Evaluation of FUO
advertisement
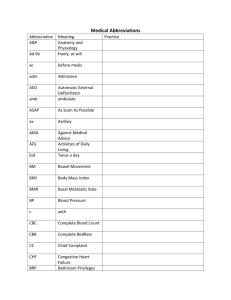
“Fever of Unknown Origin” (FUO) Courtney Hebert, MD Clinical Assistant Professor, Division of Infectious Diseases courtney.hebert@osumc.edu Learning Objectives Define and describe the term “Fever of Unknown Origin (FUO)” Recognize common infectious and non-infectious etiologies of FUO Describe the infectious and non-infectious work-up of patients diagnosed with FUO Describe the management of patients with FUO Defining the term “FUO” First formal definition (1961) 1. Temperatures greater than 38.3°C or 101°F on several occasions 2. Duration of fever greater than 3 weeks 3. Failure to reach diagnosis after 1 week in hospital Categories of FUO Hayakawa 2012 Categories of FUO Hayakawa 2012 Categories of FUO Hayakawa 2012 Categories of FUO Hayakawa 2012 Categories of FUO Hayakawa 2012 Classic FUO Etiologies fall into 5 general categories 1. 2. 3. 4. 5. Infection Malignancy Connective tissue Dz. Miscellaneous No diagnosis MACKOWIAK, PHILIP A.,DURACK, DAVID T. - Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases, 779-789 Classic FUO The Percentage of Patients with FUO by Cause Over the Past 40 years. Mourad, 2003 Arch Intern Med. 2003;163(5):545-551. doi:10.1001/archinte.163.5.545 Classic FUO Common infectious causes of FUO Unrecognized abscess (ex: abdominal, perinephric) Endocarditis – less common than in past HACEK organisms usually able to be cultured with modern techniques Difficult to culture organisms (ex: Bartonella, Aspergillus, Coxiella, Brucella) Tuberculosis Histoplasmosis Osteomyelitis Classic FUO Common connective tissue causes of FUO Adult Still’s disease Fever, rash, arthritis Rheumatoid Arthritis (RA) Systemic Lupus Erythematosus (SLE) Temporal Arteritis >50 years old, headache, symptoms of PMR, high ESR Polymyalgia Rheumatica (PMR) Classic FUO Common malignancies associated with FUO Lymphoma (most common cause) Leukemia Tumors metastatic to the liver Renal cell carcinoma Classic FUO Miscellaneous causes of FUO Factitious Fever (ex: Fraudulent vs. Self-induced) Drug fever (ex: Antibiotics, Antihistamines, NSAIDS) Familial fever syndromes Familial Mediterranean Fever TNF-receptor associated periodic syndrome Hyper- IgD syndrome. Hemophagocytic syndrome Inflammatory Bowel Disease (IBD) Pheochromocytoma Pulmonary embolism (PE) Thrombotic Thrombocytopenic Purpura (TTP) Thyroiditis Nosocomial FUO Patients who have a fever start after at least 24 hours of hospitalization Etiologies include: Drug fever Nosocomial infections Post operative complications Central fever (stroke) Immune Deficient FUO Patients with significantly impaired immune response often do not have traditional signs of inflammation This makes detection of infections more difficult Neutropenic FUO Neutropenia = < 500 PMNs (absolute) Decreased mucosal defense Febrile neutropenic patients receive empiric courses of broad spectrum antibiotics and often antifungal agents Neutropenic FUO Causes of Fever in Patients with Prolonged Neutropenia Who Are Receiving Broad Spectrum Antibiotics. Corey NEJM 2002 HIV Related FUO Incidence of FUO has decreased since the introduction of HAART Abellan-Martinez, 2009 HIV Related FUO Common causes of HIV-Related FUO: Mycobacterial disease Pneumocystosis (PCP) Cytomegalovirus (CMV) Histoplasmosis Lymphoma Drug fever Abellan-Martinez, 2009 Evaluation of FUO Comprehensive history Verify fevers and establish pattern Localizing symptoms? Workplace? Pets? Recent travel? History of connective tissue disease (CTD)? History of cancer/immunosuppression? Medications? Drug use? Familial fever syndromes? Evaluation of FUO Physical exam Temporal artery in elderly patient, sinus tenderness Evaluation of FUO Physical exam Listen for murmur, look for stigmata of endocarditis (Osler’s nodes, Janeway lesions, conjunctival hemorrhage) Evaluation of FUO Physical exam Lymphadenopathy, Thyromegaly