Skeletal System

The Reproductive System
Chapter 24
Reproductive System
Unlike other body systems which functions almost continuously the reproductive system is inactive until puberty
The primary sex organs or gonads are the testes in the male and the ovaries in the female
Reproductive System
The gonads produce sex cells, or gamates as well as secreting hormones
The remaining diversion organs of the reproductive system (ducts, glands and external genitalia) are referred to as accessory reproductive organs
Although male and female reproductive organs are quite different they have a common origin and a common purpose to produce offspring
Reproductive System
The male’s reproductive role is to manufacture males gametes called sperm and to deliver them to the female reproductive tract, where fertilization can occur
The mutually complimentary role of the female is to produce female gametes, called ova or eggs.
Reproductive System
When these events are properly timed, a sperm and an egg fuse to form a fertilized egg, the first cell of the new individual, from which all body cells will arise
The male and female reproductive systems are equal partners in events leading up to fertilization
Once fertilization has occurred, the female uterus provides a protective environment for the embryo until birth
Reproductive System
The sex hormones - androgens in males and estrogens and progesterone in females play vital roles in both the development and function of the reproductive organs and in sexual behavior and drives
These hormones also influence the growth and development of many other organs and tissues of the body
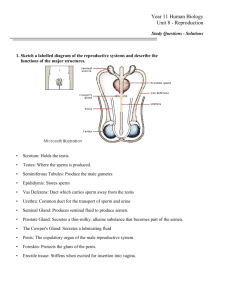
Male Reproductive System
The image which follows represents an overview of the male reproductive system
Male Reproductive System
Male Reproductive system
The sperm-producing testes, or male gonads, lie within the scrotum
From the testes the sperm are delivered to the body exterior through a system of ducts in the following order;
– Epididymis
– Ductus deferens
– Urethra
Male Reproductive System
Male Reproductive System
The accessory sex glands, which empty their secretions into the ducts during ejaculation are
– Seminal vesicles
– Prostrate gland
– Bulbourethral glands
Male Reproductive System
The Scrotum
The scrotum is a sac of skin and superficial fascia that hangs outside of the abdominopelvic cavity at the root of the penis
The Scrotum
The Scrotum
Covered with sparse hairs, the scrotal skin is more heavily pigmented than that elsewhere on the body
The Scrotum
The paired testes, or testicles, lie suspended in the scrotum
A midline septum divides the scrotum into right and left halves, one compartment for each testis
The Scrotum
The location of a man’s testes appears to make them vulnerable to injury
However, viable sperm cannot be produced at core body temperature (36.2 C)
The superficial location of the scrotum provides a temperature which is about 3 degrees cooler
Scrotum
The scrotum also responds to temperature changes
When it is cold, the testes are draw closer to the warmth of the body and the scrotum becomes shorter and heavily wrinkled to reduce heat loss
When it is warm, the scrotal skin is flaccid and loose to increase cooling, and the testes hang lower
The Scrotum
These changes maintain a fairly constant temperature and reflect the activity of the two sets of muscles
– Dartos
– Cremaster
The Testes
Each testes is approximately 4 cm long and 2.5 cm in diameter
It is surrounded by two tunics
– Tunica vaginalis
– Tunica albuginea
The Testes
The outer tunic is the two layered tunica vaginalis which is derived from the peritoneum
Deep to this is the tunica albuginea, the fibrous capsule of the testis
The Testes
Septa extending from the tunica albuginia divide the testis into 250 - 300 wedge shaped compartments or lobules
Each lobule contains
1-4 semiinferous tubules
The Testes
The seminiferous tubules produce the sperm
The seminiferous tubules of each lobule converge to form a tubulus rectus
The Testes
The tubulus rectus is a straight tubule that conveys sperm into the rete testis
The rete testis is a tubular network from which the sperm leave via the efferent ductules
The Testes
Sperm leaving the efferent ductules enter the epididymis which is located on the external surface of the testis
The Testes
Lying in the soft connective tissue surrounding the seminiferous tubules are the interstitual cells or
Leydig cells
The Testes
Interstitial cells produce androgens (most importantly testosterone), which is secreted into the surrounding interstitual fluid
It is significant that the sperm producing and hormone producing functions of the testis are carried out by completely different cell populations
The Testes
The long testicular arteries, which branch from the abdominal aorta, supply the testes
The Scrotum
The testicular veins draining the testes arise from a vinelike network called the pampiniform plexus that surrounds the testicular artery
The Scrotum
The plexus absorbs heat from the arterial blood, cooling it before it enters the testes
Thus, it provides an additional avenue for maintaining the testes at their cool homeostatic temperature
The Testes
The testes are served by both divisions of the autonomic nervous system
Associate sensory nerves transmit impulses
Nerve fibers are enclosed in the spermatic cord
Homeostatic Imbalance
Although testicular cancer is relatively rare (1 in 20,000) it is the most common cancer in young men (15-35)
A history of mumps or orchitis
(inflammation) increases the risk
The most important risk factor is cryptochidism (non-descent of the testes)
The most common sign is a painless solid mass in the testes (self-exam)
The Penis
The penis is a copulatory organ designed to deliver sperm into the female reproductive tract
The Penis
The penis and the scrotum which hang from the peritoneum make up the external reproductive structures or genitalia
The Penis
The male perineum is a diamond shaped region located between the public symphysis anteriorly, the coccyx posteriorly, and the ishial tuberosities laterally
The Penis
The floor of the perineum is formed by muscles;
– Ishiocavernous
– Bulbosponginous
– Superficial transverse perineus
The Penis
The penis consists of an attached root and a free shaft or body that ends in an enlarged tip, the glans penis
The skin of the penis is loose, and it slides distally to form a cuff of skin called the prepuce or foreskin around the glans
The Penis
Internally, the penis contains the spongy urethra and three long cylindrical bodies (corpora) of erectile tissue
Erectile tissue is a spongy network of connective tissue and smooth muscle riddled with vascular spaces
The Penis
During sexual excitement, vasular spaces fill with blood causing the penis to enlarge an become rigid
This event, called an erection, enables the penis to serve as a penetrating organ
The Penis
The midventral erectile body, the corpus spongiosum, surrounds the urethra
It expands distally to form the glans and proximally to form the part of the root called the bulb of the penis
The Penis
The bulb is covered externally by the sheetlike bulbospingiosus muscle and is secured to the urogential diaphragm
The Penis
The paired dorsal erectile bodies called the corpora cavernosa make up most of the penis and are bound by fibrous tunica albuginea
Their proximal ends from the crura of the penis and each is surrounded by the ischiocavernosus
Each crus is surrounded by an ischiocavernosus muscle and anchors to the pubic arch of the bony pelvis
The Penis
The Male Duct System
Sperm travel from the testes to the outside of the body through a system of ducts
The accessory ducts are…
– Epididymis
– The ductus deferens
– Urethra
The Male Duct System
The comma-shaped epididymis is about
3.8 cm long
Its head, which joins the efferent ductiles, caps the superior aspect of the testis
Its body and tail regions lie on the posteriolateral aspects of the testis
The Male Duct System
The bulk of the epididymis consists of the highly coiled duct of the epididymis with an uncoiled length of about 6 meters
The Male Duct System
Within the duct of the epididymis some of the cells of pseudostratified epithelium mucosa exhibit long, nonmotile microvilli which absorb excess testicular fluid and pass nutrients to the sperm in the lumen
The Epididymis
The immature, nearly nonmotile sperm that leave the testis are moved slowly through the duct of the epidymis
As the sperm move along the twisting course, a trip of 20 days, the sperm gain the ability to swim
The Epididymis
When a male is sexually stimulated and ejaculates, the smooth muscle in the walls of the epididymis contracts, expelling sperm from its tail section into the next segment of the duct system the ductus deferens
Sperm can stay in the epididymis for several months
If held longer, they are eventually phagocytized by epithelial cells of the epididymis
The Ductus Deferens
The ductus deferens or vas deferens is about
45 cm (18 in) long
It runs upward as part of the spermatic cord from the epididymis through the inguinal canal into the pelvic
The Ductus Deferens
It is easily palpated as it passes anterior to the pubic bone
It then loops medially over the ureter and descends along the posterior wall of the bladder
The Ductus Deferens
Its terminus expands to form the ampulla and then joins with the duct of the seminal vesicle (a gland) to form the short ejaculatory duct
Seminal vesicle
Ejaculatory duct
The Ductus Deferens
Each ejaculatory duct passes into the prostate gland where it empties into the urethra
Prostate Gland
Ejaculatory duct
The Ductus Deferens
The ductus deferens propels live sperm from their storage sites, the epididymis and distal part of the ductus deferens, into the urethra
At the moment of ejaculation, the thick layers of smooth muscle in its walls create strong peristaltic waves that rapidly squeeze the sperm forward
