'A' blood
advertisement

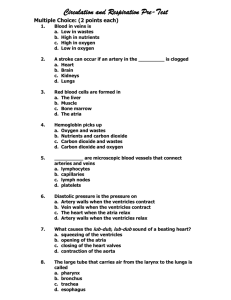
Cardiovascular System Circulation and Gas Exchange Circulation • Exchange of materials must take place across a wet membrane Simple animals have a gastrovascular cavity (digestion and circulation) Phylum Cnidaria: gastrovascular cavity Circulation • Complex organisms are multi-layered & have cells that are isolated and need transport systems • Special organs just for transport (circulation); heart, vessels Circulatory System Overview: • • • • Open vs closed Types of hearts in vertebrates Double circulation Structure and function of basic parts: – Heart, vessels, blood Open Circulatory System • No closed vascular tubes; ‘Blood’ (hemolymph) circulates freely in sinuses (spaces around organs) • Hydrostatic pressure returns the hemolymph to the heart – Ex. Arthropods, clams; limited in size Closed Circulatory System • Closed vessels; veins • Blood travels to an exchange surface (pulmonary), then to body cells (systemic) • Blood remains in vessels; – Much more efficient – Ex. Earthworms, vertebrates Closed Open Vertebrate Phylogeny Adaptations (Evolution) of the Cardiovascular System Structural Adaptations • Heart has chambers – Atria - Superior chambers - receive blood – Ventricles - Inferior chambers; pump blood away from the heart Vertebrate Hearts • Number of chambers is different, demonstrate evolutionary adaptation – 2 chambers = 1 atrium, 1 ventricle – 3 chambers = 2 atria, 1 ventricle – 4 chambers = 2 atria, 2 ventricles Blood passes through 2 capillary beds; pulmonary, (gill) systemic –Reduces blood pressure –Oxygen-rich blood slower to circulate Three Chambered Heart • Double circulation: blood travels separately to lungs and system • Oxygenated blood mixes with deoxygenated blood • Amphibians, reptiles Double circulation; pulmonary and systemic are separated Mammalian Heart 4-chambered, double circulation Systemic circuit Pulmonary circuit Systemic circuit 4 chambered: efficient, double circulation, homeothermic, lots of energy; ex. Mammals, birds Structure and Function of the Circulatory System • Three basic parts: – Heart – Blood vessels – Blood Heart • Cardiac muscle; Smooth (rhythmical, persistent) + striated (multinucleated, strength) • Muscle tissue can change shape, in response to electrical or chemical stimulation Heart Structure • Pericardium = sac that surrounds the heart (?) • 2 Atria; thin walled, receive blood, no pressure, right/left side – Right - receives systemic blood (‘deox’) – Left - receives blood from lungs (‘oxed’) Heart Structure • 2 Ventricles; thicker walls, pump blood to body/lungs, – Right - pumps blood to lungs (pulmonary) – Left - pumps blood to body (systemic); heaviest muscle Blood Flow Through the Heart 4. O2 rich blood to body 2. O2 poor blood to lungs 3. O2 rich blood from lungs 1. O2 poor systemic blood Cardiac Cycle • Heart cycle: sequence of events during heartbeat • Systole • Diastole Systole • Heart contraction • Chambers ‘pump’ blood • Atria contract first (0.1 seconds); atrial systole • Ventricles contract; force blood into arteries; ventricular systole Diastole • Relaxation phase – Ventricles refill with blood – Valves prevent ‘backflow’ Heart Cycle • Heart Rate = pulse; number of beats per minute – Avg. = 65-70/min. at rest • Stroke volume amount of blood that the left ventricle pumps systemically per minute; – Average human = 75 ml Cardiac Output • Rate x volume – vol. = 75ml – 70 ‘beats’ /min. – 75 ml x 70 = 5.25 l – 70/min. x 60 x 24 x 365 x 70 = • A lot Heart Cycle 25 1560 Inverse relationship between size and heart rate; Elephants = 25 Shrews = 1560 How Do We Keep Blood From Going ‘Backwards’? One-Way Valves Structure • Four valves: prevent ‘back flow’ • 2 Atrioventricular between atria and ventricles • 2 Semilunar; between ventricles and arteries, aorta and pulmonary Atrioventricular valves Left atrium Right atrium Tricuspid (‘three points’) Bicuspid (mitral valve) MVP