reading lesson 1 and 2
advertisement
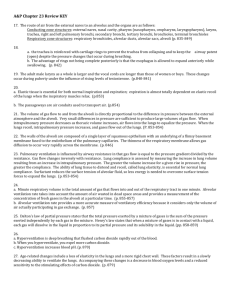
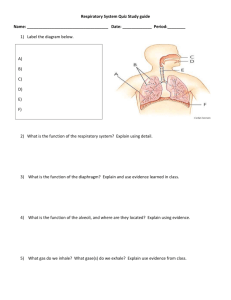
The elephant!Did you know? Elephants have no pleural cavity Elephant lungs attach directly to the walls of the chest cavity and to the diaphragm Respiratory movements are dependent on chest musculature (not on inflating lungs by negative pressure in the pleural cavity, as is usual in mammals) The respiratory system of the elephant is quite exceptional in a number of ways. The elephant lacks a pleural cavity. This means the lungs are directly attached to the walls of the chest cavity and to the diaphragm. Thus respiratory movements are solely dependent on chest musculature, since there is no mechanism of inflating the lungs by negative pressure in the pleural cavity as is usual in mammals. As a result of this unique physiology, the elephant would find it difficult to breathe if any restraint or pressure is placed on the movement of the chest and diaphragm, essentially over time suffocating from its own tremendous weight. Air enters the lungs through internal nares which are located high on the forehead. The position of the nares is indicated by the plate-size circle of skin. An elephant can breathe through its mouth as well as through its trunk, so it can retain water or dust in the trunk without having to hold its breathe. Respiratory system The respiratory system is the anatomical system of an organism that introduces respiratory gases to the interior and performs gas exchange. In humans and other mammals, the anatomical features of the respiratory system include airways, lungs, and the respiratory muscles. Molecules of oxygen and carbon dioxide are passively exchanged, by diffusion, between the gaseous external environment and the blood. This exchange process occurs in the alveolar region of the lungs.[1] Other animals, such as insects, have respiratory systems with very simple anatomical features, and in amphibians even the skin plays a vital role in gas exchange. Plants also have respiratory systems but the directionality of gas exchange can be opposite to that in animals. The respiratory system in plants also includes anatomical features such as holes on the undersides of leaves known as stomata.[2] Comparative anatomy and physiology Horses Horses are obligate nasal breathers which means that they are different from many other mammals because they do not have the option of breathing through their mouths and must take in oxygen through their noses. Elephants The elephant is the only animal known to have no pleural space. Rather, the parietal and visceral pleura are both composed of dense connective tissue and joined to each other via loose connective tissue.[3] This lack of a pleural space, along with an unusually thick diaphragm, are thought to be evolutionary adaptations allowing the elephant to remain underwater for long periods of time while breathing through its trunk which emerges as a snorkel.[4] Birds The respiratory system of birds differs significantly from that found in mammals, containing unique anatomical features such as air sacs. The lungs of birds also do not have the capacity to inflate as birds lack a diaphragm and a pleural cavity. Gas exchange in birds occurs between air capillaries and blood capillaries, rather than in alveoli. See Avian respiratory system for a detailed description of these and other features. Reptiles The anatomical structure of the lungs is less complex in reptiles than in mammals, with reptiles lacking the very extensive airway tree structure found in mammalian lungs. Gas exchange in reptiles still occurs in alveoli however, reptiles do not possess a diaphragm. Thus, breathing occurs via a change in the volume of the body cavity which is controlled by contraction of intercostal muscles in all reptiles except turtles. In turtles, contraction of specific pairs of flank muscles governs inspiration or expiration.[5] See also reptiles for more detailed descriptions of the respiratory system in these animals. Amphibians Both the lungs and the skin serve as respiratory organs in amphibians. The skin of these animals is highly vascularized and moist, with moisture maintained via secretion of mucus from specialized cells. While the lungs are of primary importance to breathing control, the skin's unique properties aid rapid gas exchange when amphibians are submerged in oxygenrich water.