Anaphylaxis can cause rapid swelling of the upper airway. – Only a few minutes to assess the airway and provide lifesaving measures – Work quickly to determine the severity of the symptoms. Primary Assessment (3 of 5) • Airway and breathing (cont’d) – Position conscious patients in tripod position and listen to the lungs. – Do not hesitate to initiate high-flow oxygen. – In severe situations, the definitive care is an injection of epinephrine. Primary Assessment (4 of 5) • Circulation – May present with hypotension – Palpate for radial pulse. • If the patient is unresponsive and without a pulse, begin BLS or use an AED. • If pulse is present, assess for a rapid pulse, and check skin condition and capillary refill. Primary Assessment (5 of 5) • Initial treatment – Oxygen – Positioning – Maintaining normal body temperature • Transport decision – Always provide prompt transport for any patient who may be having an allergic reaction. – Take along all medications and auto-injectors the patient has at the time. History Taking (1 of 4) • Identify: – Chief complaint – History of present illness – Associated signs and symptoms – Pertinent negatives History Taking (2 of 4) History Taking (3 of 4) • SAMPLE history • If the patient is conscious, ask the following questions: – Have any interventions already been completed? – Do you have any prescribed, preloaded medications for allergic reactions? History Taking (4 of 4) • Ask the following questions (cont’d): – Do you have any respiratory symptoms? – Do you have other symptoms? – Have you had previous allergic reactions, asthma, or hospitalizations? – What were you doing or what were you exposed to before the onset of symptoms? Secondary Assessment (1 of 4) • Physical examinations – Includes a systemic head-to-toe or focused assessment – Thoroughly assess breathing, including: • Increased work of breathing • Use of accessory muscles • Head bobbing, nostril flaring, grunting • Tripod positioning Secondary Assessment (2 of 4) • Physical examinations (cont’d) – Auscultate both the trachea and the chest. – Wheezing may occur because of narrowing of the air passages. – Assess the circulatory system. – Assess the skin for swelling, rash, hives, or signs of the source of the reaction. Secondary Assessment (3 of 4) • Vital signs – Assess baseline vitals: • Pulse • Respirations • • • • Blood pressure Skin Pupils Oxygen saturation Secondary Assessment (4 of 4) • Vital signs (cont’d) – Rapid respiratory rate indicates airway obstruction. – Rapid respiratory and pulse indicate respiratory distress or systemic shock. – Pulse oximetry is a useful method to assess the patient’s perfusion status. Reassessment (1 of 3) • Repeat the primary assessment and reassess the patient’s vital signs. – Deterioration of the patient’s condition could be rapid and fatal. – Give special attention to any signs of airway compromise. – Monitor the patient’s anxiety level. – Watch for signs of shock. Reassessment (2 of 3) • Interventions – Identify how much distress the patient is in. – Severe reactions require epinephrine and ventilatory support. – Milder reactions require supportive care such as oxygen. – Transport to a medical facility. – Recheck your interventions. Reassessment (3 of 3) • Communication and documentation – When to contact medical control depends on your assessment findings. – Documentation should include: • Signs and symptoms • Reasons for choosing to provide the care you did • Patient’s response to your treatment Emergency Medical Care (1 of 9) • If patient appears to be having a severe allergic (or anaphylactic) reaction: – Administer BLS, including oxygen. – Provide prompt transport to the hospital. – Reassess vital signs every 5 minutes (unstable patient) or 15 minutes (stable patient). Emergency Medical Care (2 of 9) – Place hypotensive or shock patients in the appropriate position. – Request ALS backup if you work in a tiered response system. – Be prepared to maintain the airway or administer cardiopulmonary resuscitation. Emergency Medical Care (3 of 9) – If a stinger is present, scrape away with a credit card. – Applying ice may help. – In some areas, you may be allowed to administer epinephrine or assist the patient with epinephrine