Neural Tube Defects and Hydrocephaly
advertisement

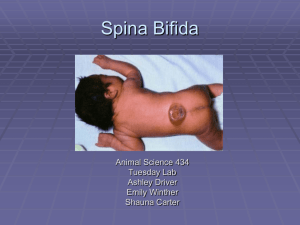
Infancy Health Problems II •Neural Tube Defects •Hydrocephaly •Anencephaly •Pyloric Stenosis •Intusseption •Hirschsprung’s Disease •Tracheo Esophageal Fistula (TEF) Neural Tube Defects 50% or more from folic acid deficiency; others are multifactoral etiology Neural tube = embryonic beginning for the brain & spinal column Brain & spinal cord encased in meninges/bone Neural tube should close ~ 30 days after conception; defect in closure may involve entire length of neural tube or small area Most common defects: anencephaly & spina bifida Spina Bifida or Myelodysplasia Failure of the bony (osseous) spine to close Two types: Spina bifida occulta – not visible externally Spina bifida cystica – visible, saclike protrusion Meningocele Myelomeningocele – most commonly referred to by the term Spina Bifida Spina Bifida Occulta Usually lumbosacral L5-S1 Skin indicators: Sacral dimple, angioma or port-wine nevus Sacral tufts of dark hair or lipoma Usually no problems unless there is an adhesion to bony or fixed structure Altered gait Bowel/bladder problems Foot deformities These usually not evident in early infancy Myelomeningocele vs Meningocele Meningocele – contains meninges and spinal fluid – no neural elements No neurological deficits Myelomeningocele – also contains nerves Anywhere along spinal column Varying & serious degrees of neuro deficit Location & magnitude of defect determine extent of impairment Below L2, flaccid paralysis of lower extremities & sensory deficit; bowel & bladder dysfunction Below S3 – no motor impairment; bowel/bladder def. Differentiating Meningocele from Myelomeningocele By definition, these two neural tube defects differ based on the presence or absence of the spinal cord or cauda equina within the sac at the base of the spine. Meningocele—fluid only Myelomeningocele—fluid and spinal cord both What determines the severity of Myelomeningocele?? The degree of neurological deficit is directly related to the level of the spinal cord defect and its extent. If only the bottom of the spinal cord is involved (conus), there may be only bowel and bladder dysfunction, while the most extensive lesions can result in total paralysis of the legs with accompanying bowel and bladder dysfunction. It is because of the varying neurological manifestations of meningomyelocele that there has been so much controversy regarding appropriate treatment. Variations in Spinal Cord Anomalies Normal Spina bifida occulta Meningocele Myelomeningocele Myelomeningocele Lateral view Statistics showing improvement with Folic Acid supplements Folic acid was deemed mandatory for certain foods after 1992. Plus there was the big educational push to have women take supplemental Folic Acid as soon as they thought about getting pregnant. CDC Stats on Folic Acid Folic Acid Quiz Management Prevention of infection & trauma to the “sac” – keep covered w/sterile saline dressing; monitor closely Observe for early signs of infection ↑temp; no rectal for this babies!! Nuchal rigidity, irritability, lethargy, ↑ICP Prone position; no diapers Assess neurological deficits Surgical repair in 12 – 72hrs. of birth How to manage bowel and bladder dysfunction Neurogenic bladder is one of the primary dysfunctions that children with spina bifida encounter. Reference for lay persons on management Reference from NIH on management Latex Allerg;y All children with any neural tube defect must be treated as if they had a LATEX ALLERGY ! See pp. 408-409 Hockenberry , 9th ed. and pp. 1640-1641 10th ed. There are various resources available to give families re: environmental sources of latex. The Spina Bifida Association offers a handout with resources. Hydrocephaly—why study it with Neural Tube Defects Hydrocephaly is commonly associated with Meningocele and Myelomeningocele. It is critical for nurses to assess the head circumference of all babies with NTD daily to note changes in the head size so that interventions can be made to prevent complications from ICP. Common signs and sx of Hydrocephaly in neonate and infancy Increasing head circumference Bulging fontanel 7 separated sutures “setting sun eyes” Frontal bossing Macewen sign High-pitched cry Changes in behavior—in older child Nausea & vomiting—in older child where fontanels are closed Hydrocephalus Commonly seen with myelomeningocele 80-85% will develop this May not be obvious at first; may appear after closure of defect Critical to measure head circumference daily & palpate fontanel for changes Also can be other congenital causes or acquired as a result of infection, neoplasm or hemorrhage It is a syndrome that results from disturbances in dynamics of CSF Anatomy of the Ventricles of the Brain This shows a picture of the ventricles of the brain, so that you can get a