The Ductus Deferens
Part of the ductus deferens lies within the scrotal sac
In a vasectomy the physician makes a small incision into the scrotom, cuts and then ties the ductus deferens
The Urethra
The urethra is the terminal portion of the male duct system
It conveys both urine and semen so it serves both the urinary and reproductive systems
The Urethra
The three regions of urethra are
– Prostatic urethra
– Menbranous urethra
– Spongy urethra
The Urethra
The prostatic urethra is surrounded by the prostate gland
The membranous urethra is in the urogenital diaphragm
The spongy urethra runs through the penis and opens outside at the external urethral oriface
The spongy urethra is about 15 cm (6 in) long and accounts for 75% of the length of the urethra
Accessory Glands
The accessory glands include;
– Seminal vesicles (paired)
– Bulbourethral glands (paired)
– Prostrate gland (singular)
These glands produce most of the volume the semen
– Sperm
– Accessory gland secretions
The Seminal Vesicles
The seminal vesicles lie on the posterior wall of the bladder
These glands are about 5-7 cm in length, roughly the size and shape of a little finger
Seminal Vesicles
The Seminal Vesicles
The secretion of the vesicles accounts for about 60% of the volumn of the semen
It is a yellowish, viscous, alkaline fluid containing fructose sugar, ascorbic acid, a coagulating enzyme and prostaglandins
The Seminal Vesicles
The duct of each seminal vesicle joins the ductus deferens on that side to form the ejaculatory duct
Sperm and seminal fluid mix in the ejaculatory duct to enter the prostatic urethra together during ejaculation
The Prostate
The prostate gland is a single doughnut shaped gland about the size of a chestnut
It encircles the part of the urethra just inferior to the bladder
Prostate Gland
The Prostate Gland
Enclosed by a thick connective tissue capsule, it is made up of 20 to 30 compound tubular-alveolar glands
The glands are embedded in a mass of smooth muscle and dense connective tissue
The Prostate Gland
The prostatic gland secretion accounts for one third of the semen volume is a milky, slightly acid fluid
It contains
– Citrate (a nutrient source)
– Enzymes
• Fibrinolysin
• Hyaluronidase
– Acid prostrate specific antigen (activates sperm)
The Prostate Gland
Prostrate gland secretions enter the prostatic urethra via several ducts when prostatic smooth muscle contract during ejaculation
The Prostate Gland
Hypertrophy of the prostate gland affects nearly every elderly male, distorting the urethra
The prostatic mass blocks the urethra making urination difficult
This condition also enhances the risk of bladder infections and kidney damage
There are a variety of treatments, and it is recommended to consult with your physician regarding the best course of action for you
Semen
Semen is a milky white, mixture of sperm and accessory gland secretions
The liquid provides a transport medium, nutrients, and contains chemicals that protect and activate the sperm and facilitate their movement
Sperm
Mature sperm cells are streamlined cells containing very little cytoplasm or stored nutrients
The fructose in seminal vesicle secretion provides nearly all their energy
Sperm
The protoglandins in seman decrease the viscosity of mucus guarding the entry point of the uterus (cervix) and stimulate reverse peristalsis in the uterus and the medial parts of the uterine tubes
These changes facilitate the movement of sperm through the female reproductive tract
Sperm
The presence of the hormone relaxin and certain enzymes in semen enhance sperm motility
The relative alkalinity of semen as a whole
(pH 7.2-7.6) due to bases (spermine and others) helps neutralize the acid environment of the male’s urethra and the female’s vagina
This also helps protect the sperm and enhance their motility
Sperm
Sperm also contains an antiboitic chemical called seminalplasmin, which destroys certain bacteria
Clotting factors (fibrinogen and others) found in semen coagulate it just after it is ejaculated
Upon ejaculation the fibrinogen liquefies the sticky mass, enabling the sperm to swim out and begin their journey through the female duct system
Sperm
The amount of semen propelled out the the male duct system during ejaculation is relatively small (2-5 ml) but there are between 50 and 130 million sperm per milliliter
Physiology: Male System
The chief phases of the male sexual response are
– Erection of the penis; which allow entry into the female vagina
– Ejaculation; which expels semen into the vagina
Erection
Erection, enlargement and stiffening of the penis results from engorgement of the erectile bodies with blood
When a man is not aroused, the arterioles supplying the erectile tissue is constricted and the penis is flaccid
Erection
However, during sexual excitement a parasympathetic reflex is triggered that promotes release of nitric oxide (NO) locally
NO relaxes vascular smooth muscle, causing these arterioles to dilate, which allows the erectile bodies to fill with blood
Erection
Expansion of the corpora cavernosa of the penis compresses their drainage veins, retarding blood outflow and maintaining engorgement
The corpus spongiosum expands but not nearly as much as the cavernosa; its main job is to keep the urethra open during ejaculation
Erection
Erection of the penis is one of the rare examples of parasympathetic control of arterioles
Another parasympathetic effect is stimulation of the bulbourethral glands, which causes lubrication of the glans penis
Erection
Erection is initiated by a variety of sexual stimuli, such as touching of the genital skin, mechanical stimulation of the pressure receptors in the penis and erotic sights, sounds, and smells
The CNS responds to such stimuli by activating parasympathetic neurons that innervate the internal pudendal arteries serving the penis
Erection
Sometimes erection is induced solely by emotional or higher mental activity (the thought of a sexual encounter
Emotions and thoughts can also inhibit erection, causing vasoconstriction and resumption of the flaccid penile state
Impotence, is the inability to attain and maintain erection
Ejaculation
Ejaculation is the propulsion of semen from the male duct system
While erection is under parasympathetic control, ejaculation is under sympathetic control
When impulses provoking erection reach certain critical level, a spinal reflex is initiated, and a massive discharge of nerve impulses occurs over the sympathetic nerves serving the genital organs (L
1
& L
2
)
Ejaculation
During ejaculation
– The reproductive ducts and accessory organs contract, emptying their contents into the urethra
– The bladder sphincter muscle constricts, preventing the expulsion of urine or reflux of semen into the bladder
– The bulbospongiosus muscles of the penis undergo a rapid series of contractions, propelling semen at a speed of 200 inches/sec from the urethra
Ejaculation
The rhythmic muscle contractions are accompanied by intense pleasure and many systemic changes such as generalized muscle contraction, rapid heartbeat, and elevated blood pressure
The entire ejaculatory event is referred to as a climax or orgasm
Ejaculation
Organism is quickly followed by muscular and psychological relaxation and vasoconstriction of the penile arterioles, which allow the penis to become flaccid again
After ejaculation, there is a latent period, ranging in minutes to hours, during which a man is unable to achieve another organism
The latent period length increases with age
Spermatogenesis
Spermatogenesis is the sequence of events in the seminiferous tubules of the testes that produce male gametes or sperm or spermatozoa
The process begins in puberty, around the age of 14 years in males, and continues throughout life
Every day, a healthy adult male makes about 400 million sperm
Ample supply of sperm for reproduction
Spermatogenesis
Having two sets of chromosomes, one from each parent, is a key factor in the human life cycle
Spermatogenesis
The normal chromosome number in most body cells is referred to as the diploid or 2 n chromosomal number of the organism
Spermatogenesis
In humans, the diploid number is
46, and such diploid cells contain 23 pairs of similar chromosomes called homologous or chromosomes or homologues
Spermatogenesis
One member of each pair is from the male parent
(paternal chromosome); the other is from the female parent
(maternal chromosome)
Spermatogenesis
Generally speaking, the two homologues of each chromosome pair look alike and carry genes that code the same traits
However, the expression of those traits may differ in each parent
Spermatogenesis
The number of chromosomes present in human gametes is 23, referred to as the haploid or n chromosomal number
Spermatogenesis
Gametes contain only one member of each homologous pair
When sperm and egg fuse, they form a fertilized egg that reestablishes the typical diploid chromosomal number of human cells
Spermatogenesis
Gamete formation in both sexes involves meiosis, a unique kind of nuclear division, that for the most part, occurs only within the gonads
Mitosis or cell division distributes replicated chromosomes equally between the two daughter cells
Consequently, each daughter cell receives a set of chromosomes identical to that of the mother cell
Spermatogenesis
Meiosis consists of two consecutive nuclear divisions, and its product is four daughter cells instead of two, each with half as many chromosomes as typical body cells
Meiosis provides the means for reducing the chromosome number by half in gametes
Mitosis and meiosis are compared on the next slide…
Spermatogenesis
Meiosis
The two nuclear divisions of meiosis, called meiosis I and meiosis II are divided into phases for convenience
Although these phases are given the same names as those of mitosis (prophase, metaphase, anaphase and telophase) events of meiosis I are quire different from those of mitosis