administration. Emergency Medical Care (4 of 9) • Epinephrine – Mimics the sympathetic (fight-or-flight) response – Causes the blood vessels to constrict – Reverses vasodilation and hypotension – Increases cardiac contractility and relieves bronchospasm – Rapidly reverses the effects of anaphylaxis Emergency Medical Care (5 of 9) • Indications include: – A severe allergic reaction – Hypersensitivity to an exposed substance • Remember that your EMS service may or may not allow you to assist the patient in the administration of epinephrine. Call medical control! Emergency Medical Care (6 of 9) Source: Courtesy of Shionogi Pharma, Inc. • All kits should contain a prepared, autoinjectable syringe of epinephrine. Emergency Medical Care (7 of 9) • The adult EpiPen delivers 0.3 mg of epinephrine; the infant-child system delivers 0.15 mg. • The Twinject autoinjector contains two doses of epinephrine. • See Skill Drills 18-1 and 18-2. Emergency Medical Care (8 of 9) • Side effects include: – High blood pressure – Increased pulse rate – Anxiety – Cardiac arrhythmias – Pallor – Dizziness Emergency Medical Care (9 of 9) • Side effects include (cont’d): – Chest pain – Headache – Nausea – Vomiting Summary (1 of 7) • An allergic reaction is a response to chemicals the body releases to combat certain stimuli, called allergens. • Allergic reactions occur most often in response to five categories of stimuli: insect bites and stings, medications, food, plants, and chemicals. Summary (2 of 7) • The reactions may be mild and local, involving itching, redness, and tenderness, or they may be severe and systemic, including shock and respiratory failure. Summary (3 of 7) • Anaphylaxis is a life-threatening allergic reaction mounted by multiple organ systems, which must be treated with epinephrine. • Wheezing and skin wheals can be signs of anaphylaxis. Summary (4 of 7) • People allergic to bee, hornet, yellow jacket, or wasp venom often carry a kit that contains epinephrine in an auto-injector. • All patients with suspected anaphylaxis require oxygen. Summary (5 of 7) • Check patients who may be having an allergic reaction for flushing, itching, and swelling skin, hives, wheezing and stridor, persistent cough, decrease in blood pressure, weak pulse, dizziness, abdominal cramps, and headache. Summary (6 of 7) • Always provide prompt transport to the hospital for any patient who is having an allergic reaction. Remember that signs and symptoms can rapidly become more severe. • Carefully monitor the patient’s vital signs en route; be especially alert for airway compromise. Review 1. The signs and symptoms of an allergic reaction are caused by the release of: A. histamine. B. adrenalin. C. epinephrine. D. glucagon. Review Answer: A Response: The two chief chemicals released by the body that result in the signs and symptoms of an allergic reaction are histamines and leukotrienes. Epinephrine (adrenalin) is used to treat allergic reactions. Review 2. The negative effects associated with anaphylactic shock are the result of: A. severe internal fluid loss. B. inadequate pumping of the heart. C. vasodilation and bronchoconstriction. D. the nervous system’s release of adrenalin. Review Answer: C Rationale: Anaphylaxis is an extreme allergic reaction that is life threatening and involves multiple organ systems. In severe cases, anaphylaxis can rapidly result in death. One of the most common signs of anaphylaxis is wheezing, a high-pitched, whistling breath sound that is typically heard on expiration, usually resulting from bronchospasm/ bronchoconstriction and increased mucus production. Review 3. You are called to a local baseball park for a 23-year-old man with difficulty breathing. He states that he ate a package of peanuts approximately 30 minutes ago and denies any allergies or past medical history. Your assessment reveals widespread urticaria, tachycardia, and a BP of 90/60 mm Hg. You can hear him wheezing, even without a stethoscope. You should be MOST suspicious of a(n): A. acute asthma attack. B. mild allergic reaction. C. severe allergic reaction. D. moderate allergic reaction. Review Answer: C Rationale: The patient’s signs and symptoms indicate a severe allergic reaction, which is