respiratory bronchiole
advertisement
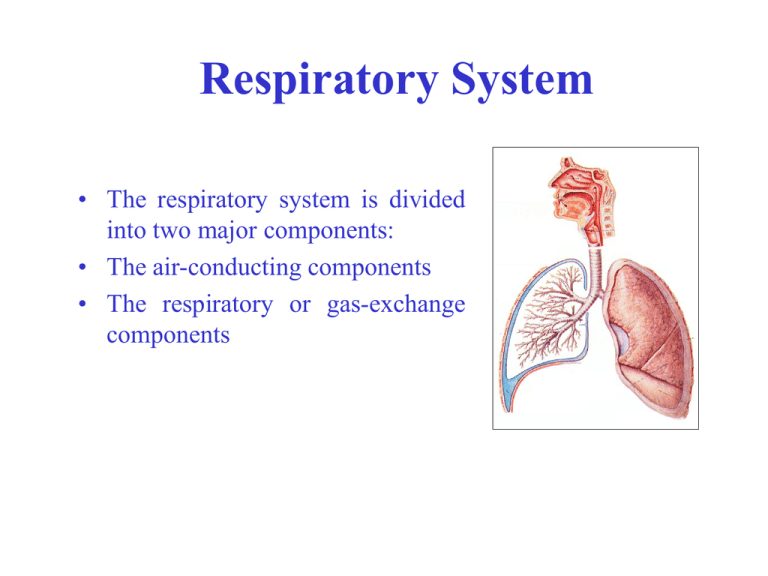
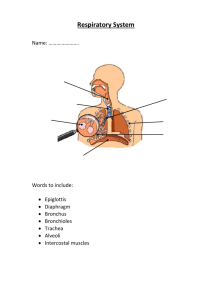
Respiratory System • The respiratory system is divided into two major components: • The air-conducting components • The respiratory or gas-exchange components Air Conducting Portion • Consists of the: – nasal cavities – Pharynx – Larynx – Trachea – Extrapulmonary bronchi – Intrapulmonary bronchi and bronchioles – Terminal bronchioles Three layers 1) Mucosa: ---epithelium: pseudostratified ciliated columnar epithelium ---lamina propria: CT, contain LC, PC, BV, LV Pseudostratified ciliated columnar epi. • ciliated cell: columnar, cilia • goblet cell • basal cell: -pyramidal, basally-located -undifferentiated cell→ciliated cell or goblet cell • brush cell: -columnar, microvilli, -EM: RER -function: not very clear • diffuse neuro-endocrine cell: -less, pyramidal -function: secret hormones to regulate contract of SM and secretion of gland Cilia on the surface of trachea Ciliated cell Goblet cell 2) Submucosa: LCT, with BV, LV and N • tracheal gland: mixed • diffuse LT and LN • S Ig A = secretory component (secreted by epi. cell) + Ig A ( produced by plasma cell) 3) Adventitia: • cartilage ring: 16-20 “C ” shaped • circular ligament: elastic F • SM- posterior part (membrane part): SM, elastic F, tracheal gland Air Conducting Portion functions: ----- Filters, moistens, and warms air before it enters lungs. -----Olfactory functions to examine air and to protect against breathing in harmful substances. -----Mucous tends to trap foreign substances and then the cilia (of pseudostratified ciliated columnar epithelium) clear the foreign substances from the trachea and bronchi of lungs. ----Cartilages found in trachea and bronchi play an important role in keeping airway open. Air Conducting Portion • • • • • • • Bronchial Tree – upside down tree with the trachea serving as the trunk of the tree and the bronchi as the primary branches Many smaller branches ending is small twigs (bronchioles) The leaves would represent the millions of alveoli. Extra-pulmonary bronchi are the left and right bronchi that branch off of the trachea and then enter the lungs. The intrapulmonary bronchi are the branches that form within the lungs. The larger sizes have hyaline cartilage which decreases with smaller bronchi. Eventually the cartilage is replaced with smooth muscle. Bronchioles have diameters of less than 5 mm. Terminal bronchioles have intact but greatly reduced amounts of smooth muscle in the wall. When this wall becomes incomplete, and contact with alveoli becomes evident, then the bronchiole changes to become a respiratory bronchiole. ① from lobar bronchi to small bronchi ---Regulation of simplification: (gradually) mucosa: -epi. : become thinner -goblet cell ↓ -lamina propria: thinner, SM ↑ • submucosa: gland ↓ • adventitia: cartilage→cartilage →decreasing ② bronchiole: D < 1mm ---continuous to change • goblet cell, Gland, cartilage ↓ or disappear • smooth muscle ↑,circular mucosa plica ↑ ③ terminal bronchiole: D < 0.5 mm ---goblet cell, gland, cartilage disappear ---SM: form a whole layer of circumferential SM ---Wall: • simple columnar epi.: two types of cells • A layer of SM Simple columnar epi: Clara cell i. ciliated cell ii. secreting cell: Clara cell EM: Ciliated cell • dome-shaped apical • SER • Secreting G: contains proteolytase and oxidase function: • dissolve the mucus, secrete surfactant. • • biological transformation undifferentiated cell → ciliated cell Respiratory Components • The respiratory components consist of: • Respiratory bronchioles • Alveolar ducts • Alveolar sacs • Alveoli Respiratory Components • Respiratory bronchioles have incomplete walls such that alveoli make direct contact. This allows for gas exchange to occur. • Alveolar ducts