Left Ventricle Right ventricle 2 Semilunar; between ventricles and arteries Aortic valve Pulmonary valve LV RV Heart Cycle • Heart sounds: valves opening/closing; “heart beat” • Stethoscope • “Lubb” = lower pitch, atrioventricular valves closing (bicuspid/tricuspid); ventricles contracting; just before systole • “Dupp” = semilunar valves closing; ventricles relax; just before diastole Heart Cycle • Heart Murmur: defect in valve causing backflow. Serious, corrected with surgery Normal Murmurs Control of the Heart Cycle Control of Heart Cycle • Intercalated disks = special areas between cells; extraordinary cell-to-cell communication; folds in between like tongue-in-groove – (Why is this important?) – structure/function Control of Heart Cycle • Cardiac muscle is myogenic (self-excitable) – Contracts without nervous input • Tempo is controlled by nodes (knots of nervous tissue + cardiac muscle) • Two ‘nodes’ stimulate muscle contraction – Sinoatrial Node (SA) – Atrioventricular node (AV) • Sinoatrial node (SA) - tempo of contraction “Pacemaker” • Starts a wave of contraction; causes both atria to contract together Atrioventricular node (AV) •Impulse delayed 0.1 second (why) •Impulse travels to Purkinje fibers; cause apex of heart to twist, wringing all blood out Electrocardiogram • Detects tiny electrical changes; action potentials • Depolarization/repolarization detected by electrodes on surface of skin • Length of time measurement indicates healthiness • Protracted time = unhealthy heart • Non-surgical procedure Regulation of Heart Cycle • Controlled by SA node • Influenced by: – Autonomic nervous system – Hormones – Temperature – Exercise • Balance controlled by medulla Regulation of Heart Cycle • Autonomic – ‘automatic’ – Causes release of norepinephrine (hormone) • Increases heart rate (emotions; fear, ‘love’) • Impulses come from cerebrum (memory) • Other causes for heart rate change: – Pressure – Ions –potassium, Ca. Blood Pressure • Systole = contraction of chambers; blood ‘pumped’ • Diastole = relaxing of chambers, ventricles, atria fill Blood Pressure • • • • Measured by a sphygmomanometer/stethoscope First number is systole Second is diastole 120/70 = ‘good’, normal Blood Pressure • The hydrostatic force that blood exerts against a vessel wall • Greater in arteries • Greatest during systole (contraction) • Peripheral resistance = impedance from arterioles; blood enters arteries faster than it can get out • Always pressure (even during diastole) Blood Pressure • What would cause blood pressure? • Cardiac output and peripheral resistance • Stress causes neural and hormonal responses which trigger smooth muscle to contract, increases peripheral resistance Blood Pressure • Pressure is near zero in veins – – – – Blood is returning to the heart Movement of muscle Valves in the veins Breathing increases volume in the thoracic cavity causing vena cavae to dilate Structural Differences in Vessels Arteries, veins, capillaries Vessels: 2 Types • Arteries; carry blood away from the heart • Branch out into arterioles • Branch into capillaries (diffusion/osmosis) Arteries • 3 layers (tunics): connective epithelium, smooth muscle and endothelium: thick walled; deep in body • Arteriole = smallest arteries with 3 tunics Veins • Veins; return blood to heart • Capillaries rejoin to form venules (microscopic) • Venules rejoin to form veins • May have flap like valves (back flow) • Thin walls; low pressure Blood Vessels • Capillary: endothelial tissue, thin, branched • Diffusion of O2 to individual cells Water that escapes from capillary diffuses back into lymph Capillary Exchange • Passive transport occurs by: – Diffusion – Osmosis – Hydrostatic pressure; blood pressure – Gap junctions = pores between cells Capillary Exchange • Capillary wall is ‘leaky’ • Materials may cross in vesicles – Active transport (endocytosis, exocytosis) Capillary Exchange • Gases move by diffusion • Fluids move by osmosis or vesicles • Direction of fluid flow depends upon the amount of pressure • Pressure = hydrostatic + osmotic Capillary Exchange • At the arteriole end: hydrostatic pressure outward is greater than the inward osmotic pressure • Fluids move OUT Hydrostatic pressure into the interstial fluid (materials move through in dissolved from) Capillary Exchange • At the venule end: outward hydrostatic pressure is less than the inward osmotic pressure • Fluids move back into the capillary Hydrostatic Osmosis pressure Hydrostatic pressure Osmosis Lymph System •Return Fluids to the Body •Immunity Lymph • 85% of fluids lost in capillary bed exchange is recovered at the venous end of the bed • Other 15% is recovered by Lymph • Lymphatic fluid = similar to interstial fluid (water, proteins, antigens) Lymph • Movement of skeletal muscle aids circulation of lymph (stay active) • Trauma or histamines may cause an increase in permeability • Lymphatic system cannot keep up • Surrounding tissues swell Lymph • • • • Lymph fluid travels through nodes ‘checked’ for antigens (invaders) Nodes may become swollen Also carries fats from digestion Heart Problems • Rheumatic heart disease = streptococcal infection; inflamed endocardium; valves damaged” MVP • Aneurysm = swelling in blood vessel • Embolism = moving clot Heart Problems • Coronary thrombosis = clot in coronary artery; causes infarction (area of damaged tissue) Heart Problems • Arrhythmia = heart out of rhythm: – Tachycardia = 100 + – Brachycardia = less than 60 – Flutter = 250+ – Fibrillation = heart muscles not contracting together; defribillator stops heart Heart Problems • Coronary heart disease = reduced flow to coronary arteries; ½ of all deaths in U.S. • Stress, hypertension (atherosclerosis) • Enlarges left ventricle (overwork) Heart Problems • Atherosclerosis = hardening of arterial wall due to build up of plaque (cholesterol); LDL = ‘bad’; HDL = ‘good’ • Arteriosclerosis = type of athersclerosis; addition of Ca deposits Arteriosclerosis Plaque Normal Arteriosclerosis Heart Problems • Myocardial infarction (‘heart attack’); angina pectoris = pain in chest, left arm, shoulder • Constriction of chest (angina); crushing, bursting (may fade/return) • Pain in back, jaw, left arm • Shortness of breath • Nausea, sweat, dizzy, pallor Heart Problems • Scar tissue replaces cardiac muscle • Rest, diet (animal fat) reduce stress • Exercise; dilation of skeletal muscles allows increased flow through systemic, increased O2 flow; brain works better… Heart Problems: Treatment • Digitalis = slows, strengthens heart contraction • Nitroglycerin = dilates vessels • Anticoagulants = prevent blood clotting Heart Problems • By-pass surgery; remove vessels (leg) and splice in around coronary vessel that is blocked (‘triple/quadruple by-pass’) • Stent = ‘balloon’ in artery to swell and break up thrombosis/clot Heart Problems • Congenital = from birth; septal defect, cyanosis (‘blue baby’) • Aging = heart failure: by 70, 30% decrease in heart efficiency; earlier if infections, toxins, anemia, hyperthyroidism, infarction, stress Heart Problems • Stroke = loss of blood supply; necrosis (tissue death); Infarction • Caused by: – Thrombosis (stationary clot) – Hemorrhage (blood leak) – Arteriosclerosis Blood • Connective tissue; 2 parts: – Plasma – fluid – 55% – Formed elements = solids; 45% • Makes up 8% of body mass • Average = 4 to 6 liters of whole blood Functions • Transport - O2, nutrients, enzymes, etc. remove CO2, wastes • Endothermy - (homeostasis) • Balance - fluid, electrolyte, pH (homeostasis) • Protection - from diseases, infection Plasma • • • • • Water = 90% Dissolved gases (CO2, O2 N2) Inorganic salts (electrolytes; salts) Proteins Other – urea, sugars, aa, hormones Plasma • Proteins = buffer blood, osmosis, viscosity (thickness) – Albumins = osmotic pressure – Globulins = immune (antibodies) – Fibrinogen = clotting agent • Serum = plasma with no clotting factors; Why