IMMUNOLOGICAL TOLERANCE
advertisement

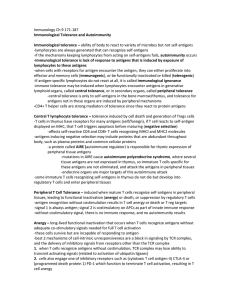
Chapter 15 Immunological tolerance is defined as unresponsiveness to an antigen that is induced by previous exposure to that antigen Antigens that induce tolerance are called tolerogens, or tolerogenic antigens, to distinguish them from immunogens, which generate immunity Tolerance to self antigens, also called self-tolerance, is a fundamental property of the normal immune system Immunological tolerance is important for several reasons: Normal individuals are tolerant of their own (self) antigens because the lymphocytes that recognize self antigens are killed or inactivated, or change their specificity Foreign antigens may be administered in ways that inhibit immune responses by inducing tolerance in specific lymphocytes Induction of immunological tolerance may be exploited as a therapeutic approach for preventing harmful immune responses Self-tolerance may be induced in immature self-reactive lymphocytes in the generative lymphoid organs (central tolerance) or in mature lymphocytes in peripheral sites (peripheral tolerance) Central tolerance occurs during the maturation of lymphocytes in the central (generative) lymphoid organs, where all developing lymphocytes pass through a stage at which encounter with antigen may lead to cell death or replacement of a self-reactive antigen receptor with a new one Peripheral tolerance occurs when, as a consequence of recognizing self antigens, mature lymphocytes become incapable of responding to that antigen, or are induced to die by apoptosis, or mature T cells are actively suppressed by regulatory T cells Foreign antigens in the absence of costimulatory signals may inhibit immune responses by inducing tolerance in specific lymphocytes The thymus also has an unusual mechanism for expressing protein antigens that are typically present only in certain peripheral tissues, so that immature T cells specific for these antigens can be deleted from the developing T cell repertoire. Some of these peripheral tissue antigens are expressed in thymic medullary epithelial cells under the control of the autoimmune regulator (AIRE) protein. Mutations in the AIRE gene are the cause of a multiorgan autoimmune disease called the autoimmune polyendocrine syndrome (APS). This group of diseases is characterized by antibody and lymphocyte-mediated injury to multiple endocrine organs, including the parathyroids, adrenals, and pancreatic islets Regulatory T cells produce IL-10 and TGF-β both of which inhibit immune responses Regulatory T cells inhibit the ability of APCs to stimulate T cells Inhibits the proliferation and effector functions of T cells and the activation of macrophages Regulates the differentiation of functionally distinct subsets of T cells Stimulates production of IgA antibodies by inducing B cells to switch to this isotype Promotes tissue repair after local immune and inflammatory reactions subside The biologic effects of IL-10 result from its ability to inhibit many of the functions of activated macrophages and dendritic cells Inhibits the production of IL-12 by activated dendritic cells and macrophages Inhibits the expression of costimulators and class II MHC molecules on dendritic cells and macrophages T lymphocytes that recognize self antigens without inflammation or that are repeatedly stimulated by antigens die by apoptosis The mitochondrial (or intrinsic) pathway is regulated by the Bcl-2 family of proteins antiapoptotic proteins (Bcl-2, Bcl-XL) proapoptotic effector proteins of the Bcl-2 family called Bim, Bax and Bak, In the death receptor (or extrinsic) pathway, cell surface receptors homologous to tumor necrosis factor (TNF) receptors are engaged by their ligands Repeated stimulation of T cells results in the coexpression of death receptors and their ligands, and engagement of the death receptors triggers apoptotic death. In CD4+ T cells, the most important death receptor is Fas (CD95), and its ligand is Fas ligand (FasL) Autoimmune lymphoproliferative syndrome (ALPS) B LYMPHOCYTE TOLERANCE