rapidly progressing to anaphylactic shock. Signs and symptoms of a severe allergic reaction include difficulty breathing, urticaria (hives) over large parts of the body, and signs of shock (eg, tachycardia, hypotension). Certain foods, such as shellfish and nuts, may result in a relatively slow onset of symptoms, but the symptoms can become just as severe. Review 4. What is a wheal? A. a raised, swollen, well-defined area on the skin B. a poison C. small areas of generalized itching or burning that appear as multiple, small, raised areas on the skin D. an exaggerated immune response to any substance Review Answer: A Rationale: Insect stings and bites can cause a wheal, which is a raised, swollen, welldefined area on the skin. There is no specific treatment for these injuries, although applying ice sometimes makes them less irritating. Review 5. You are treating a woman who was stung numerous times by hornets. On assessment, you note that some of the stingers are still imbedded in her skin. You should: A. leave the stingers in place. B. scrape the stingers from her skin. C. pull the stingers out with tweezers. D. cover the stings with tight dressings. Review Answer: B Rationale: Because of the venom left in the sac located at the end of the stinger, you should not grab the stingers in an attempt to remove them. Instead, scrape them off with a rigid object such as a credit card. Review 6. A young male is experiencing signs and symptoms of anaphylactic shock after being stung by a scorpion. His level of consciousness is diminished, his breathing is severely labored, you can hear inspiratory stridor, and his face is cyanotic. The patient has a prescribed epinephrine auto-injector. What should you do first? A. Assist him in administering his epinephrine. B. Apply high-flow oxygen via nonrebreathing mask. C. Provide ventilatory assistance with a bag-mask device. D. Elevate his legs and cover him with a warm blanket. Review Answer: C Rationale: The patient is not breathing adequately, as noted by his decreased level of consciousness, severely labored breathing, inspiratory stridor, and cyanosis. Therefore, you should first assist his ventilations with a bag-mask device. He clearly requires epinephrine, but not before restoring adequate breathing first. Regardless of the situation, a patient’s airway must be patent and his or her breathing must remain adequate at all times. Review 7. The MOST reliable indicator of upper airway swelling during a severe allergic reaction is: A. stridor. B. anxiety. C. cyanosis. D. wheezing. Review Answer: A Rationale: Stridor is a high-pitched sound that is most often heard during inhalation. It indicates swelling of the upper airway. Wheezing, a whistling sound, is caused by narrowed bronchioles; it indicates narrowing or swelling of the lower airway. Anxiety and cyanosis can occur from a variety of causes; they are not exclusive to airway swelling. Review 8. What is the best tool or method for assessing a patient’s perfusion status? A. small-volume nebulizer B. bag-mask device C. pulse oximetry D. auto-injector Review Answer: C Rationale: In a patient experiencing an allergic reaction, pulse oximetry is a useful method that you can use to assess the patient’s perfusion status. By using pulse oximetry, you can determine the percentage of oxygen saturation in the bloodstream, which will assist in identifying the degree of respiratory distress. Review 9. The adult EpiPen system delivers _____ mg of epinephrine, and the infant-child system delivers _____ mg. A. 0.15, 0.3 B. 0.3, 0.15 C. 0.15, 0.5 D. 0.5, 0.2 Review Answer: B Rationale: The adult EpiPen system delivers 0.3 mg of epinephrine via an automatic needle and syringe system; the infant-child system delivers 0.15 mg. Review 10. When administering epinephrine by autoinjector, the EMT should hold the injector in place for: A. 5 seconds. B. 10 seconds. C. 20 seconds. D. 30 seconds. Review Answer: B Rationale: When administering epinephrine via auto-injector, push the injector firmly against the thigh until it activates. Hold the injector in place for 10 seconds to ensure that all the medication is injected. Credits • Background slide images: © Jones & Bartlett Learning. Courtesy of MIEMSS.