visual feel for how the obstruction may cause increased intracranial pressure. Web Site Alert!! This web site gives lots of facts about hydrocephalus. It is easy to read and understand. http://www.ninds.nih.gov/disorders/hydrocephalus /detail_hydrocephalus.htm What Happens?? CSF circulates throughout the ventricular system & is then absorbed within the subarachnoid spaces 2 problems can occur: Communicating hydrocephalus: impaired absorption of CSF Noncommunicating hydrocephalus: obstruction to flow of CSF occurs Table 11-3, p. 443, 9th ed. and Table 32-8, p. 1485, 10th ed. has specifics Either way it leads to ↑ICP and this is serious! Ventriculo-peritoneal Shunts Here are some examples of VP shunts that may be used to help manage hydrocephaly. Website on Endoscopic Third Ventriculostomy Hydrocephalus: Initial Management Treatment of excessive CSF (shunt) – ventriculoperitoneal (VP) most common Treatment of complications – mainly related to the shunt Infection – greatest risk first 2 mos Malfunction – will see ↑ICP Manage problems related to development 2/3 are intellectually normal Post Op Care Must be alert for signs of Increased ICP Post op: daily measurements of FOC and palpation of fontanels for size, signs of bulging, tenseness, separation Initially keep flat w/o pressure on incision, gradually HOB elevated Neuro assessment, VS, I&O Abdominal distention (peritonitis or ileus) Signs of infection: temp↑, poor feeding, vomiting, seizures, ↑LOC Inspect incision line for redness, drainage (test any drainage for glucose in case it is CSF) Discharge Information Must teach how to recognize signs of infection and shunt malformation Refer to p. 1617, Box 37-1 (9th ed.) and p. 1428, Box 32-1 (10th ed.) for summary of clinical manifestations of ↑ICP in infants and children Make appropriate referrals, ie early childhood programs, early intervention services, support groups What is Arnold Chiari Malformation? Arnold Chiari Malformations are a form of hydrocephaly that was discovered by Dr. Chiari in the 1890’s. Chiari I – IV malformations may be an anomaly that people live with with minimal sx. MRI has significantly helped in the dx. Chiari Type II is often found in children with Myelomenigocele. NIH website with information Anencephaly– What is it and how do we help those families who have babies born with it? This website gives resources as well as some explanation of what it is. Here are family stories of their Children Anencephaly Incompatible with life: stillborn or live hours to weeks Absence of both cerebral hemispheres Brainstem function may be intact Cause of death usually respiratory failure Management: comfort measures, family support, discussion of end-of-life issues like organ donation, possible referral to hospice Hypertrophic Pyloric Stenosis Def: results when the circular areas of muscle surrounding the pylorus hypertrophy & block gastric emptying. Etiology: Cause unknown, heredity, possibly. Incident: 1 in 500 live births ♂( x 5) > ♀ (1) Pathophysiology: Pylorus narrows because of progressive hypertrophy and hyperplasia of the circular pyloric muscle. This leads to obstruction of the pyloric sphincter, with subsequent gastric distention, dilatation, and hypertrophy. Hypertrophic Pyloric Stenosis Pyloromyotomy, creation of an incision along the anterior pylorus to split the muscle, is performed to relieve the obstruction. Link to diagram of pyloric stenosis and surgical incision Hypertrophic Pyloric Stenosis Assessment preoperatively: Progressive, projectile, non-bilious vomiting occurs. Movable, palpable, firm, olive- shaped mass in the right upper quadrant Irritability, hunger, and crying. Sunken fontanels, dry mucus membranes, and decreased urine output, constipation, jaundice, & metabolic alkalosis. (Dehydration) U/S and upper GI series shows delayed gastric emptying and hypertrophied pylorus. Hypertrophic Pyloric Stenosis Labs: 1.↑pH & ↑bicarbonate level = metabolic alkalosis 2. Serum chloride, sodium, potassium ≈ decreased 3. HCT, Hgb ↑ = hemoconcentration Management: Preoperative management: Monitor for dehydration—strict I &O, daily weight Restore hydration through IV fluids and electrolytes (usually glucose and electrolytes including K+ e.g. D5 1/2 NS with 20 KCl. NPO, but may suck on pacifier Maintain NG tube patency if part of pre-op management Careful monitoring of VS Accurate documentation of any vomiting and diarrhea Teach parents about pathology and treatment after primary MD. Post-operative care: Maintain IV fluids until taking adequate po. Small frequent feedings of clear liquids 4-6 hours after surgery. If retained, strict diet regimen of gradual advancement of feedings until normal formula has been resumed. Breastfed babies may be given breastmilk in a bottle initially, and then allowed to go to breast. NG may be maintained for a short time post