serum? Blood: Formed Elements • Solids – Erythrocytes = 95 % – Leucocytes = varies – Platelets = 5 % Erythrocytes • ‘Red cells’ – Biconcave discs, transport oxygen – 25 trillion – Lack nuclei and mitochondria Hemoglobin Sickle cell • Iron-containing protein pigment; – 250 million molecules per RBC; 1/3 of mass – Reversibly binds with oxygen – Oxyhemoglobin -Bright red • Four heme groups; each contains an iron atom with an affinity for oxygen Sickle cell RBC Production • Hematopoeisis (‘blood make’) • Red marrow of long bones – Femur, humerus; skull, ribs, pelvis, sternum, vertebrae • 2.5 million/sec. • Nucleus lost during development RBC Production • RBC production stimulated by Erythropoeitin (hormone from kidney) • Negative feedback mechanism – Low oxygen = release of erythropoeitin • Exercise, altitude (low partial pressure) Blood: Physiology • After hemoglobin releases oxygen, it has a greater affinity for carbon dioxide – Carbaminohemoglobin – Reversible reaction • Hemoglobin has a greater affinity for carbon monoxide than oxygen or carbon dioxide Loss Prevention • • • • • Vasoconstriction Platelet plug Clotting (coagulation) Clotting factors inactive Become active when: – Connective tissue becomes exposed – Chemicals released from injured tissue • Positive feedback Clotting • Prothrombin (globulin protein) converted (by Ca) into thrombin • Thrombin converts fibrinogen into fibrin (sticky, thread like) • Fibrin forms a ‘mesh’ net • Platelets and RBC’s clog up = clot • Fragments of cells with membranes • Stick to collagen fibers (connective tissue), and each other to form platelet ‘plug’ Blood Agglutination An Example of Immune Response, Codominance, and Multiple Alleles Blood Agglutination • Clumping • Agglutinogens (antigens); – Glycoproteins on surface of RBC’s – ‘Flags’ • Agglutinins (antibodies) in plasma Blood Agglutination • Antibodies ‘attack’ antigens if they don’t match • Ex. – Anti A clumps B antigens – Anti B clumps A antigens • A person with “A” blood cannot receive “B” blood (?) • A person with “B” blood cannot receive “A” blood (?) ‘A’ antigens A ‘B’ Antibodies ‘B’ antigens B ‘A’ Antibodies Person with ‘A’ blood: given ‘B’ blood transfusion ‘B’ Antibodies ‘B’ antigens B B antibodies attach to B antigens; causes blood to agglutinate ‘A’ antigens Person with ‘B’ blood: given ‘A’ blood transfusion ‘A’ Antibodies A ‘A’ antigens are attacked by ‘A’ antibodies Person with AB blood: A, B antigens AB No antibodies What about “O”??? Person with O blood: No antigens O A and B antibodies Blood Typing • Type “AB” = ‘universal recipient’; has both antigens so neither antibody is present • Type “O” = ‘universal donor’; has no antigens so nobody’s antibodies are ‘awakened’ • Multi-allelic (more than 2 possible alleles can be inherited; A, B, or O (ABO blood groups) • Codominant = both A and B are expressed if present in the genes Genetic Blood Problems • Sickle-cell – globin molecule misshapen, recessive genetic; advantage for carriers (less malaria) • Hemophilia – lack of clotting factors; sexlinked recessive Other Blood Problems • Anemia = deficiency of erythrocytes or hemoglobin in the blood – Lack of energy; tired, listless, pale – Damage to marrow; inability to produce RBC’s; drugs – Pernicious anemia – lack of vitamin B12 (enables mitosis of RBC); lack of intrinsic factor, absorb B12 • Leukemia – cancer of leukocytes; immature (unable to function); overproduction of WBC prevents normal production of RBC’s/platelets; anemia, bleeding • Malaria – protozoa carried by mosquito (vector) • Septicemia – blood poisoning; surgery, decrease in blood pressure • AIDS – HIV; T-cell lymphocytes destroyed • Hepatitis – virus affecting liver; virus carried by blood after infection Blood Problems: Infections • Mononucleosis – lymphocytes are altered by virus, immune system attacks, swelling in lymph nodes White Blood Cells • Leukocytes = ‘white cell’; no hemoglobin – Function in the immune system – Amoeboid movement through tissues • Spend most time there (fighting) White Blood Cells • Arise from stem cells in bone marrow • Mature in spleen, thymus, lymph nodes, tonsils, adenoids • Normally 5-10,000 per mm3 5 Types of Leucocytes • Monocytes – leaves blood becomes macrophage (eats microbes, dead cells) • Neutrophils - most common; ‘pus’, eat antigen/antibody complexes • Basophils – least common; release histamine • Eosinophils – reduce inflammation, eat parasites • Lymphocytes – produce antibodies Gas Exchange Gas Exchange • Gas exchange = exchange of oxygen and carbon dioxide between the animal and the environment • CO2 + H2O H2CO3 H++ HCO3- Gas Exchange • Environment supplies oxygen and removes (recycles) carbon dioxide • Respiratory medium is air for terrestrials • Aquatics is water Gas Exchange • General knowledge: • Air = 21% O2 78% N2 • Water = 6-8 ppm O2; mg/liter; – Called Dissolved Oxygen – D.O. dependent upon: • Temperature of water • Solute concentrations in the water • Movement Slow moving, warm water = low D.O. Gas Exchange • Respiratory surface = where gas exchange takes place with environment – Must be moist – Diffusion • Thin, moist, epithelial tissue; highly vascularized • Single cell layer separates gases from blood Respiratory Organs • 4 types of respiratory surfaces: – Skin – Gills – Tracheae – Lungs Gills • Evaginations of the body surface • Skin is finely branched to form a feathery surface with large surface area • Often covered Gills • Have to be very efficient – Water has less oxygen than air • Ventilation = increase flow of the respiratory medium over the respiratory surface - brings fresh supply of O2 and removes CO2 • Water is dense; fish have to spend a lot of ATP to ventilate water • Surface is always moist Gills • Counter current exchange = blood flows in the OPPOSITE direction than the water passing over the gills • More efficient because there is a constant concentration gradient between blood and water Tracheae • Insects • Air has higher O2 content – Gases diffuse faster – Surfaces do not have to be ventilated as thoroughly • Dessicated (dry out) Tracheal System • Trachea = tiny air tubes that branch over the entire body • Spiracles= pores in the exoskeleton of animals for gas exchange • Air enters via spiracles and diffuses into the trachea into smaller branches which extend to every cell – Open circulatory system Tracheal System • Some ‘breathe’, ventilate (muscle contractions) • Others use diffusion Tracheal systems; may have ‘pouches’ near major organs Lungs • Invaginations of body surface • Thoracic cavity • Highly subdivided; many branches – Surface area • Two layers held together by surface tension of fluid between layers – Parietal pleura = thoracic wall – Visceral pleura = lung surface • Collapsed lung - broken surface tension Lungs • Air enters nostrils; filtered by hairs, warmed, humidified • Pharynx, larynx (voice box with vocal cords) • Cartilage lined trachea • Forks into 2 bronchi Lungs • Bronchi branch into bronchioles – Bronchitis • Bronchioles dead end into alveoli • Alveoli (air sacs) are lined with epithelium which is the respiratory surface Skin - Cutaneous • Amphibians, frogs, salamanders • Small, flat • Lots of surface area Lungs • Oxygen dissolves in the moist film covering the epithelium • Diffuses into the capillaries surrounding each alveolus • Carbon dioxide goes opposite Lungs • • • • Vertebrates ventilate by BREATHING Inhalation, exhalation Positive = frogs Negative = mammals Frog Ventilation • • • • • Enlarge mouth by lowering the floor of the mouth Close mouth and nostrils Push floor up Air forced into trachea Primitive lungs; mostly skin Fish Ventilation • Exchange surfaces in their mouth • Poor oxygen content of water • Air ‘gulpers’ – Betta, lungfish, electric eel Negative Ventilation Ventilating Lungs: Mammals • P = 1/V; inverse relationship • Increase volume, decrease pressure • Increase size of thoracic cavity