Meiosis
In meiosis, as in mitosis, the chromosomes replicate before meiosis begins (Interphase)
But in the prophase of meiosis I the replicated chromosomes seek out their homologous partners and pair up with them along their entire length
Meiosis
Meiosis
The alignment of the homologues takes place at discrete spots along the length of the homologues - like a buttoning
As a result of this process, called synapsis, little groups of four chromatids called tetrads, or bivalents, are formed
Meiosis
Meiosis
During synapsis, a second unique event called crossover occurs
Crossovers are formed within each tetrad as the free ends of one maternal and one paternal chromatid wrap around each other at one or more points
Crossover allows an exchange of genetic material between the paired maternal and paternal chromosomes
Meiosis
Meiosis
During metaphase I, the tetrads line up at the spindle equator
This alignment is random; that is, either the paternal or maternal chromosome can be on a given side of the equator
Meiosis
Meiosis
During anaphase I, the sister chromatids representing each homologue behave as a unit - almost if replication had not occurred - and the homologous chromosomes (each still composed of two joined sister chromatids) are distributed to opposite ends of the cell
Meiosis
Meiosis
Thus, when meiosis I is completed, the following conditions exist: Each daughter cell has
– Two copies of one member of each homologous pair (either the paternal or maternal) and none of the other, and
– A diploid amount of DNA but a haploid chromosome number because the still-united sister chromatids are considered to be a single chromosome
Meiosis
Meiosis II
The second meiotic division, meiosis II, mirrors mitosis in every way, except that the chromosomes are not replicated before it begins
Instead, the chromatids present in the two daughter cells of meiosis I are simply parceled out among four cells
Because the chromatids are distributed to the daughter cells, meiosis II is sometimes referred to as equational division meiosis
Meiosis II
Meiosis accomplishes two important tasks
– It reduces the chromosomal number by half
– It introduces genetic variability
Meiosis II
The random orientation of the homologous pairs during meiosis I produces tremendous variability in the resulting gametes by scrambling genetic characteristics derived from the two parents in different combinations
Variability is further increased by crossover because during late prophase I, the homologues break at points of crossover and exchange chromosomal segments
Meiosis II
The net result is that it likely that no two gametes are exactly alike, and all are different from the original mother cells
Spermatogenesis
A histological section of an adult testes shows that most of the cells making up the epithelial walls of the seminiferous tubules are in various stages of cell division
Spermatogenesis
Spermatogenesis
These cells, collectively called spermatogenic cells, give rise to sperm in a series of cellular divisions and transformations
Mitosis of Spermatogonia
The outermost and least differentiated tubule cells, which are in direct contact with the epithelial lamina, are stem cells called spermatogonia
The spematogonia divide more or less continuously by mitosis and, until puberty, all their daughter cells become spermatogonia
Mitosis of Spermatogonia
Spermatogenesis begins during puberty, and from then on, each mitotic division of a spermatogonium results in two distinctive daughter cells - types A and B
The type A daughter cell remains at the basement membrane to maintain the germ cell line
The type B cell gets pushed toward the lumen, where it becomes a primary spermatocyte and becomes four sperm
Mitosis of Spermatogonia
Meiosis: Spermatocytes
Still early in spermatogenesis, each primary spermatocyte generated during the first phase undergoes meiosis I, forming two smaller haploid cells called secondary spermatocytes
The secondary spermatocytes continue on rapidly into meiosis II, and their daughter cells, called spermatids, are small round cells with large spherical nuclei seen closer to the lumen of the tubule
Spermatogenesis
Spermiogenesis: Spermatids
As late spermatogenesis begin, each spermatid has the correct chromosomal number for fertilization ( n ), but it is non motile
It must undergo a streamlining process called spermiogenesis, during which it sheds its excessive cytoplasmic baggage and forms a tail
Spermatogenesis
1. Activity of the Golgi apparatus to package acrosmal enzymes
Spermatogenesis
2. Positioning of the acrosome at the anterior end of the nucleus and the centrioles at the opposite end of the nucleus
Spermatogenesis
3. Elaboration of microtubules to form the flagellum of the tail
Spermatogenesis
4. Mitochondrial multiplication and their positioning around the proximal portion of the flagellum
Spermatogenesis
5. Sloughing off excess cytoplasm
Spermatogenesis
6. Structure of an immature sperm that has just been released from a sustentacular cell
Spermatogenesis
7. Structure of a fully mature sperm
Spermatogenesis
The resulting sperm, or spermatozoon, has three major regions
– Head
– Midpiece
– Tail
Spermatogenesis
The three regions correspond to
– Genetic
– Metabolic
– Locomotor
Spermatogenesis
The head of the sperm consists almost entirely of its flattened nucleus, which contains compacted DNA
Adhering to the top of the nucleus is a helmet like acrosome
The lysosome like acrosome is produced by the Golgi apparatus and contains hydrolytic enzymes (hyaluronidase and others) that enable the sperm to penetrate and enter the egg
Spermatogenesis
The sperm midpiece contains mitrochondria spiraled tightly around the contractile filaments of the tail
The tail is a typical flagellum produced by a centriole
The mitrochondria provide the metabolic energy (ATP) needed for the whiplike movements of the tail that propel the sperm along its way in the female reproductive tract
Role of Sustentacular Cells
Throughout spermatogenesis, descenants of the same spermatogonium remain closely attached to one another by cytoplasmic bridges
Role of Sustentacular Cells
The cells are surrounded by and connected to supporting cells, called sustentacular cells or Sertoli cells, which extend from the basal lamina to the lumen of the tubule
Role of Sustentacular Cells
The sustentacular cells, bound to each other by tight junctions, form an unbroken layer within the seminiferous tubule dividing it into two compartments
Role of Sustentacular Cells
The basal compartment extends from the basal lamina to their tight junctions and contains spermatogonia and the earliest primary spermatocytes
Role of Sustentacular Cells
The adluminal compartment lies internal to the tight junctions and includes the meitoically active cells and the tubule lumen
Role of Sustentacular Cells
The tight junctions between the sustentacular cells from the blood-testis barrier
This barrier prevents the membrane antigens of differentiating sperm from escaping through the basal lamina into the bloodstream
Role of Sustentacular Cells
Because sperm are not formed until puberty, they were absent when the immune system is being programmed to recognize one’s own tissues early in life
The spermatogonia, which are recognized as “self” are outside the barrier and can be influenced by bloodborne chemical messengers that prompt spermatogenesis
Role of Sustentacular Cells
Following mitosis of the spermatogonia, the tight junctions of the sustentacular cells open to allow primary spermatocytes to pass into the adluminal compartment
Role of Sustentacular Cells
In the adluminal compartment spermatocytes and spermatids are nearly enclosed in recesses in the sustentacular cells spermatocytes spermatids
Role of Sustentacular Cells
Sustentacular cells deliver nutrients to the dividing cells, move them along to the lumen, and secrete testicular fluid that provides the transport medium for sperm in the lumen spermatocytes spermatids
Role of Sustentacular Cells
In addition, sustentacular cells dispose of excess cytoplasm sloughed off the spermatids as they transform into sperm
The sustentacular cells also produce mediators that help regulate spermatogenesis
Role of Sustentacular Cells
During spermatogenesis the time from the formation of a primary spermatocyte to release of immature sperm into the lumen takes approximately 64 to 72 days
Sperm in the lumen are unable to “swim” and are incapable of fertilizing an egg
Role of Sustentacular Cells
Sperm are pushed by pressure of the testicular fluid through the tubular system of the testes into the epididymis
Within the epididymis sperm mature further gaining increased motility and fertilizing power
Hormonal Regulation: Male
Hormonal regulation of spermatogenesis and testicular androgen production involves interactions between the hypothalamus, anterior pituitary gland, and testes
This relationship is called the brain testicular axis
Hormonal Regulation: Male
1) The hypothalamus releases gonadotropin releasing hormone
(GrRH), which controls the release of anterior pituitary gonadotropins, follicle stimulating hormone (FSH) and luteinizing hormone
(LH)
Hormonal Regulation: Male
2) Binding of GnRH to pituitary cells
(gonadotrophs) prompts them to secrete FSH and
LH into the blood
Hormonal Regulation: Male
3) FSH stimulates spermatogenesis indirectly by stimulating the sustentacular cells to release androgen binding protein (ABP)
Hormonal Regulation: Male
3 (con’t) ABP prompts the spermatogenic cells to bind and concentrate testosterone which in turn stimulates spermatogenesis
Thus, FSH makes the cells receptive to testosterone’s effects
Hormonal Regulation: Male
4) LH binds to the interstitial cells and stimulates them to secrete testosterone and a small amount of estrogen
LH is sometimes referred to as interstitial cellstimulating hormone