[6] Fish In most fish respiration takes place through gills. (See also aquatic respiration.) Lungfish, however, do possess one or two lungs. The labyrinth fish have developed a special organ that allows them to take advantage of the oxygen of the air. Anatomy in invertebrates Insects Air enters the respiratory systems of most insects through a series of external openings called spiracles. These external openings, which act as muscular valves in some insects, lead to the internal respiratory system, a densely networked array of tubes called tracheae. The scientific tracheal system within an individual is composed of interconnecting transverse and longitudinal tracheae which maintain equivalent pressure throughout the system. These tracheae branch repeatedly, eventually forming tracheoles, which are blind-ended, waterfilled compartments only one micrometer in diameter.[7] It is at this level of the tracheoles that oxygen is delivered to the cells for respiration. The trachea are water-filled due to the permeable membrane of the surrounding tissues. During exercise, the water level retracts due to the increase in concentration of lactic acid in the muscle cells. This lowers the water potential and the water is drawn back into the cells via osmosis and air is brought closer to the muscle cells. The diffusion pathway is then reduced and gases can be transferred more easily. Insects were once believed to exchange gases with the environment continuously by the simple diffusion of gases into the tracheal system. More recently, however, large variation in insect ventilatory patterns have been documented and insect respiration appears to be highly variable. Some small insects do demonstrate continuous respiration and may lack muscular control of the spiracles. Others, however, utilize muscular contraction of the abdomen along with coordinated spiracle contraction and relaxation to generate cyclical gas exchange patterns and to reduce water loss into the atmosphere. The most extreme form of these patterns is termed discontinuous gas exchange cycles (DGC).[8] Mollusks Mollusks generally possess gills that allow exchange of oxygen from an aqueous environment into the circulatory system. These animals also possess a heart that pumps blood which contains hemocyaninine as its oxygen-capturing molecule. Hence, this respiratory system is similar to that of vertebrate fish. The respiratory system of gastropods can include either gills or a lung. Physiology in mammals For more detailed descriptions see also Respiratory physiology or Respiration. Ventilation In respiratory physiology, ventilation (or ventilation rate) is the rate at which gas enters or leaves the lung. It is categorised under the following definitions: Measurement Minute ventilation Symbol Example Equation Description tidal volume the total volume of gas * respiratory entering the lungs per rate[1][2] minute. Alveolar ventilation Dead space ventilation (tidal volume - dead space) Example * respiratory rate [1] Example the volume of gas per unit time that reaches the alveoli, the respiratory portions of the lungs where gas exchange occurs. dead space * respiratory rate[3] the volume of gas per unit time that does not reach these respiratory portions, but instead remains in the airways (trachea, bronchi, etc.). Control Ventilation occurs under the control of the autonomic nervous system from parts of the brain stem, the medulla oblongata and the pons. This area of the brain forms the respiration regulatory center, a series of interconnected brain cells within the lower and middle brain stem which coordinate respiratory movements. The sections are the pneumotaxic center, the apneustic center, and the dorsal and ventral respiratory groups. This section is especially sensitive during infancy, and the neurons can be destroyed if the infant is dropped and/or shaken violently. The result can be death due to "shaken baby syndrome".[9] Inhalation Inhalation is initiated by the diaphragm and supported by the external intercostal muscles. Normal resting respirations are 10 to 18 breaths per minute, with a time period of 2 seconds. During vigorous inhalation (at rates exceeding 35 breaths per minute), or in approaching respiratory failure, accessory muscles of respiration are recruited for support. These consist of sternocleidomastoid, platysma, and the scalene muscles of the neck. Pectoral muscles and latissimus dorsi are also accessory muscles. Under normal conditions, the diaphragm is the primary driver of inhalation. When the diaphragm contracts, the ribcage expands and the contents of the abdomen are moved downward. This results in a larger thoracic volume and