decreases the pressure (less than the 760 mm atmospheric pressure) Ventilating Lungs: Mammals • Greater pressure on the outside causes air to ‘push in’ to the lungs (less pressure) • Diaphragm moves down, ribs expand outward (increased volume) Mammal Breathing • Parietal pleura attached to the ribs • Visceral pleura attached to the parietal pleura (surface tension from the fluid between) • As ribs expand, the lungs expand • Collapsed lung Mammal Breathing • Tidal volume = amount of air an organism inhales and exhales w/ each breath; 500 ml in humans • Residual volume = amount of air left in the lungs after exhalation • Vital capacity = maximum volume when forced (running); 4-5000 ml in college males Breathing: Birds • • • • Lungs; P. 892 8-9 air sacs in abdomen, neck, wings Reduces density (lighter) Heat sink for heat produced by flying (radiator) Birds • Parabronchi = small channels in the lungs where gas exchange takes place – More efficient; air moves in only one direction; no dead ends – Air is constantly pumped through – Maximizes complete air exchange (no residual volume) – Very efficient; altitude Control Centers in the Brain Regulate Rate and Depth of Breathing Breathing Controls • Automatic • Breathing center of the medulla sends impulses to the muscles (diaphragm, rib); 10-14 x min. • Negative feedback system Negative Feedback • Stretch the lungs; pressure sensors send messages back to medulla inhibiting inspiration Breathing Controls: Breathing Controls • Breathing center monitors blood pH; if CO2 levels increase, pH drops (acidic, acidosis) • CO2 + H2O H2CO3 • Stimulates increase in tempo Gas Exchange • Gas enters or leaves depends upon: Partial Pressure • O2 = 21 % of atmosphere • CO2 = 0.03 % • Partial pressure = proportion of pressure contributed by a gas in a mixture of gases • Air = gas mixture Partial Pressure • O2 = 21 % of 760 mm (atmospheric pressure) • Po2 = (760 x 21%) = 160 mm • Pco2 = (760 mm x 0.03%) = 0.23mm • Gases diffuse from ______to_____ Partial Pressure: p. 894 • In the alveoli, the PO2 is high and PCO2 is low • In systemic cells, PO2 is low and PCO2 is high • O2 diffuses into systemic from the blood; CO2 is opposite pO = 104 mm p CO2 = 40 mm pO =40mm; CO2=45mm pO=20; pCO2=45 pO=95; p CO2 = 40 Respiratory Pigments • Oxygen is carried by pigments because O2 does not diffuse easily into water • Arthropods (insects, crabs) have Hemocyanin; • Copper not iron Respiratory Pigments • Dissolved in plasma • Open circulatory • Hemoglobin; vertebrates Dissociation; p. 895 • Release of oxygen by hemoglobin is dependent upon: – Partial pressure – pH Dissociation • At rest, PO2 in tissues is low; • Hemoglobin releases only a portion of its O2 (28%) • If the partial pressure goes down (exercising) then hemoglobin releases more O2 Dissociation curve Bohr Shift • pH causes a change in hemoglobin affinity for oxygen • During exercise, increased CO2 is dissolved in the plasma • CO2 becomes carbonic acid (decreases pH) Bohr Shift • Conformation of hemoglobin is sensitive to pH change; loses affinity for O2 • BOHR SHIFT • Active muscle causes Bohr Shift, hemoglobin releases more O2 CO2 • Carbon dioxide carried by blood in 3 forms: – Bicarbonate ions in blood (70%) – Bound to amino groups (23%) – Dissolved in plasma (7%) CO2 • CO2 diffuses into erythrocytes • Carbonic anhydrase converts CO2 into bicarbonate • CO2 + H2O H2CO3 H+ + HCO3- Blood Chemistry • CO2 + H2O H2CO3 H+ + HCO3(bicarbonate) • Carbonic acid lowers pH; H+ is tied up by hemoglobin molecule to prevent drastic lowering of pH Special Adaptations • Seals, whales make lonnnggg underwater dives; deep • Myoglobin = oxygen storing pigment in muscles • More O2 in blood • Twice the blood per kg as humans Special Adaptations • Very large spleen – Contracts - releasing additional blood • Diving reflex slows heart rate – Oxygen consumption slows • Blood routed to brain, eyes, glands, placenta • Muscles shift to fermentation