(ICSH) in males
Hormonal Regulation: Male
4) (con’t) Locally testosterone serves as the final trigger for spermatogenesis
Testosterone entering the bloodstream exerts a number of effects at other body sites
Hormonal Regulation: Male
5) Both the hypothalamus and the anterior pituitary are subject to feedback inhibition by bloodborne hormones
Testosterone inhibits hypothalamic release of
GnRH and acts directly on the anterior pituitary to inhibit gonadotropin release
Hormonal Regulation: Male
5) (con’t) Inhibin a protein hormone released by the sustentacular cells, serves as a barometer of the normalcy of spermatogenesis
Hormonal Regulation: Male
5) (con’t) When the sperm court is high, inhibin release increases and it inhibits anterior pituitary release of FSH and GnRH release by the hypothalamus
When sperm court falls below 20 million/ml, inhibin secretion declines steeply
Hormonal Regulation: Male
The amount of testosterone and sperm produced by the testes reflects a balance among three sets of hormones
– GnRH, which indirectly stimulates the testes via its effect on FSH and LH (ICSH) release
– Gonadotropins, which directly stimulate the testes
– Testicular homones (Testosterone and inhibin), which exert negative feedback controls on the hypothalamus and anterior pituitary
Hormonal Regulation: Male
Since the hypothalamus is also influenced by input from other brain areas, the whole axis is under CNS control
In the absence of GnRH and gonadotropins, the testes atrophy, and for all practical purposes, sperm and testosterone production ceases
Hormonal Regulation: Male
Development of male reproductive structures depends on prental secretion of male hormones, and for a few months after birth, a male infant has plasma gonadotropin and testosterone levels nearly equal to those of a midpubertal boy
Soon thereafter, blood levels of these hormones recede and they remain low throughout childhood
Hormonal Regulation: Male
As puberty nears, much higher levels of testosterone are required to suppress hypothalamic release of GnRH
As more GnRH is released more testosterone is secreted by the testes, but the threshold for hypothalamic inhibition keeps rising until the adult pattern of hormone interaction is achieved
Hormonal Regulation: Male
Maturation of the brain-testicular axis takes about three years, and once established, the balance between the interacting hormones remains relatively constant
Consequently, an adult male’s sperm and testosterone production remain fairly stable as opposed to females where there are normal cyclic swings of gonadotropin and female sex hormones
Effects of Testosterone Activity
Testosterone, like all steroid hormones, is synthesized from cholesterol
Its exerts its effects by activating specific genes to transcribe messenger RNA molecules, which results in enhanced synthesis of certain proteins in the target cells
Effects of Testosterone Activity
In some target cells, testosterone must be transformed into another steroid to exert its effects
In the prostrate gland, for example, testosterone must be converted to dihydrotestosterone (DHT) before it can bind with nucleus
Effects of Testosterone Activity
In certain neurons of the brain, testosterone is converted to estrogen to bring about its stimulatory effects
Thus, in this case, a “male” hormone is transformed into a “female” hormone to exert its masculinizing effects
Effects of Testosterone Activity
As puberty ensues, testosterone not only prompts spermatogenesis but has multiple anabolic effects throughout the body
It targets all accessory reproductive organs (ducts, glands, penis) causing them to grow and assume adult size and function
Effects of Testosterone Activity
In adult males, normal plasma levels of testosterone maintain these organs
When testosterone is deficient or absent, all accessory organs atrophy, semen volume declines markedly, and erections and ejaculation are impaired
In this circumstance a male would become sterile and impotent
This situation would be remedied by testosterone replacement therapy
Effects of Testosterone Activity
Male secondary sex characteristics induced in nonreproductive organs by the male sex hormones (mainly testosterone) make their appearance at puberty
These induced changes include the appearance of pubic, axillary, and facial hair, enhanced hair growth on the chest and other body areas, deepening of th voice as the larynx enlarges
Effects of Testosterone Activity
The skin thickens and becomes oiler
(which predisposes men to acne), bones grow and increase in density, and skeletal muscles increase in size and mass
The last two effects are often referred to as the somatic effects of testosterone
(some = body)
Effects of Testosterone Activity
Testosterone also boosts basal metabolic rate and influences behavior
It is the basis of the sex drive (libido) in both males and females
Although testosterone is called a “male” hormone, it should be specifically tagged as a promoter of male sexual activity
In embryos, the presence of testosterone masculinizes the brain
Effects of Testosterone Activity
The testes are not the only source of androgens; the adrenal glands of both sexes also release androgens
However, the relatively small amounts of adrenal androgens are unable to support normal testosterone-mediated functions when the testes fail to produce androgens
We can assume that it is the testosterone production by the testes that supports male reproductive function
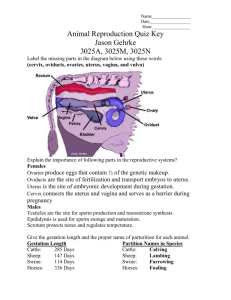
Female Reproductive System
The image which follows represents an overview of the female reproductive system
Female Reproductive System
Female Reproductive System
The reproductive role of the female is far more complex than that of a male
She must produce gametes, but her body must prepare to nurture a developing embryo for a period of approximately nine months
Female Reproductive System
Ovaries, the female gonads, are the primary reproductive organs of the female
Like the testes of the male, ovaries serve a dual purpose
– Produce gametes
– Produce female sex hormones (estogen and progesterone)
The accessory ducts (uterine tubes, uterus, and vagina) transport or otherwise serve the needs of the reproductive cells and fetus
Female Reproductive System
The ovaries and duct system, collectively known as the internal genitalia are mostly located in the pelvic cavity
The female’s accessory ducts, from the vicinity of the ovary to the body exterior, are the uterine tubes, uterus and vagina
The external sex organs of the females are referred to as the external genitalia
The Ovaries
The paired ovaries which flank the uterus on each side are shaped like almonds and are about twice as large
The Ovaries
Each ovary is held in place within the peritoneal cavity by several ligaments
The Ovaries
The ovarian ligament anchors the ovary medially to the uterus
The Ovaries
The suspensory ligament anchors the ovaries laterally to the pelvic wall
The Ovaries
The mesovarium ligaments suspends the ovaries between the fallopian tubes and the uterus
The Ovaries
Both the suspensory ligament and the mesovarium are part of the broad ligament
The Ovaries
The broad ligament is a peritoneal fold that “tents” over the uterus and supports the uterine tubes, uterus and vagina
The Ovaries
The ovaries are served by the ovarian arteries which are branches of the abdominal aorta
The Ovaries
The ovarian blood vessels reach the ovaries by traveling through the suspensory ligaments and mesovaria
The Ovaries
The ovaries are surrounded externally by a fibrous tunica albuginea
The Ovaries
The tunica albuginea is in turn covered by a layer of cuboidal epithelium called the germinal epithelium of the mesovarium
The Ovaries
The term germinal epithelium is a misnomer because this layer does not give rise to ova
The Ovaries
The ovary has an outer cortex, which houses the forming gametes, and an inner medullary region containing large blood vessels and nerves
The Ovaries
Embedded in the highly vascular connective tissue of the ovary cortex are many tiny sac like structures called ovarian follicles
The Ovaries
Each follicle consists of an immature egg, called an oocyte encased in one or more layers of very different cells
The Ovaries
The surrounding cells are called follicle cells if a single layer is present
The Ovaries
If more than one layer is present, the cells are called granulosa cells
The Ovaries
Follicles at different stages of maturation are distinguished by their structure
A primordinal follicle, has one layer of squamous like follicle cells surrounding the oocyte
A primary follicle having two or more layers of cuboidal or columnar type granulosa cells enclosing the oocyte
The Ovaries
In a secondary follicle the fluid filled spaces appearing between the granulosa cells coalesce to form a fluid filled cavity called an antrum
The Ovaries
At its most mature stage, when it is called a vesicular or Graafian follicle, the follicle bulges from the surface of the ovary
The Ovaries
The oocyte of the vesicular follicle sits on a stalk of granulosa cells at one side of the antrum
The Ovaries
Each month in adult women, one of the ripening follicles ejects its oocyte from the ovary, an event ovulation
The Ovaries
After ovulation, the ruptured follicle is transformed into a structure called the corpus luteum which eventually degenerates
The Ovaries
As a rule, most of these structures can be seen within the same ovary
In older women, the surfaces of the ovaries are scarred and pitted, revealing that many oocytes have been released
Female Duct System
The uterine tubes or fallopian tubes and oviducts form the initial part of the female duct system
Female Duct System
They receive the ovulated oocyte and provide a safe site where fertilization can occur
Female Duct System
Each uterine tube is about 10 cm (4 in) long and extends medially from the ovary to a constricted region called the isthmus
