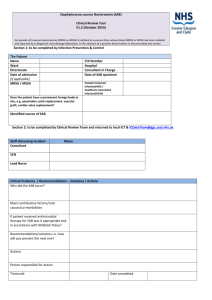
A multi-disciplinary approach to reducing haemodialysis catheter
advertisement

A multi-disciplinary approach to reducing haemodialysis catheter-related bloodstream infections Dr Karen Burns Consultant Clinical Microbiologist, Beaumont Hospital 4th Annual Transplant & Nephrology Conference November 27th 2015 Presentation Outline 1. Introduction 2. Why do we care about haemodialysis catheterrelated infection? 3. Where we were 4. What we’ve done 5. Conclusion Karen Burns November 2015 2 Introduction • Data presented on behalf of our multi-disciplinary team: – – – – – – Maeve Crudge & Maria Greene, Renal IPCNs Mairead Skally, Microbiology Surveillance Scientist Haemodialysis Nursing Team, led by Veronica Francis Nephrology Clinical & Nursing Team Clinical Microbiology Team Infection Prevention & Control Team • Beaumont Hospital Kidney Centre – 162 hospital haemodialysis patients: • Haemodialysis catheter: 60% • Fistula/graft: 40% – 45 PD patients – 25 home haemodialysis patients Nov 2015 data courtesy: C Collier & F Auguste Karen Burns November 2015 3 http://www.hse.ie/eng/about/Who/NRO/epidemiology.pdf Karen Burns November 2015 4 Resident Flora 10 times more bacteria live on and in a human, than the sum of that person’s own cells Bacteria found in and on the human body usually causing no harm – “normal flora” / “colonisers” Important to our survival Protect us from infection with C. difficile Karen Burns November 2015 5 Transient Flora – Social & healthcare hand hygiene WHO Guidelines for Hand Hygiene in Healthcare 2009 Karen Burns November 2015 6 Skin Barrier Healthcare increases a patient’s risk of developing infection Karen Burns November 2015 7 Introduction • Haemodialysis: – Temporary vascular access – Long-term vascular access Intravascular catheters are a risk factor for infection: •Exit site infection •Catheter tunnel infection •Catheter-related bloodstream infection (CRBSI)/bacteraemia Karen Burns November 2015 8 Karen Burns November 2015 9 What bugs cause haemodialysis catheterrelated infection? • Any microorganism can cause infection: bacteria, yeasts/candida • Important factors: – Bacteria: virulence, antimicrobial resistance – Opportunity/portal of entry: skin break, breach in sterile technique, biofilm, personal hygiene – Host/patient’s immune response: sepsis, critical illness, immunocompromise, prior antimicrobial exposure, skin breaks – Haemodialysis status: acutely unwell vs chronic stable – Haemodialysis access: temporary non-tunnelled vs long-term tunnelled Karen Burns November 2015 10 Biofilm Community of bacterial cells enclosed in a self-produced matrix (slime) adherent to a surface e.g; catheter tubing Surface Primary Attachment Accumulation Microcolony Formation 60% of HCAI involve biofilms 11 Karen Burns November 2015 BSI Diagnosis Karen Burns November 2015 12 Staphylococcus aureus STAPHYLE = “BUNCH OF GRAPES”, KOKKOS = “GRAIN/BERRY” • Gram-positive cocci in clusters • Coagulase positive • Normal flora/coloniser of nasal passages of up to 30% of general population – carriage may be intermittent or chronic • Skin carriage promoted in setting of skin breaks/conditions • Estimate 53 million people colonised with S. aureus in US • 26% of 2,374 patients undergoing haemodialysis nasal carriers of S. aureus Grothe C et al BMC Nephrology 2014;15:202 Karen Burns November 2015 13 On blood agar: Large beta haemolytic creamy-white colonies typical of S.aureus Karen Burns November 2015 14 S. aureus & infection • Skin/soft tissue – cellulitis, abscess, surgical site infections, device exit site infection • Bloodstream infection (BSI) • Deep-seated infection: endocarditis, discitis, osteomyelitis, epidural, psoas abscess etc. • Infection caused by S. aureus can result in sepsis, septic shock, death Karen Burns November 2015 15 BONE INFECTION INFECTIVE ENDOCARDITIS Large ulcerovegetative lesion on mitral valve. Culture grew S.aureus SKIN & SOFT TISSUE INFECTION T1 weighted MRI image reveals abnormal signal at intervertebral disc level L2-3 with associated vertebral osteomyelitis. CT-guided biopsy aspirate grew S.aureus Karen Burns November 2015 Large buttock carbuncle which developed over 7-10 days and required incision, drainage 16 and IV antibiotics. Pus grew S.aureus Staphylococcus aureus S. aureus • Antimicrobial resistance is an issue for S. aureus: – Meticillin susceptible S. aureus (MSSA) – Meticillin resistant S. aureus (MRSA) – Glycopeptide intermediate S. aureus (GISA) – Glycopeptide/vancomycin resistant S. aureus (GRSA/VRSA) Karen Burns November 2015 17 What do we know about S. aureus infection in Ireland? • We don’t know the total burden of S. aureus infection in Ireland • S. aureus bloodstream infection (SA BSI) reported by microbiology laboratories to HPSC on a quarterly basis: SA BSI in Ireland 2005 2014 Total cases 1,424 1,118 Total MRSA (%) 592 (41.6) 