negative pressure (with respect to atmospheric pressure) inside the thorax. As the pressure in the chest falls, air moves into the conducting zone. Here, the air is filtered, warmed, and humidified as it flows to the lungs. During forced inhalation, as when taking a deep breath, the external intercostal muscles and accessory muscles aid in further expanding the thoracic cavity. During inhalation the diaphragm contracts. Exhalation Exhalation is generally a passive process; however, active or forced exhalation is achieved by the abdominal and the internal intercostal muscles. During this process air is forced or exhaled out. The lungs have a natural elasticity: as they recoil from the stretch of inhalation, air flows back out until the pressures in the chest and the atmosphere reach equilibrium.[10] During forced exhalation, as when blowing out a candle, expiratory muscles including the abdominal muscles and internal intercostal muscles, generate abdominal and thoracic pressure, which forces air out of the lungs. Gas exchange The major function of the respiratory system is gas exchange between the external environment and an organism's circulatory system. In humans and mammals, this exchange facilitates oxygenation of the blood with a concomitant removal of carbon dioxide and other gaseous metabolic wastes from the circulation. As gas exchange occurs, the acid-base balance of the body is maintained as part of homeostasis. If proper ventilation is not maintained, two opposing conditions could occur: respiratory acidosis, a life threatening condition, and respiratory alkalosis. Upon inhalation, gas exchange occurs at the alveoli, the tiny sacs which are the basic functional component of the lungs. The alveolar walls are extremely thin (approx. 0.2 micrometres). These walls are composed of a single layer of epithelial cells (type I and type II epithelial cells) close to the pulmonary capillaries which are composed of a single layer of endothelial cells. The close proximity of these two cell types allows permeability to gases and, hence, gas exchange. This whole mechanism of gas exchange is carried by the simple phenomenon of pressure difference. When the atmospheric pressure is low outside, the air from lungs flow out. When the air pressure is low inside, then the vice versa. Non-respiratory functions Lung Defense Mechanisms Airway epithelial cells can secrete a variety of molecules that aid in lung defense. Secretory immunoglobulins (IgA), collectins (including Surfactant A and D), defensins and other peptides and proteases, reactive oxygen species, and reactive nitrogen species are all generated by airway epithelial cells. These secretions can act directly as antimicrobials to help keep the airway free of infection. Airway epithelial cells also secrete a variety of chemokines and cytokines that recruit the traditional immune cells and others to site of infections. Metabolic & Endocrine Functions of the Lungs In addition to their functions in gas exchange, the lungs have a number of metabolic functions. They manufacture surfactant for local use, as noted above. They also contain a fibrinolytic system that lyses clots in the pulmonary vessels. They release a variety of substances that enter the systemic arterial blood and they remove other substances from the systemic venous blood that reach them via the pulmonary artery. Prostaglandins are removed from the circulation, but they are also synthesized in the lungs and released into the blood when lung tissue is stretched. The lungs also activate one hormone; the physiologically inactive decapeptide angiotensin I is converted to the pressor, aldosterone-stimulating octapeptide angiotensin II in the pulmonary circulation. The reaction occurs in other tissues as well, but it is particularly prominent in the lungs. Large amounts of the angiotensinconverting enzyme responsible for this activation are located on the surface of the endothelial cells of the pulmonary capillaries. The converting enzyme also inactivates bradykinin. Circulation time through the pulmonary capillaries is less than 1 s, yet 70% of the angiotensin I reaching the lungs is converted to angiotensin II in a single trip through the capillaries. Four other peptidases have been identified on the surface of the pulmonary endothelial cells. Vocalization The movement of gas through the larynx, pharynx and mouth allows humans to speak, or phonate. Vocalization, or singing, in birds occurs via the syrinx, an organ located at the base of the trachea. The vibration of