Female Duct System
The distal end of each uterine tube extends as it curves around the ovary, forming the ampulla, which is where fertilization occurs
Female Duct System
The ampulla ends in the infundibulum, an open, structure bearing ciliated projections called fimbriae that drape over the ovary
Female Duct System
Unlike the male duct system, which is continuous with the tubules of the testes, the uterine tubules have little or no actual contact with the ovaries
Female Duct System
An ovulated oocyte is cast into the peritoneal cavity, and many oocytes are lost there
Female Duct System
The uterine tube performs a complex sequence of movements to capture oocytes
Female Duct System
The infundibulum bends to drape of the ovary while the fimbriae stiffen and sweep the ovarian surface
Female Duct System
The beating cilia on the fimbriae then create currents in the peritoneal fluid that act to carry the oocyte into the uterine tube
Female Duct System
The ampulla ends in the infundibulum, an open, structure bearing ciliated projections called fimbriae that drape over the ovary
Female Duct System
The uterine tube aids the process of an oocyte
Its wall contains sheets of smooth muscle, and its thick, highly folded mucosa contain both ciliated and nonciliated cells
The oocyte is carried toward the uterus by a combination of muscular peristalsis and the beating of the cilia
Female Duct System
Nonciliated cells of the mucosa have dense microvilli and produce a secretion that keeps the oocyte (and sperm, if present) moist and nourished
Female Duct System
Externally, the uterine tubes are covered by visceral peritoneum and supported along their length by a short mesentary
Female Duct System
The mesentary is called the mesosalpinx, a reference to the trumpet shaped uterine tube it supports
Female Uterus
The uterus is located in the pelvis, anterior to the rectum and posterosuperior to the bladder
The Uterus
The uterus is a hollow, thick walled organ that functions to receive, retain, and nourish the ovum
The Uterus
In a pre-menopausal woman who has never been pregnant, the uterus is about the size and shape of an inverted pear
It is usually somewhat larger in woman who have borne children
The Uterus
Normally, the uterus is fixed anteriorly where it joins the vagina, causing the uterus as a whole to be inclined forward or anteverted
However, the uterus is often turned backward, or retroverted in older woman
The Uterus
The Uterus
The main portion of the uterus is referred to as the body
The Uterus
The rounded region superior to the entrance of the uterine tubes is the fundus, and the slightly narrowed region is the isthmus
The Uterus
The cervix of the uterus is its narrow neck, or outlet, which projects into the vagina inferiorly
The Uterus
The cavity of the cervix, called the cervical canal, communicates with the vagina via the external os
The Uterus
The internal os opens into uterine body
The Uterus
The mucosa of the cervical canal contains cervical glands that secrete a mucus that fills the cervical canal and covers the external os, presumably to block the spread of bacteria from the vagina into the uterus
Cervical mucus also blocks the entry of sperm, except at midcycle, when it becomes less viscous and allows sperm to pass through
Uterus: Homeostatic Imbalance
Cancer of the cervix is common among woman between ages of 30 and 50
Risk factors include frequent cervical inflammations, sexually transmitted diseases including genital warts, and multiple pregnancies
The cancer cells arise from the epithelium covering the cervical tip
Uterus: Homeostatic Imbalance
In a Papanicolaou (Pap) smear, or cervical smear test, some of these epithelial cells are scraped away and then examined for abnormalities
A Pap smear is the most effective way to detect this slow-growing cancer
Woman are advised to have a Pap smear every year
Supports of the Uterus
The uterus is supported laterally by the mesometrium portion of the broad ligament
Supports of the Uterus
Inferiorly, the lateral cervical (cardinal) ligaments extend from the cervix and superior part of the vagina to the lateral walls of the pelvis
Supports of the Uterus
The paired uterosacral ligaments secure the uterus to the sacrum posteriorly
Supports of the Uterus
The uterus is bound to the anterior wall by the fibrous round ligament, which runs through the inquinal canals to anchor in subcutaneous tissue
Supports of the Uterus
These various ligaments allow the uterus a good deal of mobility, and its position changes as the rectum and bladder fill and empty
Uterus: Homeostatic Imbalance
Despite the many anchoring ligaments, the principle support of the uterus is provided by muscles of the pelvic floor, namely the muscles of the urogenital and pelvic diaphragms
Uterus: Homeostatic Imbalance
These muscles are sometimes torn during childbirth
Subsequently, the unsupported uterus may sink inferiorly, until the tip of the cervix protrudes through the vaginal opening
Uterus: Homeostatic Imbalance
When the tip of the uterus extends trhough the external vaginal opening the condition is called a prolapse of the uterus
The Uterus
The undulating course of the peritoneum around and over the various pelvic structures produces several blind ended peritoneal pouches
The Uterus
The most important of these pouches are the vesicouterine pouch between the bladder and the uterus
The Uterus
The rectouterine pouch lies between the rectum and the uterus
The Uterine Wall
The wall of the uterus is composed of three layers; the perimetrium, myometrium and endometrium
The Uterine Wall
The wall of the uterus
– The perimetrium is the outermost serous layer composed of visceral peritoneum
– The myometrium is the bulky middle layer, composed of interlacing bundles of smooth muscle. It is the myometrium that contracts during childbirth to expel the baby
– The endometrium is a simple columnar epithelium underlain by a thick lamina propria of highly cellular connective tissue
The Uterine Wall
If fertilization occurs, the young embryo burrows (implants) into the endometrium and resides there for the rest of development
The Uterine Wall
The endometrium has two chief strata
– The stratum functionalis (functional layer) undergoes cyclic changes in response to blood levels of ovarian hormones and is shed during menstruation (approx. 28 day cycle)
– The stratum basale is the thinner deeper layer which forms a new functionalis layer after menstruation ends
• It is unresponsive to ovarian hormones
The endometrium has numerous uterine glands that changes with the endometrium
The Uterine Wall
To understand the cyclic changes of the uterine endometrium it is essential to understand the vascular supply of the uterus
The uterine arteries arise from the internal iliacs in the pelvis, ascend along the sides of the uterus and send branches into the uterine walls
The Uterine Wall
The uterine arteries break up into several arcuate arteries within the myometrium
The Uterine Wall
The arcuate arteries send radial branches into the endometrium, where they in turn give off straight arteries to the stratum basalis and spiral arteries to the stratum functionalis
The Uterine Wall
The spiral arteries undergo repeated degeneration and regeneration, and it is their spasms that actually cause the functionalis layer to be shed during menstruation
Veins in the endometrium are thin-walled and form an extensive network with occasional sinusoidal enlargements
The Vagina
The vagina is a thin-walled tube
8-10 cm / 3-4 in. long
It lies between the bladder and the rectum and extends from the cervix to the exterior of the body
The Vagina
The urethra is embedded in its anterior wall
Often called the birth canal, the vagina provides a passageway for delivery of an infant or for menstrual flow urethra
The Vagina
The vagina receives the penis (and semen) during sexual intercourse
It is the female organ of copulation
The highly distensible walls of the vagina consists of three tunics
– Adventitia
– Muscularis
– Mucosa
The Vagina
The adventitia is made of fibrous and elastic connective tissue
The muscularis is smooth muscle
The mucosa is epithelium
– The mucosa is marked by transverse ridges or rugae, which stimulate the penis during intercourse
– The mucosa is stratified squamous epithelium which is resistent to friction
The Vagina
Certain mucosal cells (dendritic cells) act as antigen-presenting cells and are thought to provide the route of HIV transmission from an infected male to the female during sexual intercourse
The Vagina
The vaginal mucosa has no glands; it is lubricated by the cervical mucus glands
Its epithelial cells release large amounts of glycogen, which is anaerobically metabolized to lactic acid by resident bacteria
Consequently, the pH of a woman’s vagina is normally quite acidic
The Vagina
Acidity in the vagina helps to keep it healthy and free of infection, but it is also hostile to sperm
Although vaginal fluid of adult females is acidic, it tends to be alkaline in adolescents, predisposing sexually active teenagers to sexually transmitted diseases
The Vagina
The vaginal orifice forms an incomplete partition called the hymen
The hymen is quite vascular and tends to bleed during first coitus
The Vagina
The durability of the hymen varies
In some females it is ruptured during sports, tampon insertion or pelvic exam
Some individuals may need to be breached surgically
The Vagina
The upper end of the vaginal canal loosely surrounds the cervix of the uterus, producing a vaginal recess called the vaginal fornix
The Vagina
The posterior part of this recess, the posterior fornix, is much deeper than the lateral and anterior fornices
The Vagina
Generally, the lumen of the vagina is quite small and, except where it is held open by the cervix, its posterior and anterior wall are in contact with one another
The Vagina
