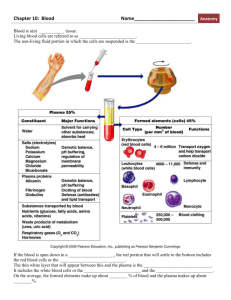
Formed Elements of Blood
advertisement

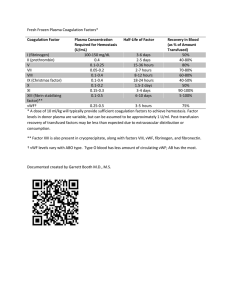
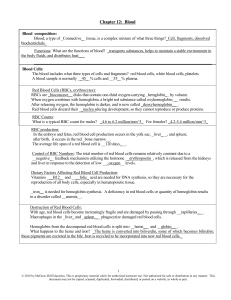
Formed Elements Formed Elements Includes all cellular parts of blood Composes approx. 45% of total blood volume Originate from stem cells Red Blood Cells A.K.A. erythrocytes Most abundant formed element – 95% of elements and 40% of total blood volume Small, flexible cells shaped like discs; thin in center, thicker on the edges—biconcave No nuclei or other organelles Shape provides more surface area; lack of organelles means more room for hemoglobin Hemoglobin RBCs continued Function is to bond to oxygen (O2) to carry it from lungs to body tissues a small amount of CO2 can also be carried by RBCs, but most of that is dissolved in plasma Short life cycle – last 120 days on average Any shortage in number of RBC’s or their capacity to carry O2 is referred to as anemia White Blood Cells Also known as leukocytes Represent less than 1% of total blood volume, increase or decrease in numbers indicate a diseased condition All contain a nucleus and can wander outside of the blood to fight infections in body tissues by either phagocytosis or secretion of antibodies See p. 351 for types of WBCs Platelets Also known as thrombocytes Fragments of complete cells Consist of cytoplasm wrapped with a membrane; contain most types of organelles Play a role in hemostasis Hemostasis Loss of blood can threaten homeostasis; hemostasis is the process by which the body prevents blood loss It is a process that involves three steps 1. Blood vessel spasm 2. Platelet plug formation 3. Coagulation Blood Vessel Spasm Walls of blood vessels contain smooth muscle tissue When vessel is broken these muscles contract, causing the ends of the vessel to “pinch in,” decreasing the size of the opening Sometimes this completely stops bleeding, sometimes not Spasm can last for up to 30 minutes Platelet Plug Formation Platelets passing through area of damage change in characteristics; increase in size, become irregular shapes, and become very sticky Sticky platelets adhere to rough edges of injury, usually collagen fibers This forms a plug which can stop the bleeding Coagulation Most effective and complex of clotting mechanisms Involves substances that are normally present in plasma (fibrinogen) and substances secreted by platelets at the site of injury Begins when platelets release thromboplastin, which interacts with Ca ions to convert prothrombin (present in small quantities in plasma) into thrombin Coagulation cont’d Thrombin works as an enzyme to link molecule of fibrinogen into fibrin Fibrin molecules very long, sticky, and insoluble in water They form a net that traps formed elements; this makes a blood clot Process takes 2 – 8 minutes, depending on size of injury to blood vessel Coagulation cont’d Once the clot is formed, repair of the injury can begin through the action of fibroblasts from neighboring connective tissues Blood clots sometimes form where they are not needed, especially if the blood vessel is not smooth Undesirable clot which is stationary can is called a thrombus, free-floating ones are called an embolus Both can block blood vessels and be dangerous Animation of Hemostasis Animation Blood Groups First discovered when blood transfusions became medically possible In blood types that are incompatible cells will clump together (agglutination) Blood grouping relies on proteins located on the surface of RBCs called antigens and their interaction with proteins found in plasma called antibodies Blood Groups cont’d Red Blood Cell Plasma Type A Antigen A Type B Antigen B Type AB Antigens A and B Antibody B (anti-B) Antibody A (anti-A) No antibodies Type O No antigens Anitibodies A and B (anti-A and anti-B) The Rh System First discovered in the rhesus monkey People with Rh antigens on cells are referred to as Rh positive, those lacking them are called Rh negative Unlike anti-A and anti-B, anti-Rh is not present from birth In order for the plasma to contain anti-Rh antibodies, the individual must first be sensitized through exposure to Rh positive blood