218 (19.5%) • 2015 HSE annual service plan: KPI for national rate of MRSA BSI in acute hospitals of <0.057/1000 bed days used (2014 national rate = 0.055) Karen Burns November 2015 18 What do we know about S. aureus infection in Ireland? • 21 labs provided additional information on SA BSI in 2014: Total MSSA BSI MRSA BSI 378 92 % Community-acquired 35% 23% % Haemodialysis 3% 8% • Since April 2014, mandatory monthly reporting of: new hospital-acquired SA BSI, by each acute hospital to HSE for monthly performance assurance report – data remains unpublished to date – doesn’t include burden of outpatient haemodialysis SA BSI http://www.hse.ie/eng/services/publications/corporate/performancereports/aug15pr.pdf Karen Burns November 2015 19 What do we know about S. aureus BSI in our hospital? SAU/MRSA no.s and Beaumont Hospital %: 120 vs. Tertiary %MRSA 30% SAU/MSSA no.s and rates: 120 25% 100 Beaumont Hospital 0.400 vs. Tertiary MSSA rate 0.350 100 15% 40 10% 0.250 %MRSA 60 80 %MRSA 20% Number of isolates 80 Number of isolates 0.300 60 0.200 0.150 40 0.100 20 5% 20 0 0% 0 2010 2011 2012 2013 2014 2015† 0.050 0.000 2010 2011 2012 Year MRSA no. MSSA no. 2013 2014 2015† Year %MRSA Tertiary %MRSA MRSA no. MSSA no. MSSA rate Tertiary MSSA rate 106 SA BSI in 2014, 21 MRSA BSI (19.8%) Karen Burns November 2015 20only Ϯ2015 data to end Q2 What do we know about S. aureus BSI in our haemodialysis patients? • All haemodialysis patients with SA BSI diagnosed in our microbiology laboratory: 1998 – 2009 • 304 patients with 394 episodes of SA BSI • 69% MSSA vs 31% MRSA • Majority of episodes due to intravascular catheter (83%) • 11% of episodes associated with infectious complication Karen Burns November 2015 21 Fitzgerald S et al. J Hosp Infect 2011 (79);218-221. What do we know about S. aureus BSI in our haemodialysis patients? • Clinical microbiology team reviews all inpatients with significant sterile site isolates • January 2007 – June 2012: Renal patients accounted for 20% of all positive blood cultures processed in our laboratory: – Coagulase-negative staphylococci – S. aureus Source S. aureus (n=171) – E. coli CVC 56.7% None 12.3% Unknown 8.2% Skin/Soft tissue 8.2% AV Fistula 2.3% Other 12.3% Source Urinary Tract IA/GI Tract UT Catheter None Unknown Other E coli (n=130) 55.4% 11.5% 10.8% 9.2% 7.7% 5.4% – Renal patients accounted for 30% of all S. aureus BSI Karen Burns November 2015 22 Why should we care about SA BSI in our haemodialysis patients? • Increasing prevalence of patients with ESKD in Ireland http://www.hse.ie/eng/about/Who/NRO/epidemiology.pdf Karen Burns November 2015 23 Why should we care about SA BSI in our haemodialysis patients? • Vascular catheter use for haemodialysis is high in Ireland • 2011 national survey: none of 19 Irish HD units met NKF-KDOQI targets of AVF prevalence >65% & CVC prevalence <10% McCann M. National survey of routine practice in Irish haemodialysis units 2011; Report Jan 2013 Karen Burns November 2015 24 Why should we care about SA BSI in our haemodialysis patients? • S. aureus BSI results in morbidity & mortality for our haemodialysis patients • S. aureus BSI results in requirement for hospitalisation, removal of permcath, temporary catheter placement and replacement of permcath, invasive investigation for infectious complications (e.g., TOE), minimum of 14 days intravenous antimicrobial therapy • Reduced future vascular access site options Karen Burns November 2015 25 Critical control points for infection prevention 1. Device insertion 2. Device maintenance 3. Device use 4. Surveillance of device-related infection: You can’t manage it if you’re not measuring it Karen Burns November 2015 26 National guidance 2005 2005 2009 Karen Burns November 2015 27 Do you know what’s going on in your haemodialysis unit? McCann M. National survey of routine practice in Irish haemodialysis units 2011; Report Jan 2013 Karen Burns November 2015 28 October 2012 – MDT convened • Screening for carriage of S. aureus: – – – – ? All S. aureus (MRSA & MSSA) ? Just MRSA Timing, frequency, logisitics of screening, lab workload What to do with the positive patient? Karen Burns November 2015 29 October 2012 – MDT convened • Improving surveillance of S. aureus BSI: – – – – Real-time surveillance Information for action – feedback and review of data Timely root cause analysis and action Calculation of rates of infection - ? Denominator – patient months, line days – Stratification of rates by BH dialysis unit Karen Burns November 2015 30 October 2012 – MDT convened • Standardisation of vascular catheter insertion – procedure, documentation – ICU, theatre, radiology, ward • Standardisation of vascular catheter maintenance – care bundles, procedures, dressings • Audit and feedback – are we doing what we’ve agreed to do? • Education of staff and patients • Ongoing promotion of fistula route • Plan for further MDT meetings