The vagina stretches considerably during copulation and childbirth
Its lateral distension is limited by ishial spines and ligaments
The External Genitalia
The external genitalia also called the vulva include
– Mons pubis
– Labia
– Clitoris
– Vestibule structures
The External Genitalia
The mons pubis is a fatty, rounded area overlying the pubic symphysis
After puberty this area is covered with pubic hair
The External Genitalia
Running posteriorly from the mons pubis are two elongated, hair covered, fatty skin folds the labia majora
These are the female counterpart of the male scrotum
The External Genitalia
The labia majora enclose the labia minora two thin, hair free skin folds, homologous to the ventral penis
The External Genitalia
The labia minora enclose a recess called the vestibule, which contains the external opening of the urethra more anteriorly followed by that of the vagina
The External Genitalia
Flanking the vaginal opening are the pea sized greater vestibular glands which are homologous to the bulbourethral glands of males
The External Genitalia
These glands release mucus into the vestibule to keep it moist and lubricated, facilitating intercourse
The External Genitalia
Just anterior to the vestibule is the clitoris
This small protruding structure, composed of erectile tissue that is homologous to the penis of the male
The External Genitalia
It is hooded by a skin fold called the prepuce of the clitoris, formed by the junction of the labia minora folds
The External Genitalia
The clitoris is richly innervated with sensory nerve endings sensitive to touch, and it becomes swollen with blood and erect during tactile stimulation, contributing to a female’s sexual arousal
Like the penis, the clitoris has dorsal erectile columns (corpora cavernosa) but it lacks corpus spongiosum
The External Genitalia
In males, the urethra carries both urine and semen and runs through the penis
In females, the urinary and reproductive tracts are completely separate, and neither runs through the clitoris
The External Genitalia
The female perineum is a diamond shaped region located between the pubic arch anteriorly, coccyx posteriorly, and the ishial tuberosities laterally
The External Genitalia
The soft tissues of the perineum overlie the muscles of the pelvic outlet and the posterior ends of the labia majora overlie the central tendon, into which most floor muscles insert
The Mammary Glands
The mammary glands are present in both sexes, but they normally only function in females
The Mammary Glands
Since the biological role of the mammary glands is to produce milk to nourish a newborn baby, they are actually important only when reproduction has already been accomplished
Developmentally, mammary glands are modified sweat glands that are really part of the skin, or integumentary system
The Mammary Glands
Each mammary gland is contained within a rounded skincovered breast anterior to the pectoral muscles of the thorax
The Mammary Glands
Slightly below the center of each breast is a ring of pigmented skin, the areola, which surrounds the central protruding nipple
The Mammary Glands
Large sebaceous glands in the areola make it bumpy and produce sebum that reduces chapping and cracking of the skin of the nipple
The Mammary Glands
Autonomic nervous system controls of smooth muscle fibers in the areolar and nipple cause the nipple to become erect when stimulated by contact or sexual stimuli and when exposed to the cold
The Mammary Glands
Internally, each mammary gland consists of 15 to
25 lobes that radiate around and open at the nipple
The lobes are separated by fat and fibrous connective tissue
The Mammary Glands
The interlobar connective tissue forms suspensory ligaments that attach the breast to the underlying muscle fascia and to the overlying dermis
The Mammary Glands
The suspensory ligaments provide natural support for the breasts
Within the lobes are smaller units called lobules which contain glandular alveoli that produce milk when lactating
The Mammary Glands
These compound alveolar glands pass milk into the lactiferous ducts, which open to the outside at the nipple
The Mammary Glands
Just deep to the areola, each lactiferous duct has a dilated region called a lactiferous sinus
Milk accumulates in these sinuses during nursing
The Mammary Glands
The discussion of the mammary glands given here applies only to nursing women or women in the last trimester of pregnancy
In nonpregnant woman, the glandular structure of the breast is largely undeveloped and the duct system is rudimentary
Breast size is largely due to the amount of fat deposits
Breast Cancer
Invasive breast cancer, the most common malignancy of U.S. women, strikes nearly
200,000 American women each year
One woman in eight develop this condition
Breast cancer usually arises from the epithelial cells of the ducts, not from the alveoli
A small cluster of cancer cells grows into a lump in the breast from which cells eventually metastasize
Breast Cancer
Known risk factors for developing breast cancer include
– Early onset menses and late menopause
– No pregnancies or first pregnancy late in life
– Previous history of breast cancer
– Family history of breast cancer (especially in a sister or mother)
– Other risk factors are also proposed
Breast Cancer
Breast cancer is often signaled by a change in skin texture, puckering, or leakage from the nipple
Early detection by breast self-examination and mammography is the best way to increase one’s chances of surviving breast cancer
Since most breast lumps are discovered by women themselves in routine monthly breast exams this should be a priority
Breast Cancer
Once diagnosed, breast cancer is treated in various ways on specific characteristics of the lesion
Current therapies include
– Radiation therapy
– Chemotherapy
– Surgery, often followed by radiation or chemotherapy
• Radial mastectomy
• Lumpectomy
• Simple mastectomy
Breast Cancer
Many mastectomy patients opt for breast reconstruction to replace excised tissue
Physiology: Female System
Gamete production in males begins at puberty and continues throughout life, but the situation is quite different in females
A female’s total supply of eggs is already determined by the time she is born, and the time span during which she releases them extends from puberty to menopause
(about age 50)
Physiology: Female System
Meiosis, the specialized nuclear division that occurs in the testes to produce sperm, also occurs in the ovaries
In this case, female sex cells are produced, and the process is called oogenesis
The process of oogenesis takes years to complete
Flowchart of Events of Oogenesis
Physiology: Female System
In the fetal period the oogonia, the diploid stem cells of the ovaries, multiply rapidly by mitosis and then enter a growth phase and lay in nutrient reserves
Physiology: Female System
Gradually, primordial follicles begin to appear as the oogonia are transformed into primary oocytes and become surrounded by a single layer of follicle cells
Physiology: Female System
The primary oocytes begin the first meiotic division, but become “stalled” late in prophase I and do not complete it
Physiology: Female System
By birth, a female’s lifetime supply of primary oocytes, approximately 2 million of them, is already in place in the cortical region of the immature ovary
Since they remain in their state of suspended animation all through childhood, the wait is a long one - 10 to 14 years at the very least
Physiology: Female System
At puberty, perhaps 400,000 oocytes remain and beginning at this time a small number of primary oocytes are selected and activated each month
Physiology: Female System
However, only one oocytes is selected each month to continue meiosis I ultimately producing two haploid cells (23 replicated chromosomes) that are quite dissimilar in size
Physiology: Female System
The smaller cell is called the first polar body
The larger cell, which contains nearly all the cytoplasm of the primary oocyte is the secondary oocyte
Physiology: Female System
A spindle forms at the very edge of the oocyte and a little “nipple” into which the polar chromosomes will be cast appears at the edge
Physiology: Female System
This sets up the polarity of the oocyte and ensures that the polar body receives almost no cytoplasm or organelles
Physiology: Female System
The first polar body may continue its development and undergo meiosis II producing two even smaller polar bodies
Physiology: Female System
In humans, the secondary oocyte arrests in metaphase II and it is this cell (not a functional ovum) that is ovulated
Physiology: Female System
If an ovulated secondary oocyte is not penetrated by a sperm, it simply deteriorates
Physiology: Female System
If an ovulated secondary oocyte is penetrated by sperm, it quickly completes meiosis
II, yielding one large ovum and a tiny second polar body
Physiology: Female System
The potential end products of oogenesis are three tiny polar bodies nearly devoid of cytoplasm, and one large ovum
All of these cells are haploid, but only the ovum is a functional gamete
This is quite different from spermatogenisis, where the product is four viable gametes - spermatozoa
Physiology: Female System
The unequal cytoplasmic divisions that occur during oogenesis ensure that a fertilized egg has ample nutrients for its seven day journey to the uterus
Without nutrient containing cytoplasm the polar bodies degenerate and die
Since the reproductive life of a female is at best 40 years (11 to 51) and typically only one ovulation occurs each month, fewer than 500 oocytes are ever released
The Ovarian Cycle
The monthly series of events associated with the maturation of an egg is called the ovarian cycle
The ovarian cycle is best described in terms of two consecutive phases
– The follicular phase is the period of follicle growth, typically indicated as lasting from the first to the fourteenth day of the cycle