air flowing across the larynx (vocal chords), in humans, and the syrinx, in birds, results in sound. Because of this, gas movement is extremely vital for communication purposes. Temperature control Panting in dogs and some other animals provides a means of controlling body temperature. This physiological response is used as a cooling mechanism. Coughing and sneezing Irritation of nerves within the nasal passages or airways, can induce coughing and sneezing. These responses cause air to be expelled forcefully from the trachea or nose, respectively. In this manner, irritants caught in the mucus which lines the respiratory tract are expelled or moved to the mouth where they can be swallowed. Development in People Humans and mammals Further information: Development of human lung The respiratory system lies dormant in the human fetus during pregnancy. At birth, the respiratory system becomes fully functional upon exposure to air, although some lung development and growth continues throughout childhood. Pre-term birth can lead to infants with under-developed lungs. These lungs show incomplete development of the alveolar type II cells, cells that produce surfactant. The lungs of pre-term infants may not function well because the lack of surfactant leads to increased surface tension within the alveoli. Thus, many alveoli collapse such that no gas exchange can occur within some or most regions of an infant's lungs, a condition termed respiratory distress syndrome. Basic scientific experiments, carried out using cells from chicken lungs, support the potential for using steroids as a means of furthering development of type II alveolar cells.[11] In fact, once a pre-mature birth is threatened, every effort is made to delay the birth, and a series of steroid shots is frequently administered to the mother during this delay in an effort to promote lung growth.[12] Disease Disorders of the respiratory system can be classified into four general areas: Obstructive conditions (e.g., emphysema, bronchitis, asthma) Restrictive conditions (e.g., fibrosis, sarcoidosis, alveolar damage, pleural effusion) Vascular diseases (e.g., pulmonary edema, pulmonary embolism, pulmonary hypertension) Infectious, environmental and other "diseases" (e.g., pneumonia, tuberculosis, asbestosis, particulate pollutants): Coughing is of major importance, as it is the body's main method to remove dust, mucus, saliva, and other debris from the lungs. Inability to cough can lead to infection. Deep breathing exercises may help keep finer structures of the lungs clear from particulate matter, etc. The respiratory tract is constantly exposed to microbes due to the extensive surface area, which is why the respiratory system includes many mechanisms to defend itself and prevent pathogens from entering the body. Disorders of the respiratory system are usually treated internally by a pulmonologist and Respiratory Therapist. Plants Plants use carbon dioxide gas in the process of photosynthesis, and exhale oxygen gas as waste. The chemical equation of photosynthesis is 6 CO2 (carbon dioxide) and 6 H2O (water) and that makes 6 O2 (oxygen) and C6H12O6 (glucose). Respiration is the opposite of that. However, plants also sometimes respire as humans do, taking in oxygen and producing carbon dioxide. Plant respiration is limited by the process of diffusion. Plants take in carbon dioxide through holes on the undersides of their leaves known as stoma or pores. However, most plants require little air.[citation needed] Most plants have relatively few living cells outside of their surface because air (which is required for metabolic content) can penetrate only skin deep. However, most plants are not involved in highly aerobic activities, and thus have no need of these living cells Vertebrate trachea Conducting passages. Laryngoscopic view of interior of larynx. (Trachea labeled at bottom.) Gray's subject #237 1084 Artery tracheal branches of inferior thyroid artery Vein brachiocephalic vein, azygos vein accessory hemiazygos vein MeSH Trachea In tetrapod anatomy the trachea, or windpipe, is a tube that connects the pharynx or larynx to the lungs, allowing the passage of air. It is lined with pseudostratified ciliated columnar epithelium cells with goblet cells that produce mucus. This mucus lines the cells of the trachea to trap inhaled foreign particles that the cilia then waft upward toward the larynx and then the pharynx where it can be either swallowed into the stomach or expelled as phlegm. Despite the name, not all vertebrates have a trachea, only non-fish. The name is used in contrast with invertebrate trachea, a structure in arthropod anatomy. In non-humans Allowing for variations in the length of the, the trachea in other mammals is, in general, similar to that in humans. In general, the reptilian trachea is also similar.