Karen Burns November 2015 31 What did we do? • Q1 2013: Renal IPCN appointed • January 2013: Enhanced surveillance of renal S. aureus BSI • July 2013: Quarterly screening of haemodialysis patients for MRSA carriage: nasal, catheter exit site, other skin breaks, device sites as indicated: – – – – Tell patients why they’re being screened Do the screening – HD unit Process and report specimens – clinical micro lab and team Identify, communicate with and manage MRSA positive patients – nose positive, exit site positive, multiple sites positive - MDT – Follow-up screening post-decolonisation – Management of chronic MRSA carriers • We found no new MRSA carriers on our first round of screening: 2/173 patients positive, both previously known Karen Burns November 2015 32 Karen Burns November 2015 33 Our first six months • Eight S. aureus BSI (MSSA;5, MRSA;3) • Seven patients had prior positive microbiology results for S. aureus • Two patients had exit site infection • Six BSI secondary to infected vascular catheter • Two CRBSI arose within 48 hours of device insertion • Room to improve with regard to documentation of device insertion and device maintenance • Suboptimal personal hygiene an issue in three cases • Infection rates higher in acute HD setting Karen Burns November 2015 34 Ongoing work - 2014 • Maintain surveillance & feedback • Maintain quarterly MRSA screening – no new positive patients identified • Feedback results at unit level • Continue MDT meetings Karen Burns November 2015 35 New changes - 2014 • Increased ANTT training • Transition to Chlorprep applicator for exit site to facilitate ANTT • Unit level run charts, with latest data displayed in staff room • QIP with additional focus at HD unit CNM meetings • Patients and staff wear surgical mask for CVC care procedures • Staff providing education to patients on importance of sterile field during HD • Dermatology referral for patients with skin sensitivity issues • Exit site infection management protocol • Routine S. aureus decolonisation protocol pre-permcath insertion or AVG creation Karen Burns November 2015 36 New changes - 2014 ELECTIVE Permanent CVC/ AVG formation Regimen: Triclosan 1 % (Skinsan) skin wash daily for 5 days (2 of the 5 days hair to be washed with this also) Mupirocin 2% (Bactroban Nasal Ointment) intranasally, 3 times daily for 5 days Day before procedure Day of Procedure 1st Day after procedure 2nd day after procedure 3rd day after procedure Wash hair and body with Triclosan 1 % (Skinsan) and nasal Mupirocin 2%, 3 times a day Wash hair and body with Triclosan 1 % (Skinsan) and nasal Mupirocin 2%, 3 times a day Wash only body with Triclosan 1 % (Skinsan) and nasal Mupirocin 2%, 3 times a day Wash only body with Triclosan 1 % (Skinsan) and nasal Mupirocin 2%, 3 times a day Wash only body with Triclosan 1 % (Skinsan) and nasal Mupirocin 2%, 3 times a day Karen Burns November 2015 37 Karen Burns November 2015 38 The first two years • 12% reduction in renal S. aureus BSI due to vascular catheters • Reduction in S. aureus BSI infection rate in acute haemodialysis setting • More data gathered on infection risk factors: 2014 2013 S. aureus colonisation 6 10 Exit site/tunnel infections 3 5* Exit site irritation/sensitivity 4 0 Poor flows- requiring additional manipulation during treatment 3 2 Dwell time of CVC: >2years 2 1 Recent device insertion procedure (<1 week): 0 4 Recent holiday haemodialysis 1 1 Risk factors *3 initially had sensitivities to dressing/ cleaning agent Karen Burns November 2015 39 The third year (to end Q3 2015) • 64% reduction in vascular catheter related S. aureus BSI vs same period 2014 • 18% increase in vascular catheter line days Q1 – Q3 2015 • Ongoing education – standard precautions, hand hygiene, decolonisation protocol • ANTT intervention kit • Learning points shared from RCA findings • Electronic flags to identify patients with prior S. aureus infection Karen Burns November 2015 40 To wrap up… • HD patients are at-risk of infection • Risk escalates for HD patients with vascular catheters • While S. aureus is the major player in vascular catheter-related infection, other bugs can be implicated, particularly in acute HD and temporary catheter settings • The vascular catheter is not the cause of every haemodialysis patient’s SA-BSI Karen Burns November 2015 41 The key ingredients 1. Multi-disciplinary team work & communication 2. Consistent application of proven evidence-based interventions 3. Continuous quality improvement & keeping up-todate 4. Ongoing surveillance, root cause analysis, with timely feedback to those who need to know 5. Local leadership, enthusiasm and commitment to patient safety and quality of care Karen Burns November 2015 42 Updated national guidance 2013 2014 Karen Burns November 2015 43 Thanks to my colleagues & thanks to you for your attention karenburns@beaumont.ie Karen Burns November 2015 44