Evaluation of FUO Physical exam Perirectal abscess in neutropenia Evaluation of FUO Physical exam Splenomegaly, Hepatomegaly Evaluation of FUO Physical exam Deep Vein Thrombosis (DVT) Evaluation of FUO Physical exam Skin, mucous membranes, teeth Evaluation of FUO Workup should be directed by patient’s symptoms and most likely diagnosis Most should get the following laboratory studies: Complete Blood Count (CBC) with Differential Serum chemistries Liver function tests Urinalysis (UA) Blood cultures HIV Antibody Chest X-Ray Selected serologies for infectious causes (based on exposure history) Disseminated granulomatous disease with abnormal CBC consider bone marrow biopsy (ex: Disseminated Histoplasmosis) Evaluation of FUO Imaging Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases, 1011-1034; http://m.australianprescriber.com/magazine/21/3/76/9/ Evaluation of FUO Imaging http://cancergrace.org/cancer-101/tag/pet-scans/; http://www.cmej.org.za/index.php/cmej/article/view/2796/3137 Evaluation of FUO Mourad, 2003 Management of FUO Withhold therapy until the cause is found Exceptions: Neutropenic Fever Corticosteroids in suspected Temporal Arteritis Unstable hospitalized patient Outcome of FUO A review of the literature from 1966 – 2000 showed a mortality rate of 12 – 35% for Classic FUO. Higher mortality If malignancy is identified Lower mortality If infection is identified If no cause is identified, 50 – 100% in these case series have a spontaneous recovery!!! Mourad, 2003 Summary of FUO The definition of classic FUO is temperature >101 °F for >3 weeks, and no diagnosis after 3 days in the hospital or 3 clinic visits. Definition differs for patients with neutropenia, HIV or suspected nosocomial onset. Causes of FUO are diverse, but can be categorized into infectious, malignancy, connective tissue disease and miscellaneous causes. Comprehensive history and physical exam are an important first step in FUO evaluation. Evaluation of FUO with laboratory test and imaging should be directed towards the most likely causes based on the history and physical. The key to management of FUO is to withhold specific treatment (but must note exceptions) until the cause is found. Thank you! Courtney Hebert, MD E-mail: courtney.hebert@osumc.edu References 1. Petersdorf RG, Beeson PB. Fever of unexplained origin: report on 100 cases. Medicine. 1961;40:1-30. 2. Durack DT, Street AC. Fever of unknown origin--reexamined and redefined. Current clinical topics in infectious diseases. 1991;11:35-51. 3. Mackowiak PA, Durack DT. Fever of Unknown Origin. In: Mandell GL, Douglas RG, Bennett JE, Dolin R, editors. Mandell, Douglas, and Bennett's principles and practice of infectious diseases. 6th ed. New York: Elsevier/Churchill Livingstone; 2005. p. 718-29. 4. Corey L, Boeckh M. Persistent fever in patients with neutropenia. The New England journal of medicine. 2002;346(4):222-4. 5. Abellan-Martinez J, Guerra-Vales JM, Fernandez-Cotarelo MJ, Gonzalez-Alegre MT. Evolution of the incidence and aetiology of fever of unknown origin (FUO), and survival in HIV-infected patients after HAART (Highly Active Antiretroviral Therapy). European journal of internal medicine. 2009;20(5):474-7. 6. Hayakawa K, Ramasamy B, Chandrasekar PH. Fever of unknown origin: an evidence-based review. The American journal of the medical sciences. 2012;344(4):307-16. Epub 2012/04/06. 7. Mourad O, Palda V, Detsky AS. A comprehensive evidence-based approach to fever of unknown origin. Archives of internal medicine. 2003;163(5):545-551. Survey We would appreciate your feedback on this module. Click on the button below to complete a brief survey. Your responses and comments will be shared with the module’s author, the LSI EdTech team, and LSI curriculum leaders. We will use your feedback to improve future versions of the module. The survey is both optional and anonymous and should take less than 5 minutes to complete. Survey