[1] In birds, the trachea runs from the pharynx to the syrinx, from which the primary bronchi diverge. Swans have an unusually elongated trachea, part of which is coiled beneath the sternum; this may act as a resonator to amplify sound. In some birds, the cartilagenous rings are complete, and may even be ossified.[1] In amphibians, the trachea is normally extremely short, and leads directly into the lungs, without clear primary bronchi. A longer trachea is, however, found in some long-necked salamanders, and in caecilians. While there are irregular cartilagenous nodules on the amphibian trachea, these do not form the rings found in amniotes.[1] The only vertebrate to have lungs, but no trachea, is Polypterus, in which the lungs arise directly from the pharynx.[1] In humans In humans, the trachea passes ventrally to the esophagus, dorsally to the ascending aortic arch, but the left main bronchus that the trachea gives off passes ventrally to the descending aortic arch. The trachea has an inner diameter of about 21 to 27 millimetres (0.83 to 1.1 in) and a length of about 10 to 16 centimetres (3.9 to 6.3 in). It commences at the larynx, level with the fifth cervical vertebra, and bifurcates into the primary bronchi at the vertebral level of T4/T5. There are about fifteen to twenty incomplete C-shaped cartilaginous rings that reinforce the anterior and lateral sides of the trachea to protect and maintain the airway. The trachealis muscle connects the ends of the incomplete rings and contracts during coughing, reducing the size of the lumen of the trachea to increase the air flow rate. The esophagus lies posteriorly to the trachea. The cartilaginous rings are incomplete to allow the trachea to collapse slightly so that food can pass down the esophagus. A flap-like epiglottis closes the opening to the larynx during swallowing to prevent swallowed matter from entering the trachea. Lined with respiratory epithelium. Tracheal diseases and conditions The following are diseases and conditions that affect the trachea: Choking Tracheotomy, a surgical procedure on the neck to open a direct airway through an incision in the trachea Tracheomalacia (weakening of the tracheal cartilage) o Tracheal collapse (in dogs) Tracheobronchial injury (perforation of the trachea or bronchi) Mounier-Kuhn syndrome (causes abnormal enlargement of the trachea) In 2008, a Columbian woman received a trachea transplant using her own stem cells so her body would not reject the transplant.[2] In June 2011, surgeons in the Swedish Karolinska University Hospital led by Professor Paolo Macchiarini performed the first synthetic windpipe transplant on a 36-year-old African man, Andemariam Teklesenbet Beyene. [3][4] GOBLET CELLS Goblet cells are glandular simple columnar epithelial cells whose sole function is to secrete mucin, which dissolves in water to form mucus. They use both apocrine and merocrine methods for secretion. The majority of the cell's cytoplasm is occupied by mucinogen granules, except at the bottom. Rough endoplasmic reticulum, mitochondria, the nucleus, and other organelles are concentrated in the basal portion. The apical plasma membrane projects microvilli to increase surface area for secretion. Recent study suggests that glycoprotein is located inside goblet cells. It is an organ-specific antigen in the gut. Contents Locations They are found scattered among the epithelial lining of organs, such as the intestinal and respiratory tracts.[1] They are found inside the trachea, bronchus, and larger bronchioles in respiratory tract, small intestines, the colon, and conjunctiva in the upper eyelid . They may be an indication of metaplasia, such as in Barrett's esophagus. Histology In mucicarmine stains, deep red mucin found within goblet cell bodies. The nuclei of goblet cells tend to be displaced toward the basal end of the cell body, leading to intense basophilic staining Pseudostratified columnar epithelium Pseudostratified columnar epithelium Transverse section of tracheal tissue. Note that image is incorrectly labeled "ciliated stratified epithelium" at upper right. Code TH H2.00.02.0.02021 A pseudostratified epithelium is a type of epithelium that, though comprising only a single layer of