– The luteal phase is the period of corpus luteum activity, days 14-28
The Ovarian Cycle
The typical ovarian cycle repeats at intervals of 28 days, with ovulation occurring midcycle
However, cycles as long as 40 days or as short as 21 days are fairly common
In such cases, the length of follicular phase and timing of ovulation vary, but the luteal phase remains constant: It is 14 days between the time of ovulation and the end of the cycle
The Ovarian Cycle
Hormonal controls of these events will be described later
The next section will focus upon what happens each month within the ovary
The Follicular Phase
Maturation of a primordial follicle to the mature state occupies the first half of the cycle and involves several events
The Ovarian Cycle
1) Primordial follicles surrounded by squamous like cells
The Ovarian Cycle
21) The squamous like cells surrounding the primary oocyte grow becoming cuboidal cells, and the oocyte enlarges
The Ovarian Cycle
3) Next the follicular cells proliferate until they form a stratified epithelium around the oocyte
As soon as more than one cell layer is present, the follicle is called a granulosa cell
The Ovarian Cycle
The granulosa cells are connected to the developing oocyte by gap junctions, through which ions, metabolites, and signaling molecules can pass
One of the signals passing from the granulosa cells to the oocytes initiates cell growth
The Ovarian Cycle
4) A layer of connective tissue begins to condense around the follicle, forming the theca folliculi
The Ovarian Cycle
As the granulosa cells continue to divide and the follicle grows, the thecal and granulosa cells cooperate to produce estrogens (the inner thecal cells produce androgens, which the granulosa cells convert to estrogens)
At the same time, the granulosa cells secrete a glycoprotein-rich substance that forms a thick transparent membrane, called the zona pellucida around the oocyte
The Ovarian Cycle
5) Clear liquid accumulates between the granulosa cells and eventually coalesces to form a fluid filled cavity, the antrum
The presence of an atrium distinguishes the new secondary follicle from the primary
The Ovarian Cycle
The antrum continues to expand with fluid until it isolates the oocyte, along with its surrounding capsule of granulosa cells called a corona radiata on a stalk on one side of the follicle
When a follicle attains full size (2.5 cm) it becomes a vesticular follicle
The Ovarian Cycle
6) The vesticular follicle bulges from the external ovarian surface
This usually occurs by day
14
The Ovarian Cycle
As one of the final events of follicle maturation, the primary oocyte completes meiosis I to form the secondary oocyte and first polar body
Once this has occurred, the stage is set for ovulation
At this point, the granulosa cells send another important signal to the oocyte, in effect holding the meiosis of the oocyte
The Ovarian Cycle
7) Ovulation occurs when the ballooning ovary wall ruptures and expels the secondary oocyte into the peritoneal cavity
The Ovarian Cycle
Some women experience a twinge of pain in the lower abdomen when ovulation occurs
This episode is caused by the intense stretching of the ovarian wall during ovulation
The Ovarian Cycle
In the ovaries of adult females, there are always several follicles at different stages of maturation
As a rule, one follicle outstrips the others to become the dominant follicle and is at the peak stage of maturation when the hormonal (LH) stimulus is given for ovulation
The Ovarian Cycle
How this follicle is selected, or selects itself, is still uncertain, but it is probably the one that attains the greatest FSH sensitivity the quickest
The others degenerate
The Ovarian Cycle
In 1-2% of all ovulations, more than one oocyte is ovulated
This phenomenon, which increases with age, can result in multiple births
Since different oocytes are fertilized by different sperm, the siblings are fraternal or nonidentical twins
Identical twins result from the fertilization of a single oocyte by a single sperm, followed by separation of daughter cells
The Ovarian Cycle
8) After ovulation, the ruptured follicle collapses, and the antrum fills with clotted blood
The Ovarian Cycle
This corpus hemorrhagicum is eventually absorbed
The remaining granulosa cells increase in size and along with the internal thecal cells they form a new, quite different endocrine gland, the corpus luteum
Once formed, the corpus luteum begins to secrete progesterone and some estrogen
The Ovarian Cycle
If pregnancy does not occur, the corpus luteum starts degenerating in about 10 days and its hormonal output ends
In this case all that ultimately remains is a scar called the corpus albicans (white body)
The Ovarian Cycle
9) If the oocyte is fertilized and pregnancy ensures, the corpus luteum persists until the placenta is ready to take over hormone production
The placenta is ready to assume these duties at about three months
Hormones and the Ovarian Cycle
Ovarian events are much more complicated than those occurring in the testes, but the hormonal controls set into motion at puberty are similar in the two sexes
Gonadotropin-releasing hormone (GnRH), the pituitary gonadotropins, and, in this case ovarian estrogen and progesterone interact to produce the cyclic events occurring in the ovaries
Establishing the Ovarian Cycle
During childhood, the ovaries grow and continuously secrete small amounts of estrogens which inhibit hypothalmic release of GnRH
But as puberty nears, the hypothalamus becomes less sensitive to estrogen and begins to release GnRH in a rhythmic pulselike manner
GnRH, in turn, stimulates the anterior pituitary to release FSH and LH which act on the ovaries
Establishing the Ovarian Cycle
Gonadotropin levels continue to increase for about four years and, during this time, pubertal girls are still not ovulating and thus are incapable of getting pregnant
Eventually, the adult cyclic pattern is achieved, and hormonal interactions stabilize
Establishing the Ovarian Cycle
These events are heralded by the young woman’s first menstrual period, referred to as menarche
Usually, it is not until the third year postmenarche that the cycles become regular and all are ovulatory
Hormones: Ovarian Cycle
Described at the right is the cycle of anterior pituitary gonadatropins
(FSH & LH) and ovarian hormones, and their negative and positive feedback mechanisms
Hormones: Ovarian Cycle
1) On day 1 of the cycle, rising levels of GnRH from the hypothalamus stimulate increased production and release of FSH and LH by the anterior pituitary
Hormones: Ovarian Cycle
2) FSH and LH stimulate follicle growth and maturation and estrogen secretion
FSH exerts its main effects on the follicle cells,
Whereas LH targets the thecal cells
Hormones: Ovarian Cycle
Why only some follicles respond to these hormonal stimuli is still a mystery
However, there is little doubt that enhanced responsiveness is due to formation of more gonadotropin receptors
As the follicles enlarge, estrogen secretion begins
Hormones: Ovarian Cycle
LH prods the thecal cells to produce androgens
These diffuse through the basement membrane, where they are converted to estrogens by the FSH-primed granulosa cells
Only tiny amounts of ovarian andogens enter the blood, because they are almost completely converted to estrogens within the ovaries
Hormones: Ovarian Cycle
3) The rising estrogen levels in the plasma exert negative feed-back on the pituitary, inhibiting its release of FSH and
LH while prodding it to synthesize and accumulate gonadotropins
Hormones: Ovarian Cycle
Within the ovary, estrogen increases output by intensifying the effect of FSH on follicle maturation
Inhibin, released by the granulosa cells, also exerts negative feedback controls on
FSH release during this period
Hormones: Ovarian Cycle
4) The initial small rise in estrogen blood levels inhibits the hypothalamicpituitary axis as just described, but high estrogen levels have the opposite effect
Hormones: Ovarian Cycle
Once estrogen reaches a critical concentration in the blood, it exerts positive feedback on the brain and anterior pituitary
Hormones: Ovarian Cycle
5) High estrogen levels set a cascade of events into motion
There is a sudden burstlike release of accumulated
LH (FSH to a lesser extent) by the anterior pituitary
Occurs midcycle
Hormones: Ovarian Cycle
6) The sudden flush of LH stimulates the primary oocyte of the dominant follicle to complete the first meiotic division
The secondary oocyte continues on to metaphase
II
Hormones: Ovarian Cycle
LH also triggers ovulation at or around the day 14
Perhaps LH induces the synthesis of proteolytic enzymes too, but whatever the mechanism, the blood stops flowing through the protruding part of the follicle wall
Within 5 minutes, that region of the follicle wall bulges out, thins, and then abruptly ruptures
Hormones: Ovarian Cycle
The role (if any) of FSH in this process is unknown
Shortly after ovulation, estrogen levels decline
This probably reflects the damage to the dominant estrogen secreting follicle during ovulation
Hormones: Ovarian Cycle
7) The LH surge also transforms the ruptured follicle into a corpus luteum
(hence the name luteinizing hormone)
Hormones: Ovarian Cycle
Almost immediately after the corpus luteum is formed, this newly formed endocrine gland begins to produce progesterone and estrogen
Hormones: Ovarian Cycle
8) As progesterone and estrogen levels rise in the blood, the combination exerts a powerful negative feedback effect on anterior pituitary release of LH and FSH
Hormones: Ovarian Cycle
Corpus luteum release of inhibin enhances this inhibitory effect
With gonadotropin decline, the development of new follicles is inhibited, and additional LH surges that might cause additional oocytes to be ovulated are prevented
Hormones: Ovarian Cycle