are where respiratory bronchioles branch. There is much greater space with alveoli exposed. • Alveolar sacs are clusters of alveoli . • Alveoli are single bubble like structures. ① respiratory bronchiole ---similar to terminal bronchioles: • simple ciliated columnar epi. • smooth muscle ---place where connect with alveoli: gradual changing • simple cuboidal epi. →simple squamous epi. • less SM, elastic F ② alveolar duct: 20-60 alveoli connect with it ---wall: hard to see- opening part between two alveoli • simple cuboidal epi. or squamous epi. • SM: single, EF- knob-liked structure ③ alveolar sac: ---many alveoli open to it ---no proper wall, no knob-liked structure ④ alveoli Respiratory Components • The lungs have an abundant blood supply. • Capillary beds are abundant within the spaces adjacent to the alveoli. • Alveoli walls consist of simple squamous epithelial cells which allow for rapid exchange of gases (diffusion). • The many millions of alveoli produce a very large surface area (1/2 of a tennis court) • Most abundant cells are the endothelial cells of the capillaries. These usually have small, elongated nuclei. ④alveoli: ---polygonal, with opening sac- 0.2mm in D, 300-400 million/per lung, total area: 70-80mm2 ---wall: • • epi. and basal lamina alveolar septum: CT with BV, EF a.alveolur epi: ---type I alveolar cell: LM: flattened, 0.2um, N: round EM: • plasmalemmal vesicles • tight junction Function: constitute the blood-air barrier ---type II alveolar cell: scattered, 5-8/per alveoles LM: • cuboidal or round, with round N • paler- stained, foamy cytoplasm EM: • secreting granules: Osmiophilic multilamellar body -0.1-1.0 um -contains: phospholipid, glycosaminoglycan and protein • microvilli, mito, lysosome, RER, Golgi Function: i. secreting surfactant ii. differentiated into type I alveolar cell neonatal respiratory distress syndrome b. alveolar septum: CT • EF • Fibroblast, macrophage, plasma cell, mast cell • LV, N • capillary: endothelium + basement membrane * Blood-air barrier: the structure through which the gaseous exchange takes place ---0.2-0.5 um ---components: • a layer of liquid • type I alveolar cell and basement M • CT • capillary endothelial cell and BM c. alveolar pore: 10-15 um ---equalize( balance) the air-pressure between alveoli ---lober pneumonia- bacteria or inflammatory spread through the pore d. alveolar marcophage: monocytes- MPS ---dust cell: macrophage which phagocytose carbon or duct particles ---heart failure cell: when lung congested(edema), the alveolar marcophage phagocytose RBC, digest the hemoglobin into hemosiderin(pigment) and accumulated them within macrophage Trachea Epithelium Hyaline cartilage Mucous acini Perichondrium Serous acini Adventitia fibrosa Pseudostratified Ciliated columnar Epithelium Blood vessel Hyaline cartilage cl = cilia, gc = goblet cell, bm = basement membrane Trachea – trachealis muscle between hyline cartilage Trachealis muscle Bronchus contains hyaline cartilage Cartilage Smooth muscle that Serves for bronchoconstriction Serous acini Intrapulmonary bronchus Bronchus with cartilage Pulmonary vein Intrapulmonary bronchus Intrapulmonary bronchus Intrapulmonary bronchus With cartilage Terminal bronchiole Terminal bronchiole Alveolar duct Respiratory bronchiole Pulmonary artery and vein bronchiole (no cartilage) Branching of bronchiole (no cartilage vissible) b=respiratory bronchiole with alveolus (a) in its wall, c and d = alveolar ducts which are lined almost entirely with alveoli, e= individual alveoli, f= blood vessel. a = two alveoli separated by thin interalveolar septa, b = smooth muscle in bronchiole, c= blood vessel d = bronchiole no cartilage Alveoli separated by the thin interalveolar septa. Reddish spots are RBC and dark spots are nuclei of simple epithelium of capillaries or alveoli.