op, not always. Monitor I&O carefully Manage pain with analgesics ‘round the clock’—using appropriate pain scale for age of infant Monitor surgical site for signs of infection. Not uncommon to have vomiting in first 24-48 hrs. Intussusception Def: Bowel telescopes onto itself. Invagination or telescoping of 1 portion of the intestine into another, resulting in obstruction behind the defect. Epidemiology: Most common cause of intestinal obstruction 3 yrs & under Rare before 3 months of age Peak age: 5 to 9 months Less common after 36 months Link was made to the Rotavirus vaccine initially, but new vaccines have been found safe, but should only be given at designated ages Intussusception Telescoping of the intestine leading to possible ischemia Common Symptoms: •Acute pain, vomiting •Current-jelly-like stools •Apathy •Abdomen tender, distended Treatment: Barium enema and/or surgery Intussusception Etiology: Idiopathic (90%) Pathologic lesion Risk factors: Cystic Fibrosis Indwelling gastrointestinal tubes Recent infections Acute Gastroenteritis Intussusception - Symptoms Acute: Child appears well between episodes of pain Vomiting Abdominal pain: Acute pain with sudden onset Colicky with paroxysms and of pain @ 20 minute intervals Stool changes Watery stools @ first (12-24 hours) Red Current Jelly Stools later (bloody mucus) Lethargy Chronic: Diarrhea Anorexia Weight loss Occasional vomiting Periodic pain Hirschsprung Disease Congenital Aganglionic Megacolon Definition: congenital anomaly results from absence of ganglion cells in colon which then results in a mechanical obstruction d/t inadequate motility from one section of the colon. Etiology: Congenital defect ;1:5000 live births 4:1 ratio [affects 4x’s >♂’s than ♀] Down's syndrome is frequently associated with it. Genitourinary abnormalities accompany it. Hirschsprung’s Disease Hirschsprung Disease cont. Pathophysiology: Lack of the intramural ganglionic cells Lack of innervations: Hypertonic bowel results in functional stenosis Internal sphincter does not relax Partial or complete colonic obstruction Proximal intestine markedly dilated with feces, gas. Hirschsprung Disease cont. Symptoms: Newborns: • Failure to pass meconium in first 24-48 hours • Bile-stained emesis * • Abdominal distention • Reluctance to eat Infants: Failure to thrive, inadequate wt gain Constipation Abdominal distention Vomiting Episodic diarrhea Ominous Signs: bloody diarrhea, fever, severe lethargy Toddlers and older children: Chronic constipation Foul-smelling stools, ribbon like stools Abdominal distention Visible peristalsis Palpable fecal mass Malnourishment Signs of anemia and Hypoproteinemia Hirschsprung Disease cont. Assessment: 1. Rectal exam: absence of stool and rectum 2. X-ray: enlarged portion of the colon 3. Rectal biopsy: absence of ganglion cells Treatment: 1. Remove ganglionic bowel 2. Temporary colostomy 3. Reanastomosis around age two Nursing considerations: 1. Prepare for surgical procedure 2. Teach ostomy care 3. Monitor fluid and electrolytes 4. Monitor nutrition 5. Help with body image Tracheoesophageal Fistula (TEF) Esophageal Atresia (EA) Atresia: absence of normal opening or normally patent lumen Failure of esophagus to develop as a continuous passage and/or trachea & esophagus do not separate May occur separately or in combination High association w/cardiac anomalies Tracheoesophageal Fistula Signs / Symptoms /Management 3 C’s: Coughing Choking episodes w/eating Cyanosis may occur d/t aspiration of formula or saliva → laryngospasm and/or apnea Frothy saliva in mouth & nose; drooling Can literally drown if esophagus is connected to trachea Attempt made to pass NG/OG catheter is unsuccessful Polyhydraminois & SGA are big warning signs Pure Esophageal Atresia Fistula from trachea to upper esophageal segment Blind pouch proximal esophagus; distal is connected to trachea or bronchus by short fistula near bifurcation Fistula from trachea to upper and lower segments of esophagus “H type” – normal trachea and esophagus but fistula connects them Management Goal: prevent aspiration pneumonia, ensure hydration & nutrition Immediately NPO; IV fluids started Antibiotics started d/t ↑ risk of aspiration Frequent suctioning & HOB ↑30° Gastrostomy frequently done Surgery – usually completed in 1-2 tries Near 100% survival rate if no other problems May have long term feeding problems so need close monitoring Post Op and Discharge Gastrostomy feedings at first, then oral Always begin w/water & close supervision Assess for skin breakdown & provide care Provide infant stimulation, pacifier, til able to suck from breast/bottle Observe for respiratory problems and teach S/S to parents; teach CPR Extreme care when introducing foods Increased risk for GERD Refer to Care Plan in book p.438 (9th ed.), p. 1111 (10th ed.) The End! Surgical Repair of TEF