9) As LH blood levels decline, the stimulus for luteal activity ends, and the corpus luteum begins degenerating
Hormones: Ovarian Cycle
As the corpus luteum, so go the level of ovarian hormones, and blood estrogen and progesterone levels drop sharply
However, if implantation of an embryo has occurred, the activity of the corpus luteum is maintained by an LH-like hormone released by the developing embyro
Hormones: Ovarian Cycle
10) A marked decline in ovarian hormones at the end of the cycle
(26-28) ends their blockade of FSH and LH secretion, and the cylce starts anew
The Uterine (Menstrual) Cycle
Although the uterus is where the young embryo implants and develops, it is receptive to implantation only for a very short period each month
Not surprisingly, this brief interval is exactly the time when a developing embryo would normally begin implanting, about seven days after ovulation
The Uterine (Menstrual) Cycle
The uterine or menstrual cycle is a series of cyclic changes that the uterine endometrium goes through each month as it responds to changing levels of ovarian hormones in the blood
These endometrial changes are coordinated with the phases of the ovarian cycle, which in turn are dictated by gonadotropins released by the anterior pituitary
The Uterine (Menstrual) Cycle
Days 1 - 5 Mentrrual phase
In this phase, the uterus sheds all but the deepest part of its endometrium
– At the beginning of this stage, gonadotropins are beginning to rise a bit and ovarian hormones are at their lowest normal levels. Then FSH levels begin to rise
The thick functional layer of the endometrium detaches from the uterine wall, a process that is accompanied by bleeding for 3-5 days
The Uterine (Menstrual) Cycle
The detached tissue and blood pass out through the vagina as the menstrual flow
By day 5, the growing ovarian follicles are starting to produce more estrogen
Notice day 5 on the chart at right
The Uterine (Menstrual) Cycle
Days 6-14: Proliferative phase
In this phase the endometrium rebuilds itself
Under the influence of rising blood levels of estrogen, the basal layer of the endometrium generates a new functional layer
The Uterine (Menstrual) Cycle
As the new functional layer thickens, its glands enlarge and its spiral arteries increase in number
The Uterine (Menstrual) Cycle
Consequently, the endometrium once again becomes velvety, thick, and well vascularized
During this phase, estrogens also induce synthesis of progesterone receptors in the endometrial cells readying them for interaction with progesterone
The Uterine (Menstrual) Cycle
Normally, the cervical mucus is thick and sticky, but rising estrogen levels cause it to thin and become crystalline, forming channels that facilitate the passage of sperm into the uterus
Ovulation occurs in the ovary at the end of this stage (day 14) in response to the sudden release of LH from the anterior pituitary
LH converts the follicle to a corpus luteum
The Uterine (Menstrual) Cycle
Days 15-28: Secretory Phase
In this phase, the endometrium prepares for implantation of the embryo
Rising levels of progesterone from the corpus luteum act on the estrogen-primed endometrium causing the spiral arteries to elaborate and coil more tightly and converting the functional layer to a secretory mucus
The Uterine (Menstrual) Cycle
The uterine glands enlarge, coil, and begin secreting nutritious glycoproteins into the uterine cavity
These nutrients sustain the embryo until it has implanted in the blood-rich endometrial lining
All events of the secretory phase are promoted by progesterone
The Uterine (Menstrual) Cycle
Increasing progesterone levels also cause the cervical mucus to become viscous again, forming the cervical plug, which blocks sperm entry and plays an important role in keeping the uterus
“private” in the event an embryo has begun to implant
Rising progesterone (and estrogen) levels inhibit LH release by the anterior pituitary
The Uterine (Menstrual) Cycle
If fertilization has not occurred, the corpus luteum begins to degenerate toward the end of the secretory phase as
LH blood levels decline
Progesterone levels fall, depriving the endometrium of hormonal support, and the spiral arteries kink and go into spasms
The Uterine (Menstrual) Cycle
Denied oxygen and nutrients, the endometrial cells begin to die, and as their lysosomes rupture, the functional layer begins to self-digest, setting the stage for menstruation to begin on day 28
The spiral arteries arteries constrict one final time and then suddenly relax and open wide
As blood gushes into the weakened capillary beds, they fragment
The Uterine (Menstrual) Cycle
Fragmentation continues causing the functional layer to slough off
The mentrual cycle starts again on this first day of menstrual flow
The Uterine (Menstrual) Cycle
Notice that the menstrual and proliferative phases overlap the follicular stage and ovulation in the ovarian cycle
The Uterine (Menstrual) Cycle
The uterine secretory phase corresponds to the ovarian luteal phase
The Uterine (Menstrual) Cycle
Extremely strenuous activity can delay menarche in girls and can disrupt the normal mentrual cycle in adult women, even causing amenorrhea or cessation of menses
Part of the problem appears to be that female athletes have little body fat, and fat deposits help convert adrenal androgens to estrogens
The Uterine (Menstrual) Cycle
In addition, hypothalamic controls are blocked in some way by severe physical regimens
These effects are usually totally reversible when the athletic training is discontinued, but a worrisome consequence of amenorrhea in young healthy adult women is that they suffer dramatic losses in bone mass normally seen only in old age
The Uterine (Menstrual) Cycle
Once estrogen levels drop and the menstrual cycle stops (regardless of cause), bone loss begins
Currently, female athletes are encouraged to increase their daily calcium intake to 1.5 g, roughly the amount in a quart of milk
Effects: Estrogen Progesterone
Estrogen is analogous to testosterone, the male steroid
As estrogen levels rise in puberty they…
– Promote oogenesis and follicle growth in the ovary
– Exert anabolic effects on the female reproductive tract
Consequently, the uterine tubes, uterus, and vagina grow larger and become functional - ready to support pregnancy
Effects: Estrogen Progesterone
The uterine tubes and uterus exhibit enhanced motility
The vaginal mucosa thickens
The external genitalia mature
Effects: Estrogen Progesterone
Estrogen supports the growth spurt at puberty that makes girls grow much more quickly than boys during ages of 12 and 13
This growth is short lived because rising estrogen levels also cause earlier closure of the epiphysis on long bones, and females reach their full height between the ages of 15 and 17 years of age while males continue to grow until 19 to 21
Effects: Estrogen Progesterone
The estrogen-induced secondary sex characteristics of females include:
– Growth of the breasts
– Increased deposits of subcutaneous fat, especially in the hips and breasts
– Widening and lightening of the pelvis
– Growth of axillary and pubic hair
– Several metabolic effects including
Effects: Estrogen Progesterone
The estrogen-induced secondary sex characteristics of females include:
– Several metabolic effects including:
• Maintaining low total blood cholesterol levels and
(and high HDL levels)
• Facilitating calcium uptake to help maintain bone density
Effects: Estrogen Progesterone
Progesterone works with estrogen to establish and then help regulate the uterine cycle and progesterone promotes changes in cervical mucus
Its other effects are exhibed largely during pregnancy, when it inhibits the motility of the uterus and takes up where estrogen leaves off in preparing the breasts for lactation
Effects: Estrogen Progesterone
It should be noted that the source of most estrogen and progesterone during pregnancy is from the placenta and not from the ovaries
Female Sexual Response
The female sexual response is similar to that of the males in most respects
During sexual excitement
– The clitoris, vaginal mucosa, and breasts engorge with blood
– The nipples erect
– Increased activity of the vestibular glands lubricates the vestibule and facilitates the entry of the penis
Female Sexual Response
These events, though more widespread, are analogous to the erection phase in men
Sexual excitement is promoted by touch and psychological stimuli and is mediated along the same autonomic pathways as in males
Female Sexual Response
The final phase of the female sexual response, orgasm, results in
– Muscle tension increases throughout the body
– Pulse rate and blood pressure rise
– The uterus begins to contract rhythmically
As in males, orgasm is accompanied by a sensation of intense pleasure followed by relaxation
Female Sexual Response
Orgasm in females is not followed by a refractory period
Consequently females may experience multiple orgasms during a single sexual experience
Female orgasm is not required for conception
Some women may never experience orgasm, yet are able to conceive and bear children
Sexually Transmitted Diseases
Sexually transmitted diseases (STD’s) or venereal disease are infectious diseases spread through sexual contact
The United States has the highest rates of infection among developed countries
Over 12 million people in the U.S., a quarter of them adolescents, get STD’s each year
Sexually Transmitted Diseases
STD’s are the single most important cause of reproductive disorders
STD’s that cause reproductive disorders are typically of a bacterial origin
– Gonorrhea
– Syphillis
– Chlamydia
In addition, genital herpes can pose a risk to a developing fetus
Sexually Transmitted Diseases
Finally, the long term health risks posed by unrecognized or untreated STD’s can cripple and kill both host parent and offspring
AIDS cripples the immune system also threatening life itself
The risks are real
Yahoo!!