cells, has its cell nuclei positioned in a manner suggestive of stratified epithelia. As it rarely occurs as squamous or cuboidal epithelia, it is usually considered synonymous with the term pseudostratified columnar epithelium. The term pseudostratified is derived from the appearance of this epithelium in section which conveys the erroneous (pseudo means false) impression that there is more than one layer of cells, when in fact this is a true simple epithelium since all the cells rest on the basal lamina. The nuclei of these cells, however, are disposed at different levels, thus creating the illusion of cellular stratification. Not all ciliated cells extend to the luminal surface; such cells are capable of cell division providing replacements for cells lost or damaged. Pseudostratified epithelia function in secretion or absorption. If a specimen looks stratified but has cilia, then it is a pseudostratified ciliated epithelium, since stratified epithelia do not have cilia. Three types of epithelium occur: Squamous is flattened cells. Cuboidal is cube shaped cells. Columnar consists of elongated cells. Bronchus Anatomy The trachea (windpipe) divides into two main bronchi (also mainstem bronchi), the left and the right, at the level of the sternal angle at the anatomical point known as the carina. The right main bronchus is wider, shorter, and more vertical than the left main bronchus. The right main bronchus subdivides into three lobar bronchi, while the left main bronchus divides into two. The lobar bronchi divide into tertiary bronchi, also known as segmentalinic bronchi, each of which supplies a bronchopulmonary segment. A bronchopulmonary segment is a division of a lung separated from the rest of the lung by a connective tissue septum. This property allows a bronchopulmonary segment to be surgically removed without affecting other segments. There are ten segments per lung, but due to anatomic development, several segmental bronchi in the left lung fuse, giving rise to eight. The segmental bronchi divide into many primary bronchioles which divide into terminal bronchioles, each of which then gives rise to several respiratory bronchioles, which go on to divide into two to 11 alveolar ducts. There are five or six alveolar sacs associated with each alveolar duct. The alveolus is the basic anatomical unit of gas exchange in the lung. There is hyaline cartilage present in the bronchi, present as irregular rings in the larger bronchi (and not as regular as in the trachea), and as small plates and islands in the smaller bronchi. Smooth muscle is present continuously around the bronchi. In the mediastinum, at the level of the fourth thoracic vertebra, the trachea divides into the right and left primary bronchi. The bronchi branch into smaller and smaller passageways until they terminate in tiny air sacs called alveoli. The cartilage and mucous membrane of the primary bronchi are similar to those in the trachea. As the branching continues through the bronchial tree, the amount of hyaline cartilage in the walls decreases until it is absent in the smallest bronchioles. As the cartilage decreases, the amount of smooth muscle increases. The mucous membrane also undergoes a transition from ciliated pseudostratified columnar epithelium to simple cuboidal epithelium to simple squamous epithelium. The alveolar ducts and alveoli consist primarily of simple squamous epithelium, which permits rapid diffusion of oxygen and carbon dioxide. Exchange of gases between the air in the lungs and the blood in the capillaries occurs across the walls of the alveolar ducts and alveoli. Role in disease Bronchitis is defined as inflammation of the bronchi. There are two main types: acute and chronic. Acute bronchitis is usually caused by viral or bacterial infections. Chronic bronchitis is a form of COPD, usually associated with smoking or long-term exposure to irritants. Asthma is hyperreactivity of the bronchi with an inflammatory component, often in response to allergens. While the left mainstem bronchus departs from the trachea at an angle, the right mainstem bronchus is almost a vertical continuation of the trachea. This anatomy predisposes the right lung to several problems: If food, liquids, or foreign bodies are aspirated, they often will lodge in the right mainstem bronchus. Aspiration pneumonia may result. If the endotracheal tube used for intubation is inserted too far, it usually lodges in the right mainstem bronchus. This allows ventilation of the right lung, but leaves the left lung useless