Neuromuscular & storage disorder
advertisement
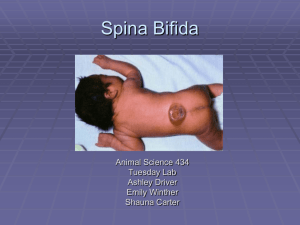
Cerebral palsy: Group of disorder result from non progressive brain damage during early development, the known causal factors include: 1 - maternal toxemia, 2prematurity, 3- peri natal anoxia, 4- kernicterous, 5- post natal brain infection, 6- post natal brain injury. The main consequence is development of neuromuscular in coordination, dystonia, weakness, spasticity, there may be convulsion, perceptual problems, speech disorder, & mental retardation or behavioral problems. Classification: According to motor dysfunction: 1- spastic palsy: account for 60% of all cases, there is increase muscle tone & hyper active ref lexes. 2- athetotic: there is continuous involuntary writhing movement. Tongue, & speech muscle may be involved. 3- ataxic: there is muscle in coordination during voluntary movement & balance is poor. 4- Rigid palsy: here the muscles are in constant state of contraction. 5- mixed type: a combination of spastic & athetotic palsy. According to topographic distribution of clinical signs: 1- Hemiplegic: appear as spastic palsy of the upper & lower limb on one side of the body, most of these children can walk. 2- diplegic affect mainly the lower limb. 3- total body involvement: affect all 4 limbs, trunk, neck & face with varying degree of severity, patient have low IQ. & unable to walk. Diagnosis: Early in infancy there is difficulty in sucking & swallowing & the mother notice that the baby fell stiff, later there is delay milestones “ sitting, walking…..” over 1 year it is important to examine the patient during sitting, standing, walking also to examine speech, hearing, visual acuity & mentality of the patient. Clinically: Child with CP. Cannot sit unsupported & tend to stand with the hip f lexed, adducted & internally rotated, the knee f lexed & feet in equinus, & the child cannot stand without support & any attempt to correct one spastic deformity tend to aggravate the other. Deformities encountered with CP. In the lower limb the hip held in f lexion, adduction & internal rotation, the knee held in f lexion & feet in equinus. in the upper limb the fingers held in spastic f lexion position which is increased by extending the wrist “ called fixed length reaction” In the spine in total body palsy: scoliosis & pelvic obliquity are common, kyphosis also quite common & may be severe enough to require surgical correction. Sensation usually present if not completely normal. Spina bifida: Is a congenital disorder in which the 2 halves of the posterior vertebral arch or several arches fail to fuse this embryonic defect occur within the first 6 wks. of gestation if this is associated with maldevelopment of neural tube & overlying skin is called dysraphisim usually occur in the lumber or lumbosacral region. If the neural element involved there may be paralysis & loss of sensation & sphencteric control. There are 2 types: 1- Spina bifida occulta: there is only midline defect between the laminae & nothing more, if several vertebrae are affected there are tell tale defect in the overlying skin such as dimple, pit, a tuft of hair. occasionally there are associated anomalies as tethering of the conus medullaris below L1, splitting of the spinal cord called diastematomyelia, cyst or lipoma of the cauda equina. 2- Spina bifida cystica (SBC): severe form of dysraphisim, the vertebral laminae are missing & the content of vertebral canal prolapsed through the defect; A) Meningocele: is the least disabling, account for 5% of SBC in which the spinal cord & nerve roots remain in there normal position, the dura mater open posteriorly & a CSF filled meningeal sac protrude under the skin, there is usually no neurological abnormality. B) Myelomeningocele: part of the spinal cord & nerve roots prolapsed together with the meningeal sac. If the neural tube is in it’s primitive state & the neural plate form part of the roof of the sac called open myelomeningocele or rachischisis. Myelomeningocele is always associated with neurological deficit below the level of the lesion & in open form it may be infected leading to severe abnormality& even death. Clinical features: Spina bifida oculta: usually discovered accidentally with no more than an isolated laminar defect however presence of midline dimple, a tuft of hair or a pigmented naevus signif y some thing more serious. Patient may present at any age with enuresis, urinary frequency or incontinence, there may also weakness & some loss of sensibility in the lower limb. X ray show the laminar defect, a midline ridge of bone suggest bifurcation of the cord called diastematomyelia. Spina bifida cystica: a sacular lesion over the lumbosacral spine is obvious at birth it may be covered with membrane or membrane & skin. In open myelomeningocele the neural element form the roof of the cyst. Meningocele is covered by normally locking skin. Deformities associated with spina bifida: are common these are hip dislocation, genu recurvatum, talipes & claw toes, such deformities may be due to 1 - muscle imbalance 2- abnormal positioning of the limb in utero or after birth 3 - it may be an associated anomalies independent of paralysis. Arthogryposis mutiplex congenita AGMC: Congenital disorder in which there is non progressive restriction of movement due to soft tissue contracture. It could be neuropathic or myopathic in origin & is characterized by 1) soft tissue contracture 2) stiffness of several joints 3) shapeless cylindrical limb 4) absence of skin creases. Deformities encountered with AGMC are: 1) Rigid equinovarus is common & difficult to treat, operative correction is often necessary & even then recurrence is very high. 2) Hip dislocation often need open reduction. 3) Spinal deformities may develop with myopathic AGMC. Deformities & contractures develop in utero & remain largely unchanged through out life. Treatment: initially with manipulation & splintage of deformed joint later tendon release , tendon transfer & osteotomy may become necessary. Muco poly saccharidosis: Glycos amino glycans (GAG) is poly saccharide form the side chain of proteoglycans which are the major component of the matrix in bone, cartilage, inter vertebral disc, synovium & other connective tissues. Lack of enzymes essential in the degenerative pathway of the proteoglycans cause accumulation of the partially degraded GAG in lysosome in the liver, spleen, bones & other tissues & spill over in the blood & urine where they can be detected by suitable biochemical test. Clinical features: MPS are group of disorder differ according to the specific enzyme deficiency & type of GAG storage. All are autosomal recessive except hunter disease which is x-linked recessive. As group they have certain recognizable features; 1) excessive short stature 2) vertebral deformities 3) coarse facieses 4) hepatosplenomegaly 5) in some cases mental retardation X-ray : show bone dysplasia affect the vertebral bodies, epiphysis & metaphysis, at least 10 different disorders are recognized; the least rare 3 are: 1) Hurler syndrome MPS I: